|
|
|
Introduction
Nasolacrimal duct obstruction with symptomatic epiphora and associated mucoid discharge is the most common indication for dacryocystorhinostomy (DCR) ( Table 53.1 ). First described by Toti in 1904 as an external procedure, DCR has undergone several modifications throughout the years. While external DCR has been described as the “gold standard,” modern endonasal techniques approach the same success rate without a skin incision and more rapid recovery.
The decision to perform endoscopic DCR depends on several factors. The procedure requires different technical skills and proficiency compared to the external approach. The preoperative intranasal exam is useful to determine if a patient is a suitable candidate for endoscopic DCR. Septal deviations, masses, scarring and other nasal pathology should be identified preoperatively and a decision is made to proceed with an external versus endoscopic approach. Since general anesthesia is usually performed, some elderly patients may be more suited for the external approach under local anesthesia with sedation. Finally, if tumor is suspected, the external approach is preferred if possible dacryocystectomy is indicated.
Several preoperative and operative aspects must be considered ( Table 53.2 ). Achieving maximal hemostasis is vital for success of endoscopic DCR. Proper preparation begins in the holding area with inhaled oxymetazoline. Intraoperatively, intranasal packing should be placed immediately after induction of general anesthesia to allow for maximal absorption. The choice of vasoconstriction varies with surgeons and patient condition. Some surgeons still prefer 4% cocaine, but cardiac toxicity may preclude its use in high risk patients. Our preference is for cottonoids soaked in epinephrine at a concentration of 1 : 10,000. Other surgeons prefer oxymetazoline-soaked packing.
After prepping and draping, the packing is removed and the endoscope is inserted. Additional anesthetic consisting of 1% lidocaine with epinephrine 1 : 100,000 is injected submucosally in the region overlying the lacrimal sac. Packing with vasoconstriction is then replaced for 5 minutes to allow for additional hemostasis. Additional adjunct measures include placing the bed in reverse Trendelenburg and hypotensive anesthesia if the patient’s medical condition permits.
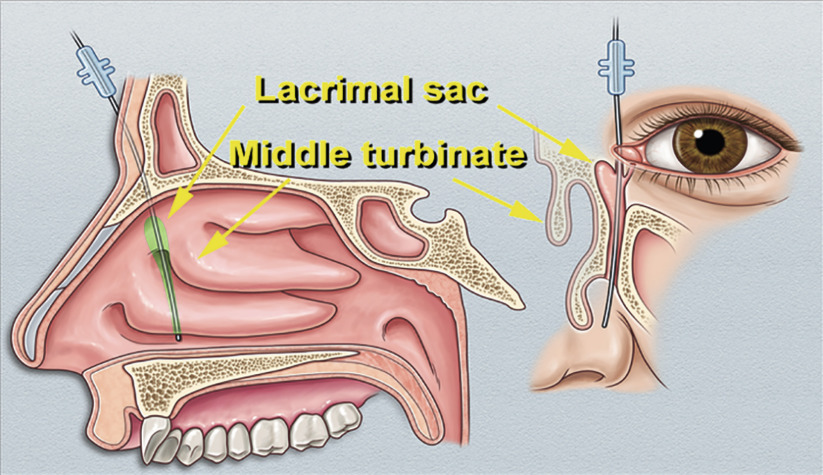
Knowledge of the anatomy of the lacrimal sac and its relation to the turbinates and lateral nasal wall is paramount. The lacrimal sac typically lies just anterior to the middle turbinate and the nasolacrimal duct courses slightly posteriorly and medially to open beneath the inferior turbinate. For nascent surgeons, localization of the lacrimal sac can be obtained by using a vitreoretinal light pipe or fracture of the lacrimal bone with a Bowman probe through the superior canaliculus; however, experienced surgeons may not find this to be necessary. The area of bone removal extends from the posterior lacrimal crest, anterior past the maxillary line to the anterior lacrimal crest of the maxilla. Superiorly it should not extend beyond the frontal bone due to proximity of the cribriform plate and the risk of cerebrospinal fluid leakage.
Numerous techniques of endonasal procedures have been described. All procedures have as the common goal the creation of a mucosally lined opening from the lacrimal sac to the nasal mucosa. This chapter and the following ( Chapter 54 , Chapter 55 , Chapter 56 , Chapter 57 , Chapter 58 ) demonstrate the different techniques for both primary and revision endoscopic DCR using various instrumentation for bony removal and adjuncts during the procedure. In this case and in Chapter 55 , primary endoscopic DCR is performed using Kerrison rongeurs. Chapter 54 demonstrates the use of an osteotome to facilitate bone removal. Some surgeons prefer intranasal flap creation with suturing and this is described in Chapter 57 . We routinely perform biopsy of the lacrimal sac in all cases of endoscopic DCR to rule out unsuspected pathology; however, this is not considered to be standard of care ( Chapter 55 ). The reader is encouraged to view each of these procedures to experience the variation in anatomy and technique.
Failure rate in DCR ranges between 5% and 10%. Re-operation may be necessary if the ostium is inadequate in size ( Chapter 56 ) or if there is common canalicular obstruction, where balloon dacryoplasty is indicated ( Chapter 58 ). Finally, conjunctivodacryocystorhinostomy with Jones tube may be considered as an ultimate option ( Chapter 59 ).