Fig. 14.1
Case I. (a). Design of platysma myocutaneous flap. (b) The primary focus of the hypopharyngeal cancer was resected. (c)The hypopharyngeal defect after resection of the primary focus. (d) The platysma myocutaneous flap was used to repair the hypopharyngeal defect. (e) The situation when the surgery was completed
2.2.2 Repair of the Hypopharyngeal Defect with Submental Flap
The blood supply of submental flap comes from the branch of the facial artery. The submental artery starts at about 5 mm below the mandible; runs forward to the upper margin of the submaxillary gland, superficial surface of the mylohyoid muscle, and the anterior belly of the digastric muscle; and gives off one to four artery perforators on the way to the platysma muscle and submental skin. The submental artery has one to two accompanying veins which converge into the facial vein. When the skin flap is prepared, the incision is made at the upper incisal margin of the skin flap at the level of about 2 cm from the lower margin of the mandible, and the facial artery and vein and the marginal mandibular branch of the facial nerve are protected. Then the submandibular gland and surrounding lymph nodes are removed, and attentions should be paid to protecting the blood vessel branches and perforators of the submental flap. The skin flap includes the skin, platysma muscle, and part of the anterior belly of digastric muscle. The skin flap can maximally reach to 6 cm × 8 cm with a thickness of 1–2 cm, and the vascular pedicle is 6 cm in length. After the removal of the primary focus and cervical lymph nodes, the cervical lymph node dissection is performed, while the external maxillary artery and vein are retained and protected from damage. After the primary focuses of the laryngeal cancer and hypopharyngeal cancer are resected, the submental flap is transferred into the pharyngeal cavity, and the skin of the skin flap is sutured with the pharyngeal and residual laryngeal mucosa, and then the hypopharyngeal defect at one side after half laryngectomy is repaired. We applied this skin flap to repair the hypopharyngeal defect in 33 patients, and all patients achieved successful results, but the disadvantage was that the beard grew out from the pharyngeal flap of the male patient. Finally the laser is used to point fire the hair follicles for dehairing [10].
Case II
The patient, male, 62 years old, was admitted into the hospital because of having a sore throat for 3 months and hoarseness for 1 month. The mass in the medial wall of the left pyriform sinus was 2.5 cm × 1.5 cm, and the surface was ulcerated. Admission diagnosis: left hypopharyngeal cancer T2N0M0. The patient underwent resection of the left vertical part of the throat and hypopharyngeal cancer; lymph node dissection in areas II, III, and IV; and the repair of hypopharyngeal and laryngeal defects with submental flap (Fig. 14.2). Postoperative pathological examination report: left hypopharyngeal highly and moderately differentiated squamous cell carcinoma, and no cancer was observed in the incisal margins and cervical lymph nodes.
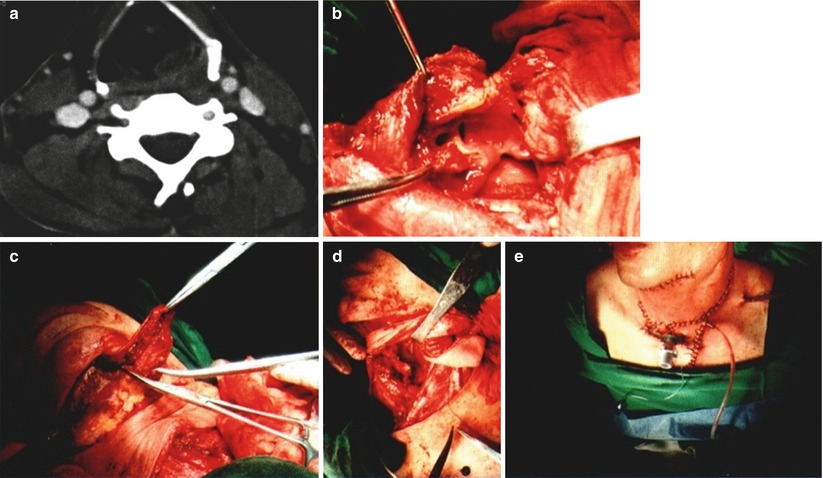
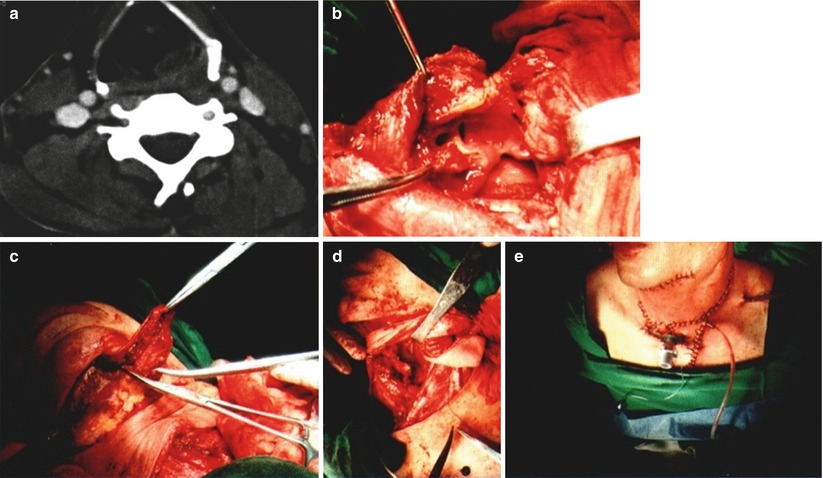
Fig. 14.2
Case II. (a) Preoperative CT showed lesions within the medial wall of the pyriform sinus. (b) The primary focus was resected, and the right half of the throat was preserved. (c) The submental flap was prepared. (d) The left laryngeal and hypopharyngeal defects were repaired with the submental flap. (e) The surgery was completed
2.2.3 Repair of Posterior Pharyngeal Wall Defect with Forearm Skin Flap
The repair of posterior pharyngeal wall defect can use the skin transplantation, forearm skin flap, free jejunum, and platysma myocutaneous flap [11]. When the resection is only limited to the mucous layer, it may be allowed to heal by itself, or the split flap is transplanted. When the split flap is transplanted, the apposition suture of the peripheral side and the mucosal margin of the posterior pharyngeal wall is performed, and the middle part is pinned and sutured to the prevertebral fascia with a 3-0 silk thread by an interval of 1 cm. Peng Jieren reported that acellular artificial tissue patch was used to repair the posterior pharyngeal wall defect, because the basic structure of the artificial tissue patch is the fibroblast-populated collagen lattice, and the immune response induced by the allogenic skin plays main effects on components such as epidermal cells, dermal fibroblasts, and endothelial cells, while the noncellular components in the dermis such as extracellular matrix protein and collagen are immunoincompetent relatively [12]. After repair of the laryngeal wall defect, the mucosal cells in normal incisal margins crawl along the scaffold of the tissue patch and finally cover the entire defect area to become the mucosal epithelia. The incidence rate of pharyngeal fistula is low, and the preoperative and postoperative radiotherapies do not affect the tissue patch transplantation. The platysma myocutaneous flap can also be prepared through lateral pharyngeal incision approach and covered onto the posterior pharyngeal wall defect. The larger posterior pharyngeal wall defect requires meticulous surgical reconstruction. Because of its moderate thickness, the radial forearm free flap has become the suitable skin flap for repair of skin and mucosal defects which are not necessary to be repaired with thick soft tissue, and it is the best material for hypopharyngeal reconstruction. After it is repaired and sutured tightly with the mucous membrane, the swallowing function of the patient can be satisfactorily recovered. The forearm skin flap of 5 cm × 6.5 cm is designed upward at the site with a distance of 3 cm from proximal horizontal grain line of the left wrist, and the skin, subcutaneous tissue, and superficial fascia are incised on the forearm midline along the running direction of the radial artery; meanwhile the superficial branch of the radial nerve is protected and preserved. Between the brachioradialis muscle and the flexor carpi radialis muscle, the radial artery and its accompanying veins are exposed, and the dissection is performed upward to ligate the small branches of arteries and veins. The distal ends of the radial artery and the accompanying veins are ligated and cut off at the end of the skin flap close to the wrist, and attentions are paid to protecting the close linkage of the blood vessels with the skin flap. Between the brachioradialis muscle and pronator teres muscle, the vascular pedicle is dissociated to site at 5 cm near the elbow joint and then is ligated and cut off, so that the length of vascular pedicle of the skin flap can reach up to about 10 cm. After the preparation of skin flap is completed, the radial artery and vein are anastomosed with the superior thyroid artery and vein or the facial artery and vein. The skin flap can also be placed in appropriate location of the posterior pharyngeal wall, before vascular anastomosis, and three fourths of skin flap is sutured with the mucosa. To avoid esophageal stenosis, when the posterior wall of the cervical esophagus is sutured with the free skin flap, the middle of the posterior wall of the esophagus may be ripped off longitudinally by a small portion, and the wedge-shaped skin is implanted. Our department also successfully repairs the posterior pharyngeal wall defect using the anterolateral thigh flap. It is noted that the skin flap should be trimmed thinly during surgery using the perforator flap technique.
Case III
The patient, male, 58 years old, was admitted into the hospital because of having a sore throat for 2 months. The posterior pharyngeal wall mass was 2.0 cm × 1.5 cm, and the surface was ulcerated. Admission diagnosis: right hypopharyngeal cancer T1N0M0. The patient underwent resection of posterior pharyngeal wall cancer with preservation of throat + lymph node dissection in right areas II, III, and IV + the repair of posterior pharyngeal wall defect with free forearm skin flap under the general anesthesia (Fig. 14.3). Postoperative pathological examination report: left hypopharyngeal highly and moderately differentiated squamous cell carcinoma, and no cancer was observed in the incisal margins and cervical lymph nodes.
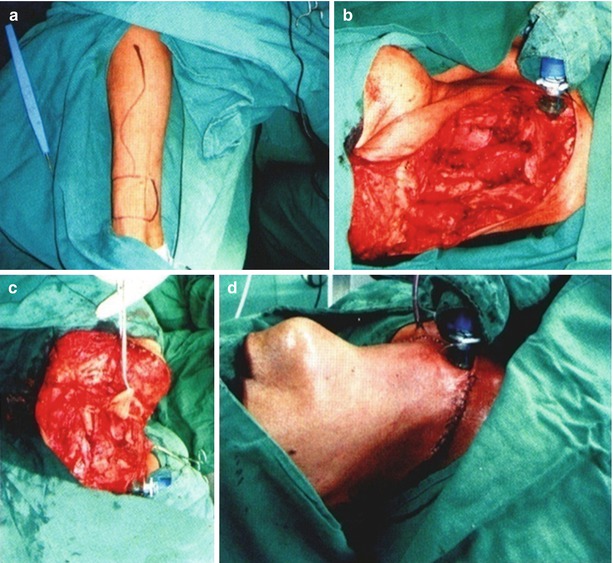
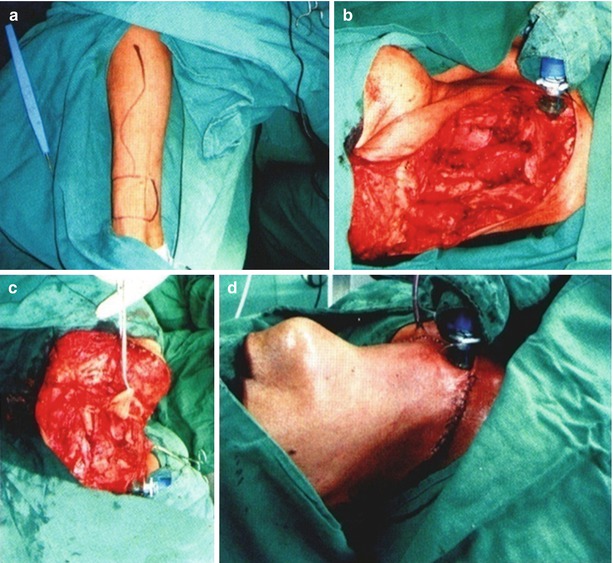
Fig. 14.3
Case III. (a) Design of forearm skin flap. (b) The defects in the right lateral and posterior walls of the laryngopharynx after resection of hypopharyngeal cancer. (c) Repair of posterior pharyngeal wall defect with forearm skin flap. (d) The surgery was completed
2.2.4 Repair of Posterior Hypopharyngeal Wall Defect with Free Jejunum
After resection of T2 and selected T3 lesions in posterior hypopharyngeal wall area, the defects can be repaired with free jejunum. The jejunum wall far away from the mesentery is split off to form the jejunum graft, which is sutured with the mucosal margin of the pharyngeal defect, and the jejunum mucosal surface is taken as the pharyngeal mucosa, and then the mesenteric artery and vein are anastomosed with the appropriately selected artery and vein. The esophageal invasion of the posterior hypopharyngeal wall cancer often causes most of hypopharyngeal and cervical esophageal defects, and thus the free jejunum can be selected to repair the hypopharyngeal and cervical esophageal defects, while the pronunciation function of the throat body is preserved [13, 14]. The jejunum segment is used to repair the pharyngeal defect above esophageal entrance, and the mesenteric margin corresponding to the jejunum segment should be split off longitudinally, and the form of the jejunum graft is used to repair the pharyngeal defect. The lower jejunum segment is anastomosed with the cervical esophagus stump, and the mesenteric artery and vein are anastomosed with the appropriately selected artery and vein. The surgery is relatively simple, but the walls of the mesenteric artery and vein are thin, and a high level of microvascular anastomotic techniques and clinical experiences are required. The ideal supplying arteries include the facial artery, thyroid artery, lingual artery, or transverse cervical artery. In the abdominal surgery group, the upper middle abdominal incision is made, and the jejunum segment is selectively transplanted. The proximal jejunum segment has richer vascular arcades and is more suitable for transplantation. The end-to-end anastomosis between the jejunum segment and esophagus is very ideal. Among the ideal blood vessels of the jejunum segment, there is an artery and a vein running into the mesenteric root. The blood vessels within the mesentery feeding the jejunum are not cut off at first, and they will be treated when the transplantation is performed. In order to ensure that the jejunum segment wriggles downward from upper to lower levels, it is necessary to make a mark in the jejunum wall, anastomose the proximal jejunum segment with the pharyngeal area, and anastomose the distal jejunum segment with the cervical esophagus stump. Such wriggling way is conducive to swallowing. The transplanted jejunum segment is implanted into the cervical area at first, and the nasogastric tube is inserted into the jejunum segment. Later, the pharynx-jejunum anastomosis and the jejunum-esophagus anastomosis are performed, and then the vascular anastomosis is performed under the microscope. The length of the jejunum segment should be appropriate, and if it is too long, the speed of swallowing can be slowed down. Due to the maturity of the laparoscopic technique, the donor jejunum can be harvested under the laparoscope to reduce the abdominal complications [15].
Case IV
The patient, male, is 53 years old. The admission examination showed cauliflower-shaped mass in the posterior hypopharyngeal wall and esophageal entrance, and the esophageal entrance was narrow, so the gastroscope could not enter through it. Bilateral vocal cords had good activity, and the laryngeal structures were normal. Admission diagnosis: hypopharyngeal and cervical esophageal cancers. After admission, the esophageal barium swallow X-ray inspection showed cervical esophageal mucosal disorders of about 4 cm with irregular filling defect. When the resection of hypopharyngeal and cervical esophageal cancers combined with left cervical lymph node dissection was performed, it was observed that the mass mainly invaded the posterior hypopharyngeal wall, esophageal entrance, and 5 cm cervical esophagus, but the postcricoid mucosa was normal, and bilateral arytenoid cartilages and throat body were normal; thus it was decided to preserve the throat body and perform the esophageal replacement with free jejunum. 15 cm jejunum was harvested and transplanted to the cervical area, then the intestinal wall of 4 cm was incised longitudinally at the contralateral side of the mesentery in the upper end, and then it was tiled and sutured with the retropharyngeal mucosa and postcricoid mucosa to repair the posterior hypopharyngeal wall defect; the end-to-end anastomosis between the lower end of the jejunum and the esophageal stump (equivalent to the level of the clavicle) was performed. Under the microscope, the mesenteric artery was anastomosed with the superior thyroid artery, and the mesenteric vein was anastomosed with the external jugular vein; meanwhile it was noted that the recurrent laryngeal nerve and the myolemma of the posterior cricoarytenoid muscle were not damaged. The blood supply of the jejunum was good after surgery. The anti-inflammatory, supportive, and symptomatic treatments were carried out after surgery, and the patient healed well. The reexamination was performed at 1 year after surgery, and the eating and swallowing functions returned to normal except when the patient was eating, a few choking coughs and a mild hoarseness would occur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree