Correction of Orbital Floor Blow-Out Fractures: Variation 1
Jean-Francois Lefaivre
David Charles A. Fisher
DEFINITION
Orbital blow-out fractures commonly result from force directly applied to the globe with subsequent energy transmission through the thin surrounding bones. The affected bones are typically the orbital floor and medial wall. It may be accompanied by entrapment of the inferior rectus muscle and inferior oblique muscle. True entrapment is a rare clinical finding. It is often mentioned on radiology reports and must be differentiated from herniation.
Orbital floor fractures are often associated with additional facial fractures and soft tissue injury.
ANATOMY1
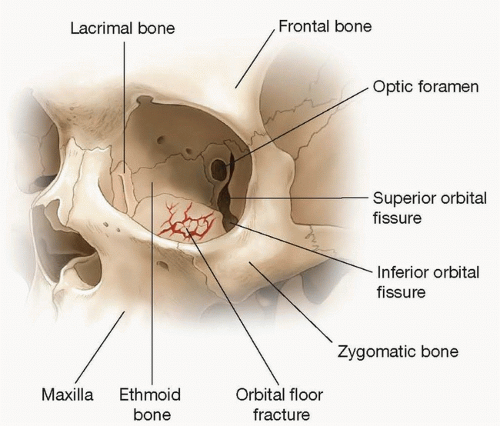
The orbital floor is composed of thin maxillary and zygomatic bone. Anteriorly, just behind the orbital rim, the floor is concave and becomes convex, posterior to the axis of the globe. It is bordered laterally by the lateral orbital wall, which is relatively thick, and consists of the frontal process of the zygoma, and greater and lesser wings of the sphenoid. Medially, the floor slopes upward toward the medial orbital wall, which is also a thin bony structure, made of the frontal bone superiorly, lacrimal bone anteriorly, and lamina papyracea of the ethmoid and lesser wing of the sphenoid posteriorly. The lamina papyracea, as its name implies, is thin and fragile.
The inferior orbital fissure is located between the orbital floor and lateral orbital wall. Structures present in the fissure include the maxillary division of the trigeminal nerve, infraorbital artery, zygomatic nerve, branches of the sphenopalatine ganglion, and branches of the ophthalmic vein. The inferior orbital fissure is also known as the sphenomaxillary fissure (FIG 1).
The orbital plate of the maxilla and a portion of the zygoma represent the orbital floor. The zygoma makes up the anterior portion of the orbital floor, anterior to the inferior orbital fissure. The infraorbital nerve runs through the orbital floor in the infraorbital groove posteriorly and in the infraorbital canal anteriorly. The nerve often provides a landmark and a good plane of dissection.
The infraorbital rim is made of zygomatic bone and maxilla. The frontal zygomatic suture is exposed during dissection. Just inferior to the inferior orbital rim, the infraorbital foramen is located about 1 cm below the rim, generally in line with the midaxis of the pupil.
Both the orbital floor and medial orbital wall are vulnerable to injury because they are relatively thin compared to the surrounding structures.
Knowledge of anatomy is essential to perform safe dissection and optimal exposure of the orbital floor defect.
PATHOGENESIS
Orbital blow-out fracture is often the result of blunt injury to the globe and/or orbital rim, sustained during altercations, falls, sports-related injury, or motor vehicle accidents. These injuries transmit an external force to the orbital contents and orbital bones. The weakest portion of the orbit then fractures, resulting in herniation of orbital contents through the bony defect. The anterior and posterior portions of the orbital floor are thicker. The middle portion of the orbital floor is thinner, which accounts for the majority of fractures into the maxillary sinus. The medial orbital wall also commonly fractures into the ethmoid sinus air cells.
The globe typically moves posteriorly, inferiorly, and medially if there is significant prolapse or herniation of the orbital content into the orbital floor defect.
NATURAL HISTORY
Untreated fractures generally result in enophthalmos. Depending on the volume increase associated with orbital fracture, it will range from minimally to significantly noticeable. Enophthalmos can be identified clinically with 2 mm of posterior displacement of the globe.2 A 5% increase in orbital volume is sufficient for a clinical diagnosis of enophthalmos.2 An important part of informed surgical consent is to discuss the anticipated natural history of untreated defects. Hypoesthesia in the distribution of a second branch
of the trigeminal nerve generally resolves over several months. Diplopia may improve if it is secondary to muscle contusion.
If an entrapped muscle is not treated promptly, permanent ischemic injury to the extraocular muscle will result in diplopia. It is the only emergency associated with orbital floor fractures. Our experience, as previously reported, is that it is more common in children than in adults.
Retrobulbar hematoma that results in optic nerve compression is an emergency; however, in a blow-out fracture, there is typically an expanded volume that alleviates the pressure on the orbital apex.
Patients with large orbital floor defects are generally treated acutely secondary to obvious enophthalmos. Patients with more subtle findings may be observed initially and surgically treated when/if they develop enophthalmos. These are generally patients with smaller defects on computed tomography (CT) scans.3
The decision of whether or not to operate can generally be made within the first 6 weeks following injury. Longer follow-up may be recommended in patients managed nonoperatively.
PATIENT HISTORY AND PHYSICAL FINDINGS
Specific trauma-related history helps elucidate the amount of force transmitted to the globe and orbit.
Previous eye surgery, eye injury, or pathology should be documented as well as the use of prescription glasses or contact lenses.
Physical examination often reveals
Periorbital ecchymosis and swelling
Subconjunctival hemorrhage
Enophthalmos, most easily identified by both a worm’s eye and a bird’s eye view; may be masked by edema early after injury
Diplopia, often in upward gaze
Hypoesthesia in the distribution of the second branch of the trigeminal nerve, involving the cheek, nose, upper lip, gingiva, and upper teeth in various distributions
Visual acuity, extraocular movements, and pupil examination need to be assessed
Preoperative consultation with ophthalmology may be beneficial, especially in patients with decreased visual acuity or retrobulbar hemorrhage.
IMAGING
Orbital or maxillofacial CT scan with 1 to 2 mm axial cuts and coronal and sagittal cuts will help understand the size and location of the defect, as well as soft tissue herniation. It will help determine the length and width of the bone graft or implant required for adequate repair4 (Video 1).
A three-dimensional (3D) reconstruction is often beneficial in patients with multiple associated facial fractures. It is not essential for isolated orbital floor fractures.
DIFFERENTIAL DIAGNOSIS
Medial orbital wall fractures may result in similar findings.
Medial orbital wall defects should be identified preoperatively.
Surgical treatment of orbital floor fractures that do not address associated medial floor fractures will result in only partial correction of enophthalmos.
NONOPERATIVE MANAGEMENT
Small defects without herniation of orbital contents and without entrapment may be managed conservatively with close follow-up.
SURGICAL MANAGEMENT
The primary objective of surgical intervention is to recreate normal anatomy with restoration of the orbital floor integrity and reduction of herniated soft tissue into normal position. Restoration of orbital shape and volume should help rebalance extraocular muscles and correct diplopia.
Indications to correct orbital floor fractures include the following:
Enophthalmos
Large orbital floor defects with herniation on CT scan. Some authors mention that a 1 to 2 cm2 defect or 50% of the orbital floor surface will result in enough orbital volume increase to result in clinically significant enophthalmos.2,3
Diplopia associated with entrapment
Entrapment with positive forced duction test. Extraocular muscles recover better if surgically released within 48 hours.
Persistent oculocardiac reflex may be associated with soft tissue entrapment. Patients who benefit from early surgical intervention are those presenting with nausea, vomiting, and bradycardia, exacerbated with upward gaze.2
Preoperative Planning
Complete review of the chart including medications is important, particularly anticoagulants.
If long-acting dilating eye drops are used by ophthalmology, it is generally recommended to wait before taking the patient to the operating room. Pupil diameter is assessed preoperatively. If a pupil dilates intraoperatively, it is often secondary to excess retraction. This phenomenon cannot be observed in patients with pupils pharmacologically dilated.
If the patient has a retrobulbar hematoma, clearance from ophthalmology prior to surgery is recommended.
A thorough eye examination should be performed by the plastic surgeon and documented in the chart preoperatively.5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree