CHAPTER 16 Endoscopic facial rejuvenation
History
Endoscopic facial rejuvenation is an approach that was started by the pioneering work on the forehead by Luis Vasconez and associates in the early 1990s.1 Many of us working independently and almost simultaneously developed our own methods to address the upper face.2–4 I had the privilege to perform the first ever recorded case of a complete endoscopic facelift that included the forehead, midface and neck,5 although a year earlier in April of 1992 at the First International Workshop on Facial Rejuvenation in Baltimore, Maryland, Oscar Ramirez and Robert Oneal telecasted live surgery demonstrations of two cases of endoscopic “assisted” open subperiosteal facelifts at the Johns Hopkins Hospital (video records). In the evolution of my own procedure, I also issued the first paper on the tridimensional approach to midface rejuvenation.6 A more extensive report followed in the years 2000 and 2001.3–8
Physical evaluation
The preoperative evaluation of my prospective patient follows this sequence.
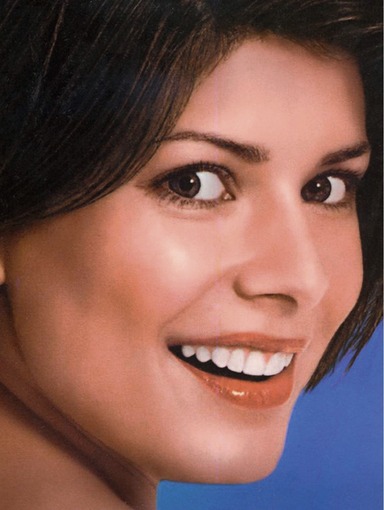
• I place the patient in a chair with two mirrors, each at 45 degrees for tridimensional evaluation of the face and observation of the digital maneuvers to be performed on the face. The two mirrors help to see the face from different angles including the lateral views.
• I assess the quality, texture and laxity of the skin and the amount of subcutaneous tissues and fat pads. I look for sun-damaged skin, areas of subcutaneous fat atrophy and for areas of fat accumulation.
• I assess the patient’s facial expression: position of the brows, lateral canthal area, laxity of the lower eyelid (snap test). Next, I check position of the corners of the mouth, sagging of the cheeks, and jowl formation.
• I evaluate the facial skeletal support: orbital rim support (upper and lower), malar bone prominence, pyriformis area, chin projection and height, gonial angle projection and height.
• I examine the neck from different angles: observation of excessive subcutaneous and/or subplatysma fat is critical. The digital maneuvers and visual observations for this might be deceiving and unreliable. Definite assessment of the location of fat accumulation may have to be postponed until the time of the surgery.
• I inspect to determine whether there is digastric bulge and/or salivary gland ptosis and/or enlargement.
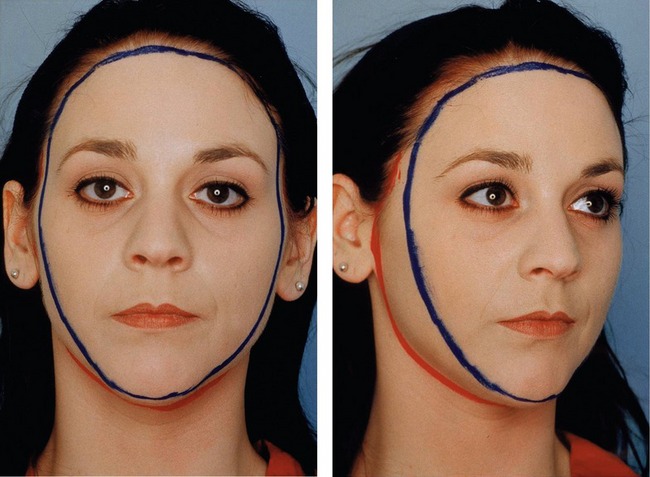
• I then perform digital maneuvers with lifting of the soft tissues of the brows, lateral canthal areas, lower eyelids, cheeks, corners of the mouth and jowls. I do these in a vertical or more oblique direction and I ask the patient which way they like the most. This will determine my vectors of pull during surgery. Generally, I lift the central oval of the face in a more vertical direction and the peripheral hemicircle in an oblique/horizontal direction. As the direction of the peripheral hemicircle changes from superior to inferior the vector of pull changes from oblique to horizontal. The more superior the structure, the more oblique the pull (e.g. temples). The more inferior the structure, the more horizontal the pull (jawline and neck) (Fig. 16.1). I compare and assess pulling and lifting versus anterior posterior projection. You can digitally pinch and imbricate the brows and cheeks; you can lift the mentum; you can pull the lax soft tissues in the directions indicated to see the desired changes.
• Digital elevation of the brow to the desired position will help you assess the need for concomitant upper eyelid blepharoplasty. Likewise, digital elevation of the cheek will determine how much skin can be safely removed from the lower eyelid.
• Examine the face in a three-quarter view. Observation from a true oblique position should allow visualization of both medial canthi. In this position, you can evaluate the reciprocal multicurvilinear line of beauty (“double ogee” line) of the face and the need to reconstruct this beautiful and youthful line.9
Anatomy
The central oval is where the ocular, nasal, and oral frames are located. Therefore, they are the most mobile and dynamic parts of the face. These are the areas where the facial mimetic muscles are located. The areas of transition between the central oval and peripheral hemicircle is where the motor branches of the facial nerve are most susceptible to injury. If surgical dissection continues from the superficial layers on the peripheral hemicircle to the intermediate layers of the central oval, more chances of nerve and muscle injury are likely (Fig. 16.2).
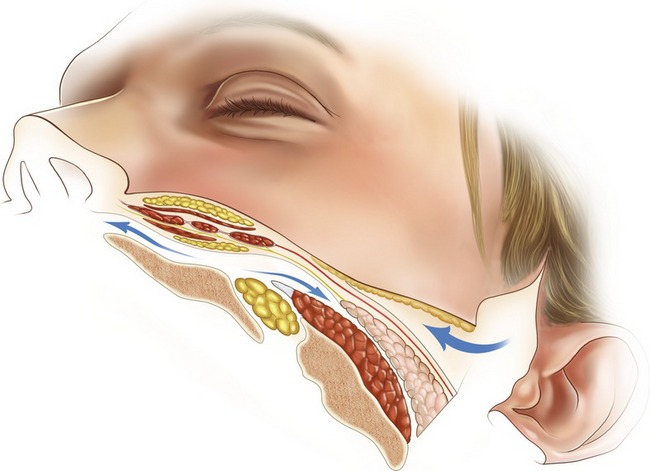
Fig. 16.2 Combination of subperiosteal dissection in the central oval with subcutaneous dissection in the peripheral hemicircle is the safest plane. Dissection coming from superficial in the peripheral hemicircle to deeper planes in the central oval poses a high risk of nerve and/or muscle injury.
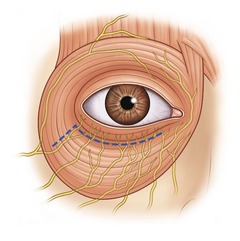
An important finding of our research is that the lower orbicularis oculi muscle is innervated by branches of the zygomatic and buccal nerves that penetrate the undersurface of this muscle, not from the lateral aspect as originally was presumed, but from the inferior border.10 Therefore, when cutting or separating the pretarsal portion from the preseptal muscle portions during routine lower blepharoplasty (the McIndoe operation), the pretarsal muscle is denervated (Fig. 16.3). The extent of denervation will depend on how aggressive is the separation medially. Limited separation will preserve some of the innervations. Likewise, lifting the innervated preseptal portion over or close to the denervated pretarsal portion during canthopexy or orbicularis oculi muscle suspension will favor a quicker neurotization.
Another important anatomical characteristic relevant to my technique is that the orbicularis oculi muscle is attached to the bony orbital rim. Better redraping and upper lifting of this muscle requires the detachment of this bony origin. The suborbicularis oculi fat (SOOF) is a fatty structure deep to the orbicularis oculi muscle. This is in continuity with another fatty structure that I call a “deep orbital malar fat” (DOMF). Both provide deep structural support to the orbit and midface. These fatty structures are rich in fibrous tissue. This fibroadipose character allows application of sutures for support and lifting. These deep fatty structures are not isolated from the more superficial fatty structures located over the mimetic muscles of the face. They are interconnected through the intermuscular spaces forming a network of soft tissue structural support in which the mimetic muscles, motor and sensory nerves, and vessels are located. It seems that atrophy of this deep fat is more important in the aging appearance of the older face. The superficial fat with a less fibrous component is more prone to sagging, forming the ptotic nasolabial folds and jowls that you see with aging.
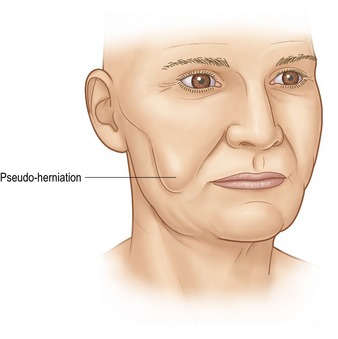
The eyelid fat pads and the buccal fat pad (Bichat’s) allow the gliding mechanism of the ocular motor muscles and the masticatory muscles respectively. They are also more prone to herniation because of the muscle activity of the related muscles and the lack of external support overlying these fat pads. They are also encased in a thin fascial pouch that allows gliding. This gliding also facilitates their expulsion from their original anatomical locations. This is clinically seen as a pseudo-herniation (Fig. 16.4). The Bichat’s fat pad is an important component of the upper jowl, located lateral to the oral commissure. Here forms the typical bulging of aging. Structurally some young individuals also have fullness in this area. Therefore excision or reposition of this structure helps improve the aesthetics of this portion of the face.
Another important anatomical and aesthetic configuration of the face is the presence of planes and curves. The face has multifaceting not unlike the faceting of the nose that has been previously described elsewhere. The most important curve of the face is seen in a three-quarter oblique view while both inner canthi are seen in this view. I call this the “reciprocal multicurvilinear line of beauty” or “double ogee” line.9 The single ogee of the cheek, also called “sigma,” has been previously described by William Little; however in my view the “double ogee” line is a more complete observation of the outline of the face (Fig. 16.5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 view. The presence of this line characterizes youth and beauty.
view. The presence of this line characterizes youth and beauty.





