Epidural Anesthesia
Rachel C. Steckelberg
Jean-Louis Horn
Sarah Madison
DEFINITION
Neuraxial anesthesia is a type of regional anesthesia technique in which anesthesia medication is injected into the tissue surrounding the nerve roots as they exit the spine (eg, epidural anesthesia) and/or directly into the cerebrospinal fluid (eg, spinal anesthesia or subarachnoid anesthesia).
Continuous epidural anesthesia is a neuraxial anesthetic technique that may be used for postoperative analgesia, surgical anesthesia, and obstetric analgesia.
Epidural anesthesia may be used to provide anesthesia at any level below the chin, either alone or in combination with general anesthesia.
Epidural anesthesia may be administered as a single injection or as a continuous infusion via a catheter.
The location of the epidural placement determines the distribution of analgesia. An epidural block may be performed at the cervical, thoracic, lumbar, or sacral (eg, caudal) levels.
A continuous infusion of local anesthesia and/or opioid pain medication may provide postoperative pain control for several days after surgery.
Motor block with an epidural may range from none to complete, depending on the choice of drug, concentration, dosage, and/or level of administration.
Epidural analgesia is often part of a multimodal regimen that also includes systemic medications.
ANATOMY
The epidural space surrounds the spinal meninges (eg, dura mater) and the spinal nerve roots as they course outward to become peripheral nerves. It also contains venous plexuses, lymphatics, and fat tissue.
Knowledge of surface anatomy landmarks is essential for safe and reliable epidural placement (Table 1).
Table 1 Anatomic Landmarks for Identifying Vertebral Levels for Epidural Injection
Anatomic Landmark
Features
C7
Vertebral prominence (most prominent spinous process in neck)
T3
Root of spine of scapula
T7
Inferior angle of scapula
L4
Line between iliac crests
S2
Line between posterior inferior iliac spines
Sacral hiatus
Depression or groove above or between gluteal clefts directly above the coccyx
In the cervical area, the most prominent spinous process is usually C7.
The inferior angle of the scapula can be used to estimate the level of the T7 spinous process with the arms located at the side.
The spinal cord terminates at level L1 in adults. The dural sac terminates at S2.
The body of L4 and/or the interspace between L4 and L5 spinous processes typically can be found by drawing a line between the highest points of both the iliac crests (Tuffier line).
The line connecting the posterior superior iliac spine (PSIS) crosses at the level of the S2 posterior foramina.
The sacral hiatus is located by palpating for a depression (eg, the sacral hiatus) just above or between the gluteal clefts and above the coccyx. This is the point of entry for caudal epidural blocks.
By counting up or down from these surface anatomy reference points, other spinal levels can be identified.
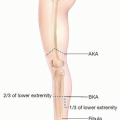
Epidural anesthesia may be performed at any level of the spinal cord. However, each epidural location (cervical, thoracic, and lumbar) has unique anatomic features (Table 2).
The angle of the spinous processes become progressively less angled closest to the base of the spine. For example, the spinous processes of the cervical and lumbar spine are more horizontal than the spinous processes in the thoracic spine, which are typically slanted in a more caudad direction and can overlap significantly. Thus, the technique for placement of the epidural needle varies considerably depending on the level selected.
The ideal location of epidural placement is at the same dermatome of the surgical incision.
Table 2 Anatomic Features of Cervical, Thoracic, and Lumbar Spine Regions | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
PATIENT HISTORY AND PHYSICAL FINDINGS
A preoperative history and physical must be performed prior to epidural placement. Particular attention should be paid to anesthetic history, preexisting neuropathies, history of bleeding diatheses, medication history (especially any use of blood thinning medications), medication allergies, a history of prior neuraxial anesthesia and/or spine surgery (including spinal fusion surgery), and any history of spine disorders (including spina bifida and/or scoliosis). If imaging of the spine is available and would be useful for epidural placement, it should be reviewed.
Physical exam should pay particular attention to any localized infections, masses, or other irregularities at the site of the planned epidural placement or surrounding areas.
Contraindications to epidural anesthesia include patient refusal, bleeding disorders, severe hypovolemia, elevated intracranial pressure, infection at the site of epidural needle placement, flow-limiting cardiac lesions such as mitral or aortic valve stenosis, and local spinal pathology.
IMAGING
When available, previous imaging of the spine should be reviewed, but routine imaging is not typically required prior to epidural placement.
NONOPERATIVE MANAGEMENT
The balance of risks and benefits must be considered for every interventional technique, including epidural anesthesia. Depending on a number of factors (including patient history, anatomy, surgery type, etc.), it may be more appropriate to employ alternative methods of analgesia, including peripheral nerve blocks and/or systemic medications for pain control.
Careful attention must be paid to the maximum dose of additional opioid or other local anesthetic medications used for pain control when an epidural is in place.
Nonopioid pain medications can also be useful adjuncts to epidural anesthesia/analgesia.
SURGICAL MANAGEMENT
Epidural anesthesia is indicated for postoperative analgesia of any surgical procedure below the level of the neck.
Thoracic epidurals are rarely used for primary surgical anesthesia, but more commonly for intraoperative and postoperative analgesia.
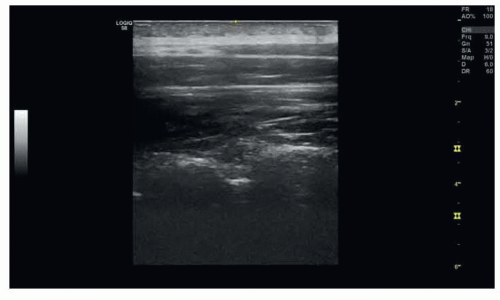
FIG 1 • Ultrasound of the lumbar and thoracic spine for epidural placement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access