Correction of Orbital Floor Blow-Out Fractures: Variation 2
Henry C. Vasconez
DEFINITION
The orbit is a paired structure of the upper craniofacial skeleton.
It houses the globe, nerves, vessels, and surrounding soft tissue structures.
The orbital floor consists of very thin bone and ligamentous structures and therefore is easily fractured when sustaining a significant force.
ANATOMY
The orbit is a paired structure that has a conical shape and is separated in the midline by the interorbital structures consisting primarily of the ethmoid and frontal sinuses and the underlying nasal structures.
The cone or bony pyramid of the orbit is made up of a roof, floor, and medial and lateral walls.
At the apex of the cone posteriorly lie the optic nerve and other important nerves and vessels.
The orbital floor forms the roof of the maxillary sinus, slopes upward and medially toward the apex of the cone, and has an AP distance of approximately 45 mm.
The bony orbit volume is approximately 30 cc and the globe is approximately 7 cc.
The anterior portion of the floor is concave; the posterior portion is convex and is the thinnest part of the floor and sustains most of the fractures.
PATHOGENESIS
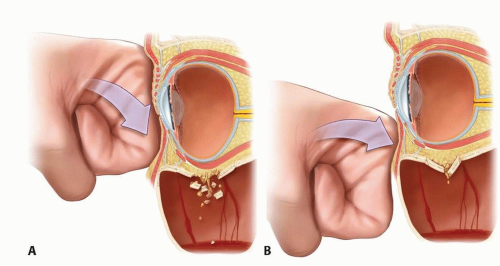
Orbital floor fractures are categorized as pure or impure blow-out fractures.2
There are also linear or cracked and trapdoor fractures as well as comminuted fractures of the floor.
The type of fracture depends, in large measure, on the vector and amount of force applied to the orbit or surrounding skeletal structures.
A pure blow-out fracture involves the thin floor and medial and/or lateral walls of the orbit.
An impure blow-out fracture involves the disruption of the thick orbital rim and, many times, adjacent facial skeletal structures.
A trapdoor orbital fracture is a pure orbital blow-out fracture, whereby a bony fragment is displaced inferiorly, into the maxillary sinus, while still being hinged. Orbital structures herniate through this defect and become entrapped.
Orbital contents that can become entrapped include the periocular muscles, commonly the inferior rectus and inferior oblique. Muscle entrapment causes restriction of upward gaze and consequent diplopia.
NATURAL HISTORY
Significant controversy remains regarding the indications for operative repair of orbital floor fractures.
Nondisplaced or mildly displaced orbital floor fractures will tend to do well after edema subsides and the brain adapts to the small visual field discrepancy.
Diplopia secondary to enophthalmos, significant defects in ocular motility, and significant radiographic findings are all important indications for operative intervention.
Entrapment of orbital contents, especially in the pediatric age group, can lead to significant, early symptoms, both visual and systemic (including nausea and vomiting), and should be addressed urgently.
Significant orbital floor fractures that remain untreated can later present problems to the patient and can be very challenging to correct properly.
PATIENT HISTORY AND PHYSICAL FINDINGS
Most orbital floor fractures result from blunt injuries, primarily from motor vehicle crashes or assaults.3
Signs and symptoms of these fractures include edema and bruising, pain, diplopia, subconjunctival hemorrhage, sensory deficits mostly in the infraorbital region, and, at times, visual deficits.
Ophthalmology should be consulted with any visual field deficits.
The position of the globe, including cornea and pupil, is important to asses and compare with the contralateral, uninjured side.
Extraocular muscle movements are then tested for any pain or deficits.
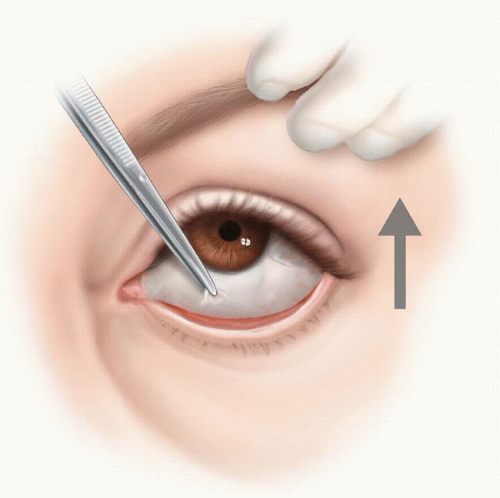
In the unconscious patient, extraocular muscle movements can be assessed by performing a forced duction exam, testing for any restriction of muscles or associated structures (FIG 2). If possible, this result is compared with the contralateral side.
Gentle yet thorough palpation of the orbit and its periorbital structures, is performed to identify obvious fractures or step-offs.
Examination of the pupils is important to identify an optic nerve injury or other afferent pupillary defects. Consensual and accommodation reflexes are also evaluated.
The oculocardiac reflex is particularly important in children with entrapment of orbital structures in the floor. An increase in vagal tone can lead to nausea and vomiting and ultimately cardiac disorders, including asystole. These cases should be managed emergently.
Volume discrepancies of the orbit can lead to enophthalmos or dystopia of the globe. Early evaluation can be difficult because of edema and should be carefully monitored over a 2-week period as the edema subsides and the displacement becomes more obvious.
Delayed enophthalmos repair may be necessary even weeks after the injury if it is noted to be greater than 2 mm in an AP direction or is contributing to visual disturbances.
IMAGING
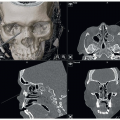
CT scanning has revolutionized the diagnosis and treatment of orbital fractures.
Coronal and sagittal reconstructions are most helpful for orbital floor fractures (FIG 3). They define the extent, size, and location of the injury, as well as associated injuries.
3D reconstructions can be helpful, especially in extensive injuries to outline any other affected structures. This is very usual in nasoethmoidal orbital fractures, as well as associated zygomatic maxillary fractures.
CT scan imaging distinguishes between a pure and an impure orbital floor blow-out fracture.
DIFFERENTIAL DIAGNOSIS
Orbital roof fractures
Medial orbit fractures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree