Key Terms
Epidermoid Cyst
Epidermal inclusion cyst
Milium
Ruptured epidermoid cysts
Apocrine Cystadenoma
Apocrine hidrocystomas
Cutaneous Odontogenic Sinus Tract
Cutaneous dental sinus tract
Dentocutaneous sinus tract
True cysts of the skin represent epithelium-lined structures and may be caused by epidermis driven into the dermis (e.g., epidermal inclusion cysts), or they can arise from a variety of normal skin structures, such as hair follicles (e.g., epidermoid cysts, trichilemmal cysts), sebaceous duct (e.g., steatocystomas), apocrine glands and ducts (e.g., apocrine cystadenoma), and eccrine glands and ducts (e.g., eccrine hidrocystoma). Cutaneous sinuses represent epithelium-lined channels that communicate with a deeper process, such as a dental abscess. Finally, there are cyst-like structures of the skin that are not lined by an epithelium but arise from deeper structures, such as tendon-sheath (ganglion) and joint spaces (digital mucous cyst).
Important History Questions
How long has the lesion(s) been present?
Most cystic structures of the skin are acquired, but dermoid cysts are congenital. Therefore questioning is important when evaluating a potential cyst around the eyes or posterior axial skeleton of a child, because congenital lesions in these areas may connect to deeper structures and are often not amenable to outpatient surgery.
Has the lesion changed?
Malignant tumors may be indistinguishable from cysts, and malignancy may arise in long-standing cysts; thus, change is important to identify. On rare occasion, a squamous cell carcinoma may even develop in common epidermoid cysts, so any change in behavior is a noteworthy event.
Important Physical Findings
How are the lesion(s) distributed?
Some cysts have characteristic locations. For example, trichilemmal cysts are most common on the scalp, whereas apocrine cystadenomas are most common on the eyelid margins.
How many lesions are there?
Some cystic lesions are characteristically solitary (e.g., digital mucous cyst), whereas others are often multiple (e.g., steatocystomas, eruptive vellus hair cysts).
Does the cyst demonstrate transillumination?
Some cysts are filled with clear or translucent material (e.g., apocrine cystadenoma; Fig. 34.1 ), which can be demonstrated via transillumination. Cysts that contain keratin (e.g., epidermoid cysts) do not transilluminate in the same brilliant manner.

Does the cyst have a punctum?
Epidermoid inclusion cysts nearly always demonstrate a punctum that can be visualized with the unaided eye, whereas other types of cysts, such as a trichilemmal cyst, often do not manifest a punctum.
Epidermoid Cyst
ICD10 code L72.0
RETENTION CYST
Pathogenesis
An epidermoid cyst, also called an epidermal cyst or sebaceous cyst (the latter is inaccurate and is disfavored) is the most common cyst of the skin. Epidermoid cysts are derived from the infundibulum (upper portion) of the hair follicle and are filled with keratin rather than sebaceous material. Some epidermoid cysts may be induced by trauma or follicular inflammation, especially acne ( Fig. 34.2 ). An epidermal inclusion cyst is a closely related entity caused by inclusion of a fragment of epidermis into the dermis, without an attachment to a hair follicle ( Fig. 34.3 ), and it is nearly always related to trauma. A milium (plural milia) is simply a small epidermoid cyst (≤2 mm in diameter).

Clinical Features
- •
Epidermoid cysts can occur at any age but are most common in adolescents and young adults.
- •
Epidermoid cysts can be solitary or multiple.
- •
The face, neck, upper trunk, and scrotum are preferentially affected by epidermoid cysts.
- •
Epidermoid cysts exist as skin-colored dermal nodules that may extend into the subcutis (see Fig. 34.2 ).
- •
A punctum or keratin-filled follicular, comedone-like opening may be present on the skin surface.
- •
If the punctum is large enough, white, foul-smelling, cheese-like keratin debris may be expressed.
- •
The size of epidermoid cysts varies, but most are 0.4 to 4 cm in diameter.
- •
Ruptured epidermoid cysts may engender inflammation, with acute pain, erythema, and dramatic enlargement ( Figs. 34.4 and 34.5 ). Drainage of pus and cystic contents may occur.

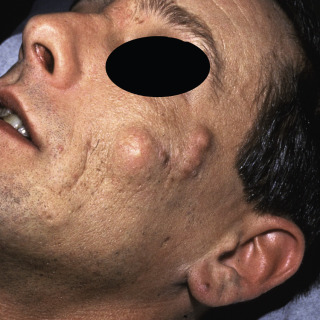
Fig. 34.4
Inflamed epidermoid cyst due to rupture of cyst wall. The inflammation is due to a foreign body reaction and not infection.
(From the Fitzsimons Army Medical Center Collection, Aurora, CO.)

Fig. 34.5
Incision with a no. 11 scalpel blade allows drainage of pus and keratin.
(From the Fitzsimons Army Medical Center Collection, Aurora, CO.)
Diagnosis
- •
The clinical presentation of a flesh-colored cystic nodule, located in the dermis and/or subcutis, often with an identifiable punctum, is diagnostic.
- •
In some cases, foul-smelling keratin debris can be expressed through the punctum or through a small incision with a no. 11 scalpel blade, further establishing the diagnosis.
- •
Rare cases may require surgical extirpation, with histopathologic assessment for diagnosis.
Treatment
- •
Epidermoid cysts are benign and do not require treatment unless they are symptomatic or unless there is concern for a commingled malignancy.
- •
Excision of the entire cyst is often utilized to ensure complete removal.
- •
An alternative procedure is incision with a no. 11 scalpel blade, or 3- or 4-mm punch, followed by careful removal of the entire the cyst wall with forceps and scissors. Use of this technique is more tedious and requires greater surgical expertise, but it results in a smaller scar.
- •
Ruptured or inflamed epidermoid cysts can be injected with intralesional triamcinolone (2–5 mg/mL). Cysts that are ripe or have already begun to drain should be incised with a no. 11 scalpel blade, with the contents evacuated, followed by intralesional triamcinolone (2–5 mg/mL). Although erythema may be interpreted as an infected cyst, in most cases the reaction is due to a foreign body response to the keratin, and oral antibiotics are not usually required.
Clinical Course
Once present, epidermoid cysts usually persist. In about one-third of cases, where there is spontaneous rupture of the cyst wall, the cyst is completely destroyed by the inflammatory response, leading to resolution.
Trichilemmal Cyst
ICD10 code L72.1
NEOPLASTIC CYST
Pathogenesis
A trichilemmal cyst, also known as a pilar cyst or wen, is the second most common form of follicular cyst. In contrast to epidermoid cysts, which arise from the upper third of the hair follicle, trichilemmal cysts arise from the middle third of the hair follicle, a region called the isthmus. The pathogenesis of solitary trichilemmal cysts is unknown, but when multiple trichilemmal cysts are present, a familial autosomal dominant pattern of inheritance has been observed.
Clinical Features
- •
Trichilemmal cysts develop in adults, with women being affected more often than men.
- •
The vast majority of trichilemmal cysts involve the scalp, although any area of the body can be affected.
- •
Trichilemmal cysts present as smooth, firm, mobile subcutaneous nodules ( Figs. 34.6 and 34.7 ).