NATURAL HISTORY
■ Mastectomy offers potential cure in breast cancer patients and prevention for those at high risk for cancer. Immediate breast reconstruction offers an improvement in health-related quality of life and patient satisfaction for women choosing mastectomy as part of their treatment plan.1–3
PATIENT HISTORY AND PHYSICAL FINDINGS
■ Patient selection in immediate direct-to-implant breast reconstruction is one of the keys to success. A history is obtained to check for comorbidities that are known risk factors for increased complications including smoking, diabetes, body mass index (BMI), and previous breast radiation. On physical exam, the breast is assessed for skin quality, size, scars from previous procedures, symmetry, position of the IMF, and nipple position if a nipple-sparing mastectomy is being considered.
DIFFERENTIAL SURGICAL TREATMENT OPTIONS
■ Two-stage tissue expander–implant reconstruction
■ Autologous reconstruction using tissue from the body including the abdomen (TRAM, transverse rectus abdominis myocutaneous; DIEP, deep inferior epigastric perforator; SIEA [superficial inferior epigastric artery] flaps), buttocks (SGAP, superior gluteal artery perforator; IGAP [inferior gluteal artery perforator] flaps), thighs (TUG [transverse upper gracilis] flap), and back (latissimus dorsi)
■ Fat transfer
■ No, or delayed, reconstruction
NONOPERATIVE MANAGEMENT
■ Breast reconstruction is a choice, and patients undergoing mastectomy may not elect to pursue reconstruction. If no reconstruction is planned, the breast skin is closed and the chest remains flat in contour. If desired, external breast prostheses are available for women to wear in their clothing to give the appearance of a breast.
SURGICAL MANAGEMENT
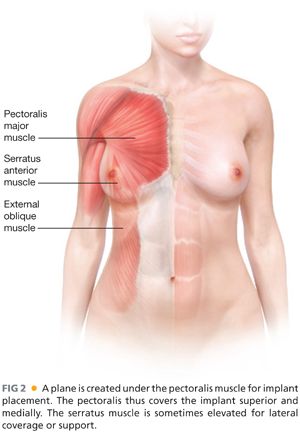
■ The goals of reconstruction are considered in determining if the reconstruction is designed to augment, reduce, or maintain the current breast size. In general, if a woman wants a significant increase in breast size, this is more safely done in two stages using a tissue expander followed by exchange to implant in a second surgery (see Chapter 15). For single-stage implant reconstruction, the implant is placed directly in a partial subpectoral pocket in order to allow superior soft tissue coverage with muscle in the cleavage area of the breast and to help prevent contracture around the implant.4 The implant is subcutaneous inferiorly, which allows a more natural teardrop shape, and is typically supported by a surgical acellular dermal matrix (ADM) or mesh. Currently, the most common ADM is AlloDerm (human dermis, LifeCell, Branchburg, NJ), but a variety of ADM or mesh material derived from human dermis, porcine dermis, bovine pericardium, fetal bovine dermis, silk, titanium, and Vicryl exist.
Preoperative Planning
■ With immediate implant reconstruction, a foreign body (implant) is placed into a skin envelope that has been partially devascularized with the mastectomy. Therefore, sterility is an important component of preoperative planning and operative management. The patient sits upright and is marked prior to the procedure. Important landmarks include the IMF position, its relation to the IMF on the contralateral breast, and the lateral border of the breast. The mastectomy portion of the procedure is performed first followed by the reconstruction.
Positioning
■ The patient is positioned supine with the arms secured on arm boards at the side, angled approximately 80 to 85 degrees from the operating table (FIG 3). This allows access to the axillary lymph nodes for sampling during the mastectomy. Both breasts are prepped and draped into the field.
Approach
■ The mastectomy and reconstruction may be performed using various incisions. If a nipple-sparing approach is chosen, the safest option is to use a radial lateral incision extending from the areola toward the axilla without a full-thickness incision around the nipple. The incision that maximizes cosmesis is an inferolateral or standard IMF incision under the breast.5 For skin-sparing mastectomies, the incision is made around the areola and extended laterally if needed for access. For larger breasts, a skin-reducing pattern is designed to remove excess skin in a vertical or horizontal direction. The inverted T/Wise/anchor skin pattern is typically avoided (secondary to higher risk of skin necrosis and complications). The pectoralis muscle is partially released inferiorly to accommodate the implant size and allow more natural breast shape. The challenge of direct-to-implant breast reconstruction is in replacement of the breast volume with an implant that closely matches the breast base diameter but without placing undue stress on the breast skin envelope. If this cannot be achieved in one stage, a two-stage approach is used with a tissue expander intermediary step.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








