Pemphigus foliaceus is an acquired autoimmune blistering disease in which the body’s immune system produces IgG autoantibodies that target the intercellular adhesion glycoprotein desmoglein-1, which is principally expressed in the granular layer of the epidermis, resulting in the loss of intercellular connections between keratinocytes (acantholysis) and the formation of subcorneal blisters within the epidermis. This article summarizes the epidemiology, clinical features, techniques for diagnosis, and drugs associated with treatment of this rare disease.
Pemphigus foliaceus (PF) is an acquired autoimmune blistering disease in which the body’s immune system produces IgG autoantibodies that target the intercellular adhesion glycoprotein desmoglein (dsg)-1. The binding of these autoantibodies to dsg-1, which is principally expressed in the granular layer of the epidermis, results in the loss of intercellular connections between keratinocytes (acantholysis) and the formation of subcorneal blisters within the epidermis. The ultimate clinical manifestations of this process are fragile, superficial blisters and bullae of the cutaneous surface that easily rupture to yield erosive lesions.
The pathogenic autoantibodies of PF are of the IgG4 subclass, which has been demonstrated by their passive transfer from human sera to neonatal mice. These IgG4 autoantibodies recognize antigenic epitopes located on the N-terminus of the ectodomain of dsg-1, specifically on extracellular domains 1 and 2. The binding of pathogenic IgG to dsg-1 triggers the phosphorylation of p38 mitogen-activated protein kinase, which is thought to induce apoptosis of the affected keratinocyte. Although complement component (C) 3 deposition on direct immunofluorescence (DIF) initially suggested that it may play a role in acantholysis in PF, both C5-deficient mice and total complement-depleted mice develop subcorneal vesicles upon passive transfer of pathogenic human sera. The pathogenesis of PF is covered elsewhere in this issue in more detail by Valeria Aoki.
There are two predominant types of PF: idiopathic PF, which is found universally and occurs sporadically, and fogo selvagem (FS), an endemic variety linked exclusively to multiple distinct geographic areas. Other, albeit rarer, variants of PF have been described, including pemphigus erythematosus (PE, Senear-Usher syndrome) and drug-induced PF. IgA pemphigus and pemphigus herpetiformis (PH) have previously been described in the literature as variants of PF, but appear to be distinct subtypes of the general pemphigus category, both clinically and histopathologically.
Clinical features
Epidemiology
The worldwide incidence and prevalence of PF is very low, making it a rare disease. Because of the presence of endemic areas, however, these figures may vary considerably based on the specific geographic area being studied. For instance, the incidence of PF in Tunisia has been found to be as high as 6.7 new cases per million per year. In Brazil, which has multiple foci of endemic PF, there is a region located in the state of Mato Grosso do Sul that has a prevalence equal to approximately 3% of its population. Other endemic areas are found within Colombia and Peru. The average age of nonendemic PF symptom onset ranges from 40 to 60 years of age. FS affects a larger number of children and young adults as symptoms usually begin during the second or third decade of life. Both sporadic and endemic PF are typically seen equally in men and women and affect those of all races and ethnicities. However, there are populations of FS that may deviate from the norm. For example, epidemiologic studies in Tunisia found the female-to-male ratio of incidence rates to be approximately 4 to 1.
Patient History
Patients usually report a history of blister formation on the skin ( Fig. 1 ). Lesions commonly begin on the trunk, but may also originate as localized lesions on the face or scalp. The patient may be unaware of the blisters because they rupture very easily. In these cases, there may only be a history of superficial sores or areas of crusting. Pain and/or a burning sensation localized to the areas of the lesions may be noted. Unlike pemphigus vulgaris (PV), there is typically no history of oral or other mucosal lesions. The lesions may become widespread. Patients with the mildest form of PF may only report a history of a small, solitary, recurrent scaly and crusty lesion of the face ( Fig. 2 ). In these cases, it may be years before the patient is correctly diagnosed. In cases of PE, patients report the development of lesions in sun-exposed areas of the face, scalp, and upper chest and back—similar to the distribution of lesions seen in lupus erythematosus.
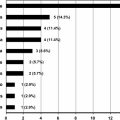
Because multiple drugs have been found to be associated with the development of PF, it is important to thoroughly review the patient’s current medications. The most commonly implicated drug is penicillamine, which is a chelating agent used to treat Wilson disease, lead and arsenic poisoning, and severe active rheumatoid arthritis. Drug-associated cases may persist or quickly clear after the offending agent is withdrawn. Various angiotensin-converting enzyme (ACE) inhibitors have also been found to induce pemphigus. Box 1 shows other drugs that have been associated with PF. Most of these drugs contain thiol (-SH) functional groups in their chemical structure, whereas others have disulfide bonds that are cleaved during metabolism to yield thiol groups. PF can also be either induced or exacerbated by exposure to ultraviolet light and ionizing radiation.
ACE inhibitors
Captopril
Lisinopril
Enalapril
Fosinopril
Disease-modifying antirheumatic drugs
Penicillamine
Bucillamine
Angiotensin-II receptor blockers
Candesartan
Antibiotics
Rifampicin
Orphan drugs
Tiopronin
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree