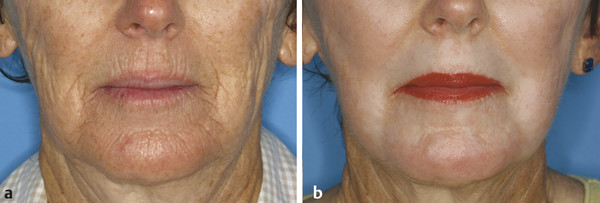
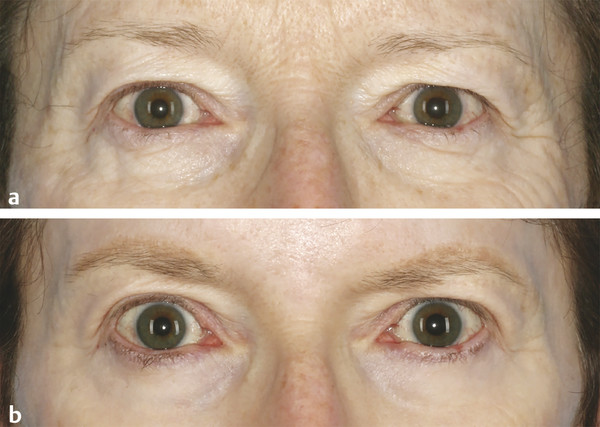
Background/History The mid-1990s saw the publication of several initial reports regarding early experience with 2,940-nm erbium:yttrium aluminum garnet (Er:YAG) laser skin resurfacing.1,2,3 The clinical allure of an alternative wavelength to the 10,600-nm carbon dioxide (CO2) skin resurfacing laser was in part related to the desire to improve skin tone and texture while minimizing collateral thermal effects. The first Er:YAG skin resurfacing devices were low-power, narrow pulse width lasers with clinically limiting tissue ablation efficiency and minimal tissue coagulation effect. As a result, per-pass tissue ablation depth was shallow and multiple passes were required to reach the papillary dermis.3 Whereas superficial dyschromia was greatly improved, the lack of a significant tissue coagulation effect resulted in bleeding upon reaching the papillary dermis and poor wrinkle effacement. The subsequent ability to modify the pulse duration (variable pulse vs. quasi-long pulse) and other energy delivery advances (e.g., optical multiplexing―see following text) with higher powered devices enabled laser surgeons to perform deeper treatments with less bleeding and improved rhytid reduction and tissue tightening. The convergence of wavelengths for the Er:YAG skin resurfacing laser with the peak for water absorption in the near infrared spectrum (both ~ 2,940 nm) enables the defining characteristic photomechanical tissue interaction of this device. Extremely rapid and efficient absorption of radiant energy from the 2,940-nm Er:YAG skin resurfacing laser causes near instantaneous conversion of light energy into mechanical energy as the affected layers of the skin are photodisrupted, ejected, and partially vaporized; very little tissue coagulation occurs with the short pulse Er:YAG skin resurfacing laser. By comparison, with far less efficient water absorption (2,940-nm Er:YAG ~ 16 times greater), the 10,600-nm CO2 skin resurfacing laser interacts with skin tissue primarily via a photothermal effect that creates extensive tissue coagulation and relatively less tissue ablation.4 Lengthening the pulse duration of the Er:YAG skin resurfacing laser through a series or train of subablative (laser fluence or energy below the threshold for maximum photomechanical effect and skin vaporization) pulses enabled laser surgeons to mimic the photothermal effect of the CO2 laser. This new feature became known as “dual mode” or “variable pulse mode,” wherein the Er:YAG laser was capable of delivering energy to the tissue via a short pulse (ablation) mode or a long pulse (coagulation) mode. Optical multiplexing―the use of a spinning mirror assembly to integrate the photon energy output of two separate laser heads operating in either ablate or coagulate modes―was another significant and necessary tissue delivery advance that allowed laser surgeons to effectively harness the power of the new dual mode (ablation, coagulation) Er:YAG laser skin resurfacing systems for maximum flexibility and speed in treatment.5 The ability to use either ablate or coagulate modes or both ablate and coagulate modes simultaneously while also controlling the depth of effect for each became known as “blending” or “tuning” the dual mode Er:YAG laser to meet specific treatment objectives. Skin rejuvenation, the primary indication for Er:YAG laser skin resurfacing, encompasses improvement of coarse, dull surface texture, reduction of dyschromia and photodamage, along with wrinkle effacement and improvement of scarring (▶ Fig. 6.1, ▶ Fig. 6.2, ▶ Fig. 6.3 and ▶ Fig. 6.4). Whereas traditional full-field, dual mode Er:YAG deep laser skin resurfacing is most often performed in Fitzpatrick skin types I, II, and possibly III, a more superficial full-field, ablate mode–only Er:YAG laser skin resurfacing treatment may be preferred in darker Fitzpatrick skin types (III, IV, and V). Deeper dual mode treatments have been associated with prolonged erythema (more than 4 months) and a relatively high rate (nearly 40%) of postinflammatory hyperpigmentation (PIH).6,7 Fig. 6.1 (a) Before and (b) 7 months after close-up photographs of perioral area following dual mode erbium:yttrium aluminum garnet (Er:YAG) laser skin resurfacing (66-year-old woman, Fitzpatrick skin type II, four passes at 50% overlap with ablate/coagulate settings 120/0, 100/50, 140/50, and 50/100). Note: near complete effacement of perioral lines and wrinkles. Fig. 6.2 (a) Before and (b) 7 months after left lateral photos following dual mode erbium:yttrium aluminum garnet (Er:YAG) laser skin resurfacing (66-year-old woman, Fitzpatrick skin type II, two passes on cheek areas at 50% overlap with ablate/coagulate settings 120/0 and 100/50). Note: effacement of rhytids, skin tightening, and increased contrast in skin tone between treated and untreated skin areas at jawline. Fig. 6.3 (a) Before and (b) 7 months after close-up images of periorbital area following dual mode erbium:yttrium aluminum garnet (Er:YAG) laser skin resurfacing (66-year-old woman, Fitzpatrick skin type II, three passes at 50% overlap with ablate/coagulate settings 80/0, 60/50, and 60/50). Note: effacement of rhytids and skin tightening of the upper and lower eyelids. Fig. 6.4 Composite of six separate left oblique photographs documenting progression of erythema following dual mode erbium:yttrium aluminum garnet (Er:YAG) laser skin resurfacing (66-year-old woman, Fitzpatrick skin type II). (a) Before; (b) 7 days after; (c) 30 days after; (d) 60 days after; (e) 90 days after; (f) 210 days after. Note: persistent erythema 90 days following treatment and resulting moderate hypopigmentation at 210 days. Several split-face (side-by-side) studies comparing modulated Er:YAG and pulsed CO2 skin resurfacing lasers have determined that benefits from dual mode Er:YAG laser skin resurfacing of facial rhytids approach or match those of CO2 laser skin resurfacing (treatment outcomes evaluated included wrinkle improvement, skin tightening, and improvement in photoaging scores), when similar immediate posttreatment end points are reached clinically and histologically.8,9,10,11 Although similar clinical results may be achieved, tissue contraction may be mediated differently with heat-induced collagen tightening from the pulsed CO2 laser with its significantly deeper residual thermal damage (e.g., 200 µm vs. up to 50 µm) and with wound contracture secondary to tissue healing following treatment with the Er:YAG laser.12 Photodamage and superficial dyschromia may be effectively treated with a single-pass intraepidermal peel (e.g., 50-µm depth) using ablate-only mode; however, when desired, the entire epidermis may be removed and the upper dermis partially ablated with a single pass (e.g., up to 200-µm total depth in ablate-only mode) (Video 6.1). In addition to clinically evident improvement of skin tone, superficial or microablative (intraepidermal, i.e., basement membrane remains intact) Er:YAG laser skin peels have also been shown to increase dermal matrix remodeling and to increase collagen types I, III, and VII as well as newly synthesized collagen (e.g., procollagen I and III) and tropoelastin.13,14,15 Although microablative Er:YAG laser treatments (Video 6.2) initiate inflammatory and tissue regenerative responses that extend into the dermis and well beyond the depth of tissue injury, it appears that maintenance of these changes may require ongoing interval treatments with repeated stimulation of the skin. The advent of nonablative fractional resurfacing (NFR) and ablative fractional resurfacing (AFR) enabled thermal and/or mechanical microablative injury with related long-term structural change extending from the epidermis into the deep dermis (e.g., up to 1,000-µm depth) with just transient erythema (NFR) or limited downtime (AFR). Although effective for removal of actinic keratoses and for nonmelanoma skin cancer prophylaxis, full-field laser skin resurfacing is not superior to other common treatment approaches including topical 5-fluorouracil (5-FU) or trichloroacetic acid (TCA) peels.16 Various types of benign skin lesions (e.g., moles, seborrheic keratosis) may be effectively removed using a handpiece with a small spot (e.g., 2 mm) or point beam mode (Video 6.3). Skin layers covering deeper milia and small intradermal pseudocysts may be ablated, enabling mechanical extraction and/or laser ablation. In select cases large patulous pores or deep ice pick scars may be de-epithelialized and then allowed to close through cicatricial wound contracture or they may be closed with one or more small sutures. Whereas Er:YAG laser skin resurfacing has been employed for treatment of various types of scarring, newer approaches with NFR and AFR have become more prevalent and the de facto nonsurgical standard of care for these conditions. Pretreatment considerations for Er:YAG laser skin resurfacing include absolute and relative contraindications that may require avoidance, delay, or modification of the proposed treatment. Patients who are deemed appropriate candidates for laser skin resurfacing must indicate willingness to accept downtime and responsibility for wound care during healing, as well as possible sequelae and attendant risks of complications. Absolute contraindications for laser skin resurfacing include active skin infection (bacterial, viral), isotretinoin use in the past 12 months, impaired immune function, suspicious skin lesion or skin cancer in treatment area, melasma, and unrealistic expectations regarding laser skin resurfacing benefits and outcomes. Relative contraindications for laser skin resurfacing include collagen vascular disease, abnormal scarring, prior radiation therapy or deep burn in treatment area, diffuse hyperpigmentation, Koebnerizing skin conditions, inflammatory condition of skin, severe skin sensitivity, lower eyelid laxity, and prior lower eyelid surgery. Severe hyperpigmentation affecting the face, neck, and other areas of the body may lead to relative hypopigmentation of the treated skin with an unusually stark contrast between treated lower facial skin and untreated neck skin (▶ Fig. 6.2
6.2 Indications/Contraindications


![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








