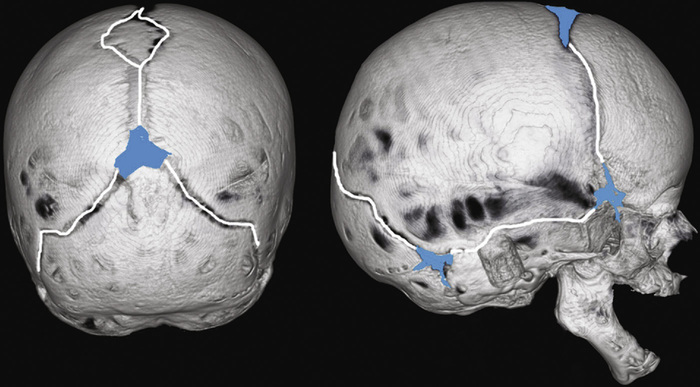
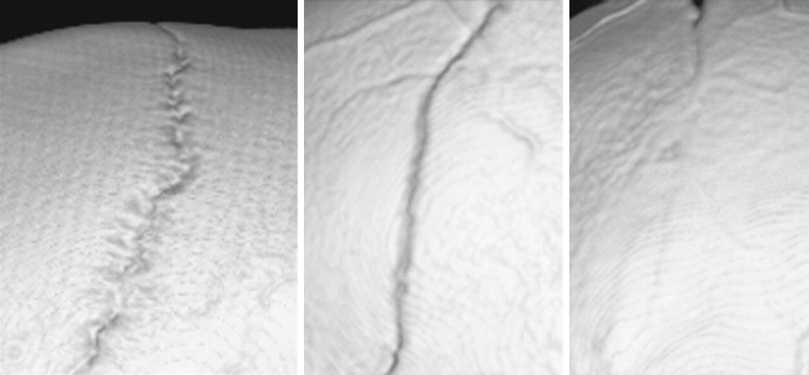
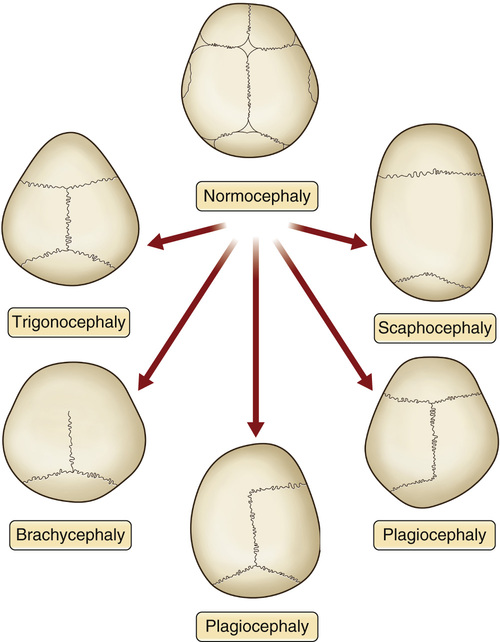
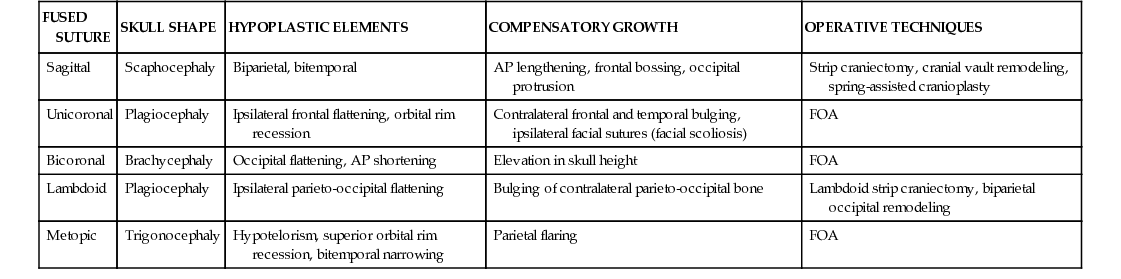
1. Craniosynostosis: Abnormal fusion of cranial sutures leading to abnormal head shape • May lead to increased intracranial pressure (ICP) and developmental delay ▪ Increased ICP can be diagnosed by papilledema and “thumb printing” on radiographic studies. • Prevalence: ~1:2500 live births • Syndromic craniosynostoses and their related gene mutations ▪ Saethre-Chotzen syndrome: TWIST 1 2. Cranial sutures (see Figure 5.1) • With an open suture, the bone grows perpendicular to the suture line. • When the suture is fused, compensatory bone growth occurs parallel to the suture line (see Table 5.2). 3. Suture closure (see Figure 5.2) • Hypertelorism: Abnormal increase in the distance between the bony orbits • Hypotelorism: Decreased distance between the bony orbits • Telecanthus: Increased distance between the medial canthi • Exorbitism: Protrusion of the globe due to decreased volume of orbit See Figure 5.3. • Also known as trigonocephaly (“triangular-shaped” head) ▪ Metopic ridge (in mild cases) • Most likely to be associated with midline brain abnormalities • Also known as scaphocephaly (“boat-shaped head”) or dolichocephaly ▪ Bilateral frontal and occipital bossing ▪ Elongated head in the anteroposterior direction • Unilateral coronal synostosis is characterized by ▪ Flattening of the ipsilateral forehead and supraorbital rim ▪ Contralateral forehead bossing ▪ Anterior displacement of the ipsilateral ear ▪ Deviation of the nasal root toward the affected side • Bilateral coronal synostosis is characterized by ▪ Decreased anteroposterior length • Also known as posterior plagiocephaly; very rare • Distinguished from deformational plagiocephaly by a “trapezoid”-shaped head ▪ Flattening of the ipsilateral occiput ▪ Inferior displaced mastoid bulge on affected side ▪ Contralateral forehead bossing ▪ Inferior displacement of the ipsilateral ear 5. Multisuture craniosynostosis • Involves premature fusion of multiple sutures • In the most severe form (pansutural synostosis), patients can develop a “cloverleaf” skull deformity (also known as the kleeblattschädel skull deformity) ▪ Characterized by a “moth-eaten” appearance of bone on computed tomography (CT) imaging ▪ May lead to severe increases in ICP and airway anomalies 6. Treatment of craniosynostosis depends on severity, appearance, and functional concerns. 7. Surgical treatment options (see Table 5.1) • Cranial vault remodeling: Multiple techniques have been described. ▪ Surgery is often performed between 6 and 12 months of age. ▪ Useful for advancements >1 cm ○ A typical latency phase lasts between 1 and 7 days. ○ A typical consolidation period is twice the duration of the active distraction. ▪ Often, LeFort I or III advancements Table 5.1 Skull Deformity in Craniosynostosis and Operative Techniques Used for Correction
Craniosynostosis and Craniofacial Syndromes
General Craniosynostosis Nomenclature and Information
Craniosynostoses
FUSED SUTURE
SKULL SHAPE
HYPOPLASTIC ELEMENTS
COMPENSATORY GROWTH
OPERATIVE TECHNIQUES
Sagittal
Scaphocephaly
Biparietal, bitemporal
AP lengthening, frontal bossing, occipital protrusion
Strip craniectomy, cranial vault remodeling, spring-assisted cranioplasty
Unicoronal
Plagiocephaly
Ipsilateral frontal flattening, orbital rim recession
Contralateral frontal and temporal bulging, ipsilateral facial sutures (facial scoliosis)
FOA
Bicoronal
Brachycephaly
Occipital flattening, AP shortening
Elevation in skull height
FOA
Lambdoid
Plagiocephaly
Ipsilateral parieto-occipital flattening
Bulging of contralateral parieto-occipital bone
Lambdoid strip craniectomy, biparietal occipital remodeling
Metopic
Trigonocephaly
Hypotelorism, superior orbital rim recession, bitemporal narrowing
Parietal flaring
FOA
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Craniosynostosis and Craniofacial Syndromes
Chapter 5