1 Comprehensive lower extremity anatomy
Synopsis
 The reconstructive surgeon who embarks on surgery on the lower extremity must be well acquainted with its complex anatomy.
The reconstructive surgeon who embarks on surgery on the lower extremity must be well acquainted with its complex anatomy.
 The essence of reconstructive surgery is using one’s thorough knowledge of the nuances of the anatomical structures to enable borrowing from one or more structures to reconstruct the loss of others.
The essence of reconstructive surgery is using one’s thorough knowledge of the nuances of the anatomical structures to enable borrowing from one or more structures to reconstruct the loss of others.
 This chapter aspires to provide a comprehensive review of the anatomical structures from the hip through to the plantar surface of the foot in order to provide the basis of mastery of lower-extremity reconstruction.
This chapter aspires to provide a comprehensive review of the anatomical structures from the hip through to the plantar surface of the foot in order to provide the basis of mastery of lower-extremity reconstruction.
 The components of the lower extremity vary widely in regard to the redundancy of tissue, density of distinct structures, and function as one travels from proximal to distal regions. It is for this reason that the anatomical depiction of the lower extremity is divided into discussion of the thigh, knee, lower leg, and foot. Each of these structures differs greatly from each other. However, many reconstructive tasks bridge and cross these regions.
The components of the lower extremity vary widely in regard to the redundancy of tissue, density of distinct structures, and function as one travels from proximal to distal regions. It is for this reason that the anatomical depiction of the lower extremity is divided into discussion of the thigh, knee, lower leg, and foot. Each of these structures differs greatly from each other. However, many reconstructive tasks bridge and cross these regions.
 Even though present in discrete sections, the anatomy of the lower extremity should be viewed as an interconnected and interrelated unit.
Even though present in discrete sections, the anatomy of the lower extremity should be viewed as an interconnected and interrelated unit.
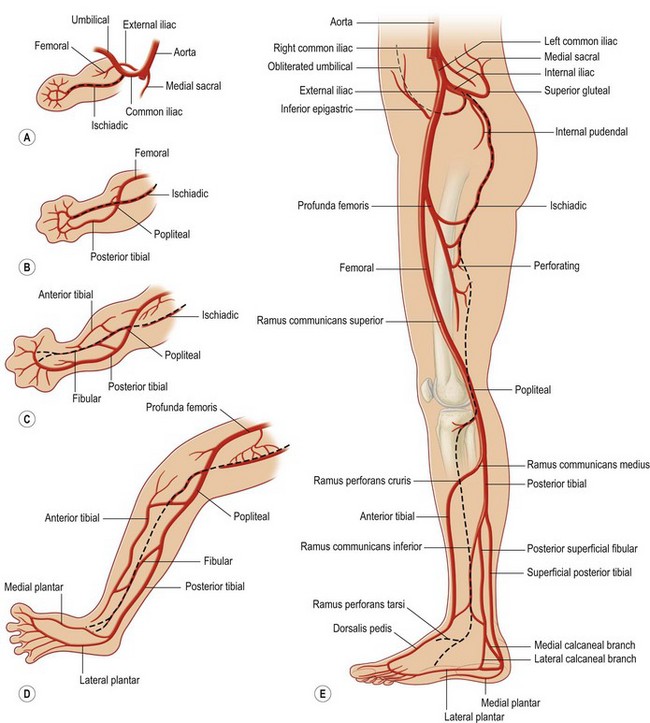
Embryology
The lower extremity vascular anatomy of the embryo differs from the adult primarily by the development and transient presence of the sciatic artery (also called the axis or ischiadic artery). This artery arises from the umbilical artery and is separate from the femoral artery as it courses inferiorly along the posterior surface of the thigh, knee, and leg and is a major contributor to lower extremity vascular supply in early fetal development. The femoral artery passes along the anterior side of the thigh and branches into the primitive posterior tibial and peroneal artery and an anterior tibial artery. As the fetus grows, the femoral artery increases in size and the sciatic artery becomes attenuated. In normal development the sciatic artery involutes during the eighth week of gestation and its remnants contribute to the formation of the inferior gluteal, deep femoral, popliteal, and peroneal vessels (Fig. 1.1). However, in 0.025–0.04% of the population a sciatic artery persists throughout fetal development and into adulthood. A persistent sciatic artery can lead to aneurysm formation, thrombosis, and embolization. Although it is a rare anomaly, failure to recognize a persistent sciatic artery can lead to inappropriate assumptions of vascular patterns to common lower extremity flaps.
The gluteal region
Gluteal skeletal structure
The pelvis consists of the two paired hip bones and the midline sacrum, articulating together at the two sacroiliac joints. The hip bones are formed by the fusion of the ilium, pubis, and ischium. These three bony regions of the pelvis coalesce to form the acetabulum (Fig. 1.2). The complex bony structure of the pelvis serves to cradle the abdominal organs during upright ambulation, and the large thick bony prominences of the pelvis serve as muscle attachments for the muscles of the hip and thigh. Dense ligaments reinforce the pelvis and distribute the numerous opposing forces acting on it. The sacrospinous ligament runs from the sacrum to the ischial spine, bounding the greater sciatic foramen. The sacrotuberous ligament attaches the sacrum to the ischial tuberosity and encloses the lesser sciatic foramen. Running from the anterior superior iliac spine to the pubic tubercle is the inguinal ligament. Most of the muscles of the thigh originate from the bony pelvis (Fig. 1.3). The action of the multiple flexors, extensors, and internal and external rotators on the hip joint serves to stabilize and position the torso during the complex process of ambulation.
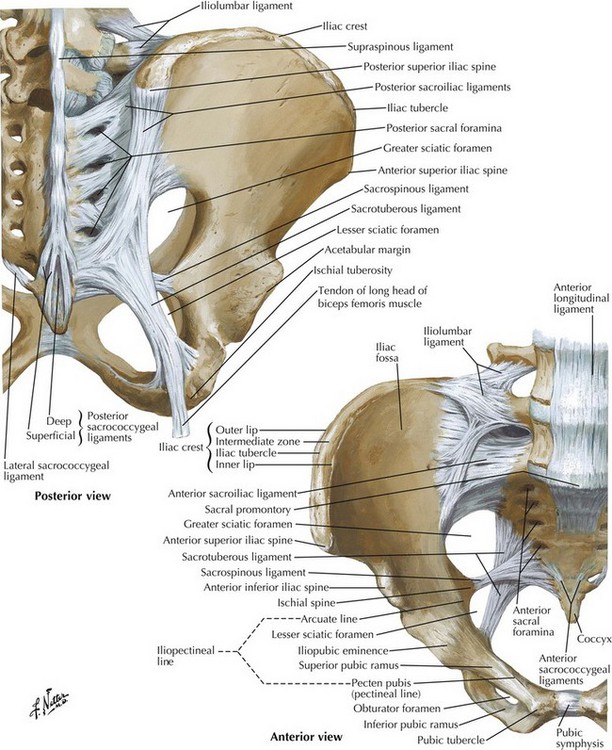
Fig. 1.2 Bones and ligaments of pelvis.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
Muscles of the buttocks
The gluteus maximus is the largest muscle in the body and lies most superficially in the gluteal region, originating from the posterior gluteal line of the ilium and the dorsal portion of the sacrum (Fig. 1.4). The superficial fibers coalesce into a thick tendinous expansion which contributes to the iliotibial band of the fascia lata, while the deep fibers insert on the gluteal tuberosity of the femur. The gluteus maximus acts as a hip extensor when the hip is in a flexed position. When the lower extremity is fixed in position – as in standing – the gluteus maximus dorsally rotates the pelvis and torso. The vascular supply is primarily derived from the inferior gluteal vessels, which supply the inferior two-thirds of the muscle. The superior gluteal vessels supply the superior portion and the first perforator branch of the femoral profunda contributes to the vascular supply of the muscle laterally. For ease of description, the Mathes–Nahai classification system is used when discussing the vascular supply to muscle in this chapter (Table 1.1). The vascular supply of gluteus maximus with two dominant pedicles (superior and inferior gluteal arteries) is considered to be type III.
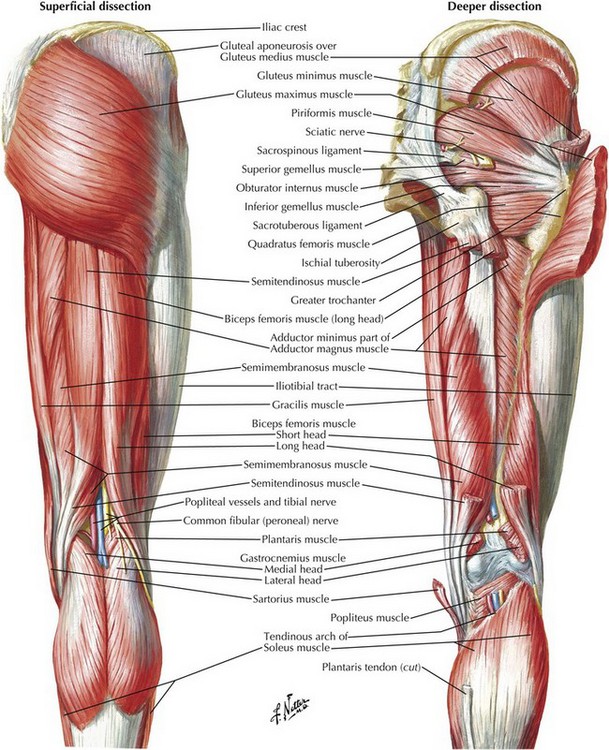
Fig. 1.4 Muscles of hip and thigh: posterior views.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
Table 1.1 Mathes–Nahai classification system for muscle vascular supply
| Muscle vascular supply type | Description |
|---|---|
| I | Single vascular pedicle |
| II | Dominant vascular pedicle and one or more minor pedicles |
| III | Two dominant pedicles |
| IV | Segmental vascular pedicles |
| V | Single dominant vascular pedicle and secondary segmental pedicles |
Gluteal vasculature
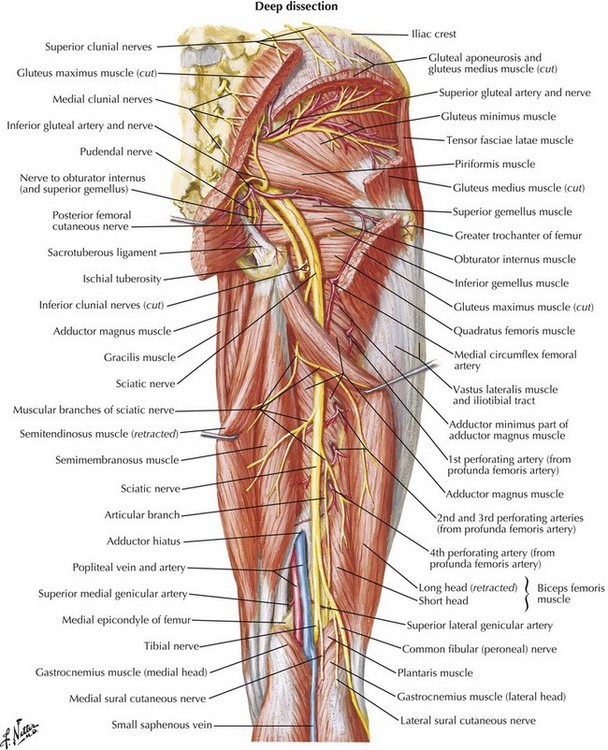
The superior gluteal artery is the last branch of the posterior trunk of the internal iliac artery. It exits the pelvis through the greater sciatic foramen superior to the piriformis, dividing into two branches (Fig. 1.5). The deep branch runs deep to the gluteus medius, dividing into superior and inferior branches. The superior branch travels laterally to the anterior superior iliac spine and connects with the ascending branch of the lateral circumflex femoral and the deep circumflex iliac. The inferior branch supplies the gluteus medius and minimus, and later joins with the lateral circumflex femoral. The superficial branch of the superior gluteal artery pierces the gluteus maximus, connecting intramuscularly with branches of the inferior gluteal artery, and sending musculocutaneous perforators to the overlying skin. The inferior gluteal artery branches from the anterior trunk of the internal iliac and exits the pelvis through the greater sciatic foramen below the piriformis. It runs deep to the gluteus maximus, supplying it and its overlying skin with musculocutaneous perforators. The artery continues down the posterior thigh, connecting with the perforating branches to supply the skin.
Gluteal innervation
The posterior cutaneous nerve of the thigh exits the pelvis with the inferior gluteal vessels (Fig. 1.5). Several branches will curl around the inferior border of the gluteus maximus and run superiorly to innervate the overlying skin of the buttocks, while the posterior cutaneous nerve continues to descend down the posterior thigh deep to the fascia lata, sending segmental cutaneous branches to the skin of the posterior thigh. The gluteal muscles are innervated by the superior and inferior gluteal nerves. The superior gluteal nerve runs with the superior gluteal artery and divides into superior and inferior branches, which course respectively with the superior and inferior branches of the deep superior gluteal artery, supplying the gluteus medius and minimus. The inferior branch runs laterally to also innervate the tensor fascia latae. The inferior gluteal nerve runs with the inferior gluteal artery, exiting the pelvis below the piriformis and entering the gluteus maximus.
The thigh
Thigh skeletal structure
The femoral head articulates with the pelvic acetabulum to form the only true ball-and-socket joint in the body, allowing for stability under load as well as smooth multiplanar movement. A dense ligamentous capsule surrounds the hip joint circumferentially, extending from around the pelvic acetabulum to encase the femoral head and insert on the femoral neck (Fig. 1.6). The ligaments of the hip joint are the iliofemoral, pubofemoral, ischiofemoral, transverse acetabular and the ligamentum teres. As the hip moves, so do the capsular ligaments. The ligaments are reinforced with capsular thickenings which wind and unwind, tightening around the hip, affecting stability, excursion, and joint capacity.
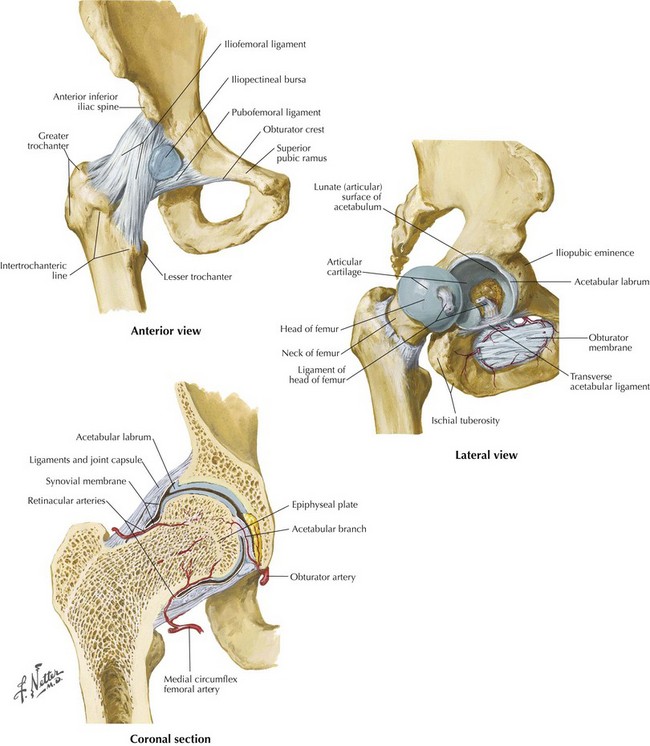
Fig. 1.6 Joints and ligaments of the hip.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
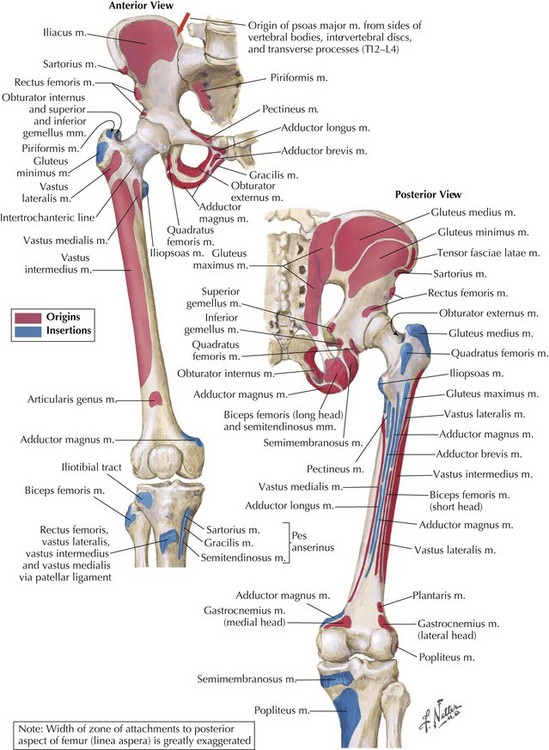
The pelvic bone serves as the principal base for the thigh musculature. Eleven out of the 17 muscles of the thigh originate from the pelvis. Two bony prominences emanate from the femoral neck at about 90° from each other – the greater and lesser trochanters. These femoral prominences primarily serve as insertion sites for hip actors (Fig. 1.3). The greater trochanter receives insertions from the quadratus femoris, gluteus medius, obturator externus, piriformis, obturator internus, and gemellus muscles. The lesser trochanter is the insertion target for the iliopsoas muscle. The action of multiple flexors, extensors, and internal and external rotators on the hip joint serves to stabilize and position the torso during the complex process of ambulation.
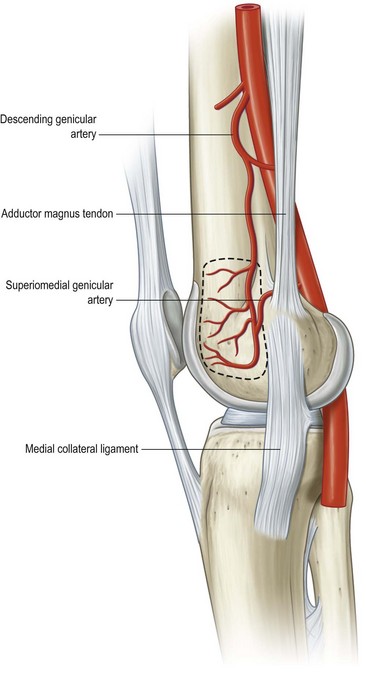
The vascular supply of the femoral bone arises from multiple sources. The femoral head and neck are encircled by an arterial-connecting arcade contributed by the medial and lateral circumflex arteries with lesser contribution by the superior and inferior gluteal vessels. These vessels piece the hip joint synovial capsule and form a subsynovial intra-articular ring. The femoral shaft has multiple nutrient foramina via which branches from the second perforating artery from the profunda femoris (Fig. 1.7) enter and deliver endosteal blood supply. These foramina usually run along the linea aspera (Latin for “rough line”) on the posterior surface of the femur in the middle one-third of the femoral shaft. Periosteal vascularity along the femur receives vascular input from either the perforating branches of the profunda or directly from the profunda femoris. The distal metaphyseal region of the femur also has multiple vascular foramina that are derived from the genicular arterial system.
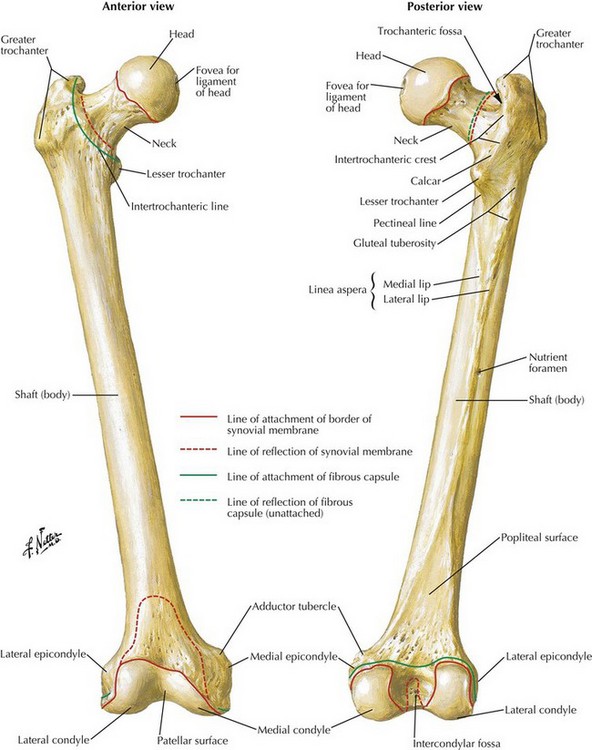
Fig. 1.7 Osteology of the femur.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
This genicular system, based on the superficial femoral artery, is the anatomical basis for the clinically relevant medial femoral periosteal bone flap. Using the descending genicular artery (a medial branch of the superficial femoral artery) as a pedicle, perisosteum, cortical and cancellous bone can be harvested from the medial femur as a vascularized flap. Usually used as a free flap (with or without an associated skin paddle off the saphenous artery), the medial femoral periosteal bone flap is utilized as an effective treatment for recalcitrant bony nonunions of the clavicle, humerus, tibia, and radius (Fig. 1.8).
Thigh fascial composition
The deep fascia structure of the lower extremity is a tough, well-vascularized fibrous tissue that lies beneath the superficial fascia and all the subcutaneous fat. This fibrous structure encircles and constrains the thigh musculature in a near-complete sheath, often found to be dual layers. The deep fascia of the thigh has been referred to and described by several different names, making the terminology somewhat confusing. The deep fascia of the thigh is also called investing fascia of the thigh; the fascia lata (lata, Latin for wide or broad); or, even more confusingly, the “thick layer of the superficial fascia.” The deep fascia of the thigh attaches posteriorly to the sacrum and coccyx, anteriorly to the inguinal ligament, and laterally to the iliac crest. At the inguinal ligament, where the superficial fascia joins the deep fascia, lies the fossa ovalis. The fossa ovalis is an opening in both fascial layers through which the great saphenous vein, superficial branches of the femoral artery, and lymphatics pass through, transitioning between the deep and the superficial layers of the thigh (Fig. 1.9). This opening is covered by a membranous layer of the superficial fascia called the cribriform fascia (derived from the Latin cribrum or sieve). A thickening of the fibrous tissues is present on the lateral aspect of the deep fascia (fascia lata) which is called the iliotibial band or tract (Fig. 1.10). The iliotibial band is proximally attached to the tensor fascia latae muscle and together this myofascial unit aids in maintaining knee extension.
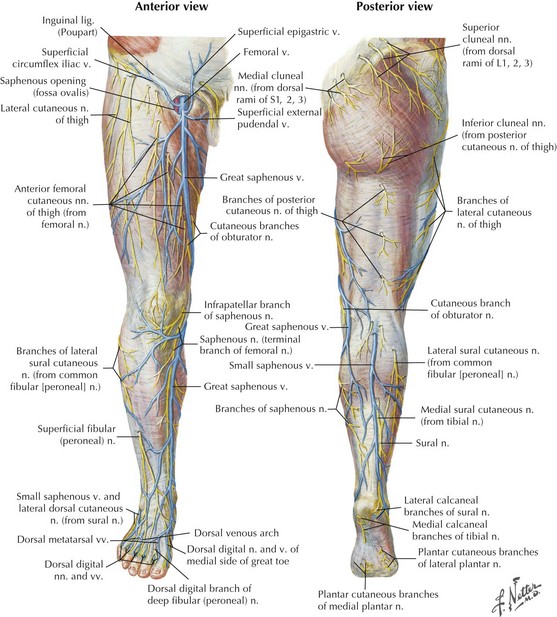
Fig. 1.9 Surface anatomy: superficial veins and nerves.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
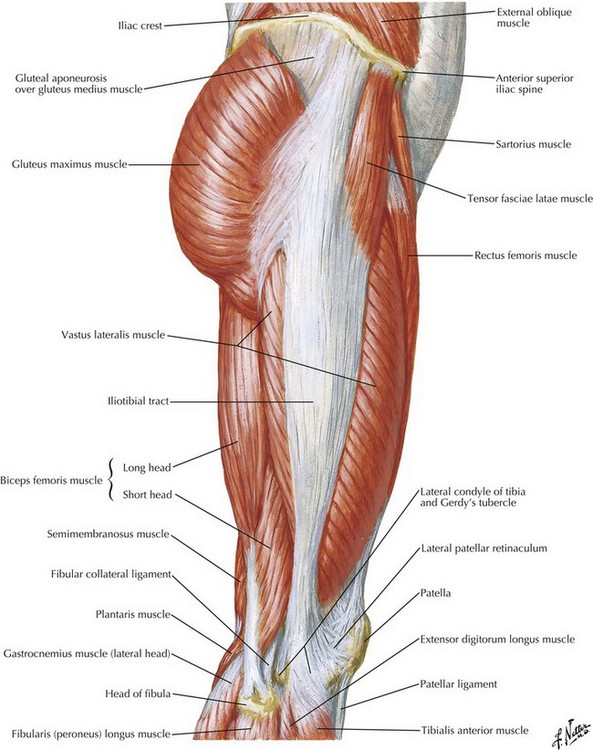
Fig. 1.10 Muscles of hip and thigh: lateral view.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
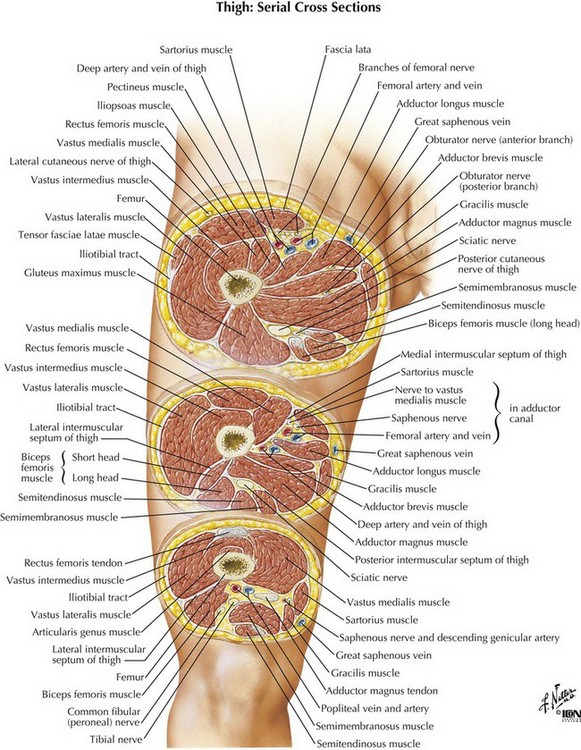
There are three functional compartments of the thigh: anterior, posterior, and medial. The anterior compartment contains the knee extensor muscles; the posterior compartment is comprised of knee flexors; and the medial compartment retains the hip adductors (Fig. 1.11). The medial and lateral intermuscular septa travel from the fascia lata to attach to the femur on the linea aspera along its posterior aspect. These septa then divide the anterior compartment from the posterior compartments and partition the thigh musculature according to knee function. Only the anterior and posterior compartments have definite fascial boundaries. The medial (adductor) compartment is not a true anatomical compartment as it has no defined intermuscular septa separating it. The muscles of the adductor compartment – gracilis, pectineus, adductor longus, adductor brevis, and adductor magnus – form a functional compartment in the proximal aspect of the thigh.
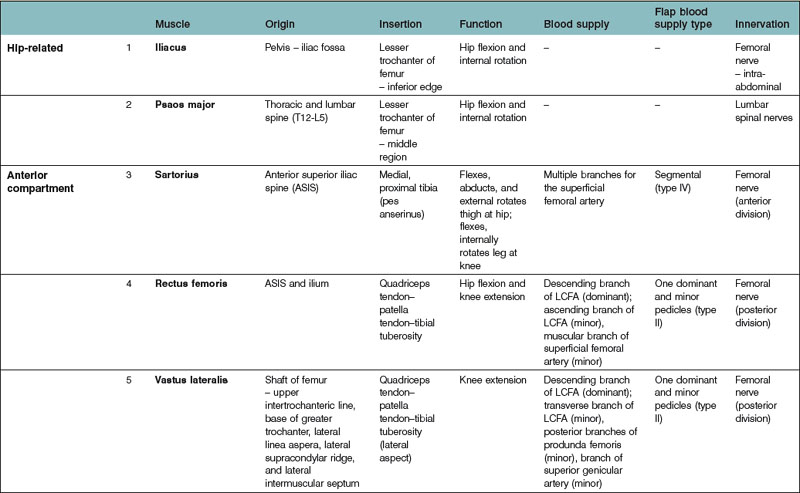
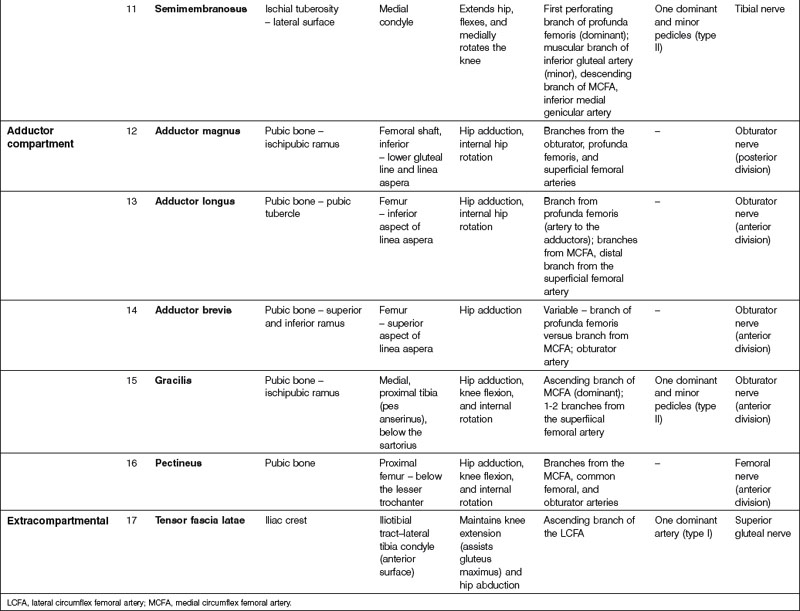
Thigh musculature
The three compartments of the thigh are a well-organized way to approach the thigh musculature (Table 1.2). The anterior thigh compartment contains the sartorius, articularis genu, and quadriceps femoris, comprised of the rectus femoris, vastus lateralis, intermedius, and medialis (Table 1.3). These muscles are the primary knee flexors. All of the anterior-compartment musculature is monoarticular functioning, with the exception of the sartorius and the rectus femoris, which crosses both the hip joint and the knee joint. These muscles are therefore biarticular muscles and flex both the hip and knee joints.
Table 1.3 Anterior thigh compartment musculature
| Muscle | Function |
|---|---|
| Sartorius | Flexes, abducts, and external rotation of thigh at hip |
| Flexes and internally rotates leg at knee | |
| Rectus femoris | Hip flexion and knee extension |
| Vastus lateralis | Knee extension |
| Vastus medialis | Knee extension, patellar stabilization |
| Vastus intermedialis | Knee extension |
| Articularis genu | Retracts bursa as knee extends |
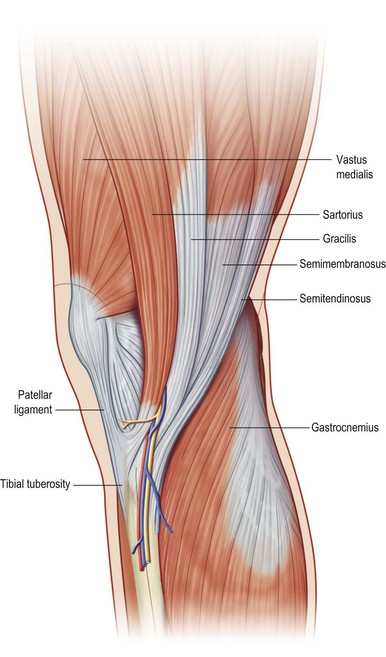
The sartorius muscle is the most superficial muscle of the thigh. It obliquely crosses the anterior thigh from superolateral to medial inferior. The proximal end of the sartorius makes up one of the three limbs of the femoral triangle. The medial border of the sartorius makes up the lateral side; the medial border of the adductor longus makes up the medial side of the triangle; and the inguinal ligament makes up the superior limb (Fig. 1.12). The femoral triangle denotes the region where the femoral artery, nerve, and vein are transiently uncovered superficially by muscle in the proximal thigh. Here, all three structures radiate multiple branches in multiple directions to supply the vasculature and innervation to the groin region, lower abdomen, and proximal thigh. As the femoral artery, vein, and nerve descend distally in the thigh, they dive under the adductor longus and then proceed to the adductor canal. At the distal end of the sartorius, the muscle inserts on the proximal, medial surface of the tibia. The sartorius inserts in this region above the gracilis, which then inserts above the semitendinosus (Fig. 1.13). This three-muscle insertion point forms the pes anserinus (a Latin derivation for “duck’s foot”) which is so named because of the three-toed pattern of the duck’s foot. The sartorius’ superficial and femoral triangle proximity location makes it an ideal candidate for muscle transposition coverage over proximal thigh wounds with femoral vessel exposure. It has a type IV segmental blood supply but there exist more dominant segmental pedicles which allow for adequate vascular pivot points. In addition, partial sartorius muscle transfer can be effectively utilized to ensure vascular supply and close complex proximal thigh wounds.
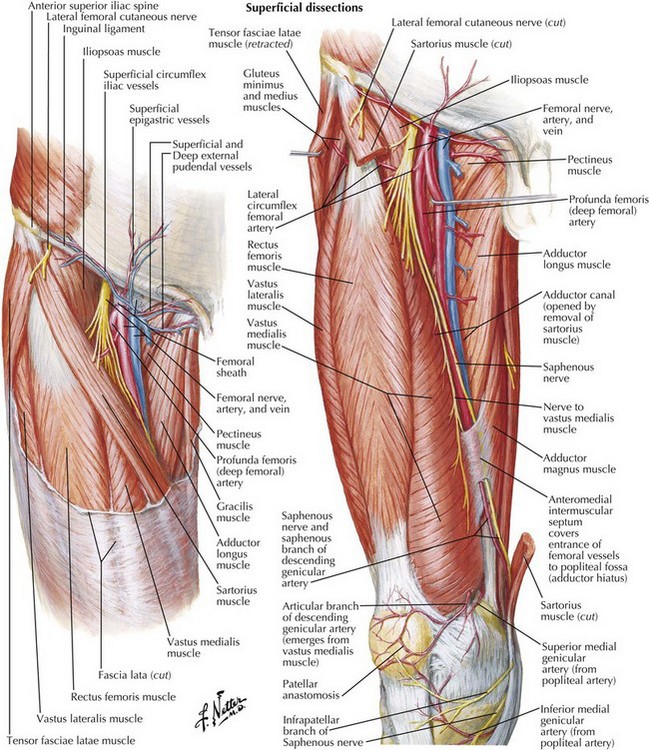
Fig. 1.12 Arteries and nerves of thigh: anterior views.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
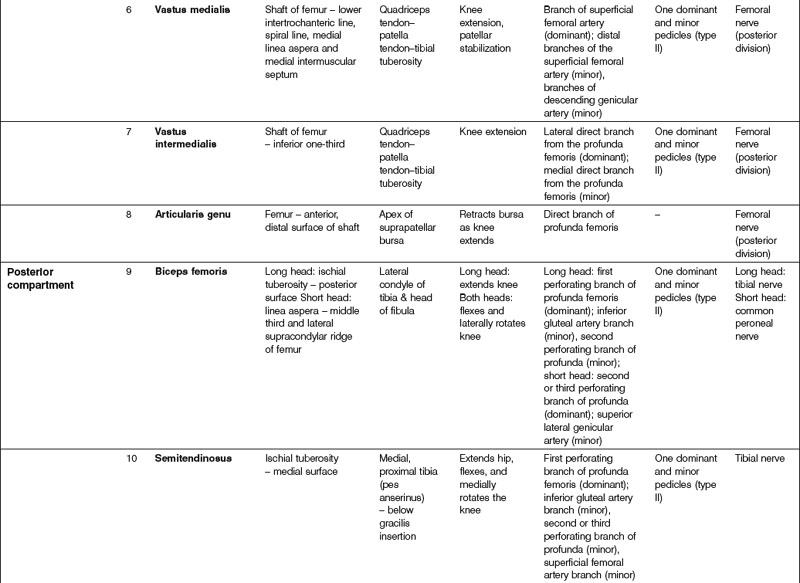
The posterior compartment musculature is comprised of the knee flexion muscles, colloquially known as the hamstrings (termed referring to the posterior thigh culinary cut of the hog – ham) (Table 1.4). The three muscles of this compartment facilitate knee flexion. The biceps – as its name denotes – has two heads, each with a slightly different origin and action. All three of these muscles span the posterior knee, with the tendons of the semitendinosus and semimembranosus traveling medially and forming one border of the popliteal fossa and the biceps femoris tendon traveling laterally and forming the other border (Fig. 1.14).
Table 1.4 Posterior thigh compartment musculature
| Muscle | Function |
|---|---|
| Biceps femoris | Long head: extends knee |
| Both heads: flexes and laterally rotates knee | |
| Semitendinosus | Extends hip, flexes and medially rotates the knee |
| Semimembranosus | Extends hip, flexes and medially rotates the knee |
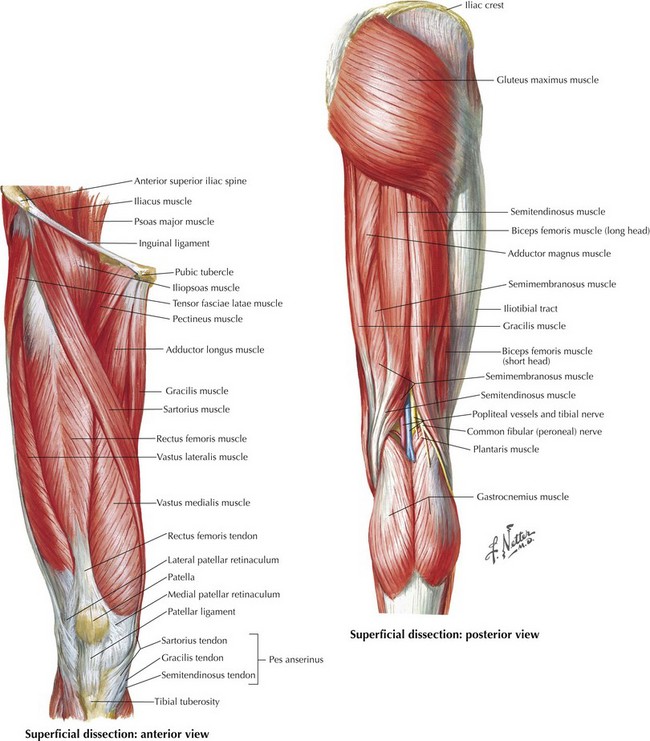
Fig. 1.14 Muscles of the thigh.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
The adductor compartment houses the adductor magnus, brevis, and longus, as well as the gracilis and pectineus (Figs 1.15 and 1.16 and Table 1.5). All five muscles cross the hip joint but only one – the gracilis – crosses the knee. The gracilis is also the most superficial muscle of the adductor compartment. It begins from its origin on the pubic bone as a flat, broad muscle that tapers down into a narrow tendon that inserts into the pes anserinus. Because of its superficial location, its muscle vascular supply type II, and an associated vascular branch that leads to the overlying skin, the gracilis is a frequent choice for a muscle or musculocutaneous flap. Due to their position and musculature structure, the remainder of the adductor muscles do not lend themselves easily for flap transposition.
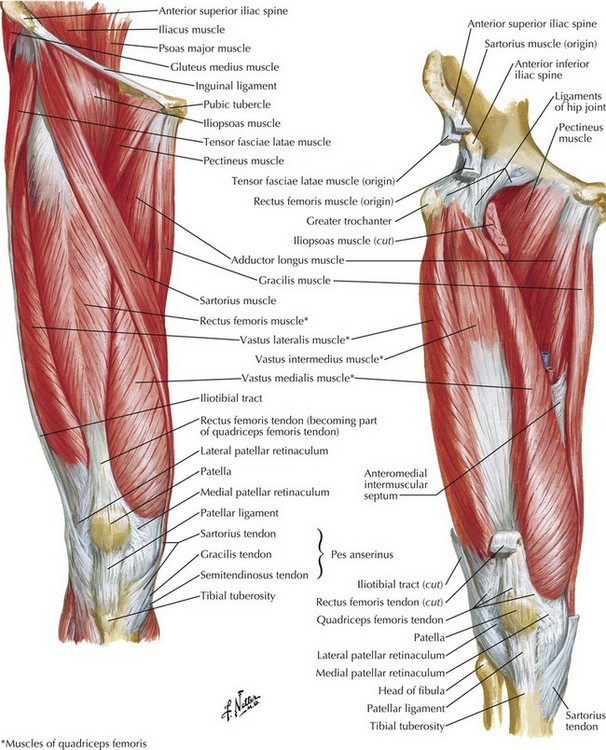
Fig. 1.15 Muscles of thigh: anterior view.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
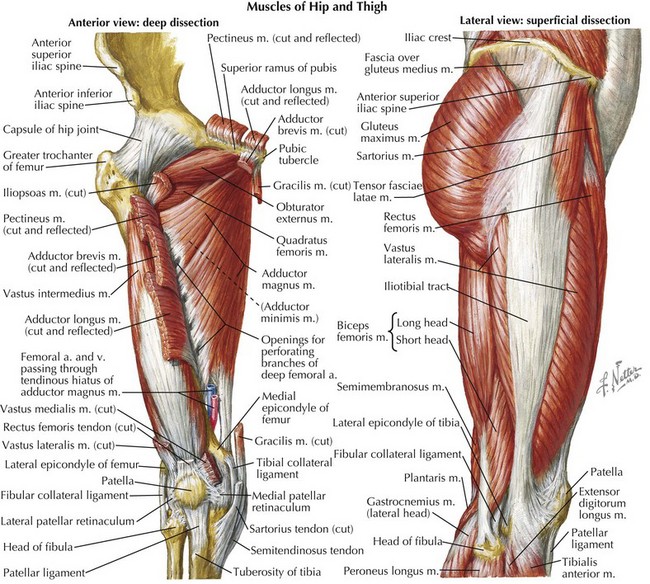
Fig. 1.16 Muscles of the thigh, deep dissection: anterior view.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
Table 1.5 Adductor compartment musculature
| Muscle | Function |
|---|---|
| Adductor magnus | Hip adduction, internal hip rotation |
| Adductor longus | Hip adduction, internal hip rotation |
| Adductor brevis | Hip adduction |
| Gracilis | Hip adduction, knee flexion, and internal rotation |
| Pectineus | Hip flexion, adduction, and internal rotation |
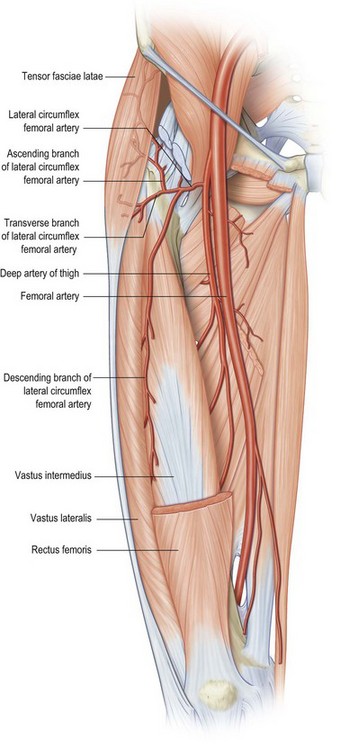
The tensor fascia latae is not classically designated in the previously described compartments but included in the discussion of the thigh because of its intimate relation to thigh musculature and it utility in thigh reconstructive options. The tensor fascia latae lies on the proximal lateral aspect of the thigh originating from the iliac crest. As it descends distally, it is enveloped by the two layers of the iliotibial band of the fascia lata (Figs 1.10 and 1.12). The tensor fascia latae muscle usually ends in the first third of the thigh but can extend down to the lateral femoral condyle. Its blood supply is from the ascending branch off the lateral circumflex femoral arterial system. This allows the muscle and fascia to be included with other flaps based off the same system if such a composite reconstruction is required. Also, with dissection to the branch to the source lateral circumflex femoral vessels, the tensor fascia latae with its long iliotibial band can be used to reconstruct other fascial defects in nearby regions such as the abdomen.
Thigh vasculature
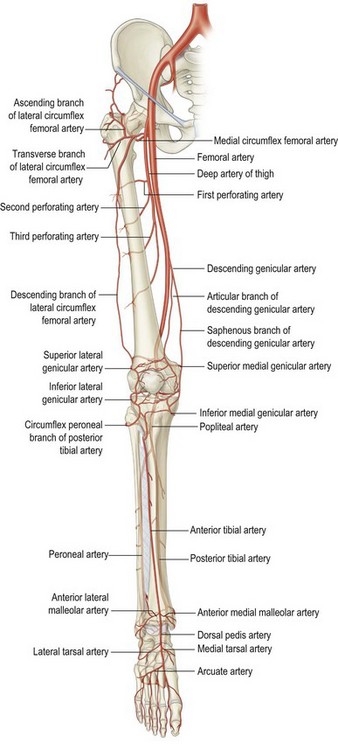
The primary blood supply to the entire lower extremity is the femoral artery, passing beneath the inguinal ligament into the femoral canal (Fig. 1.17). It courses with the femoral vein through the femoral sheath, a short canal composed of continuation of the transversalis fascia anteriorly and the iliac fascia posteriorly. These fascial layers fuse with the vascular adventitia approximately 4 cm inferior to the inguinal ligament. The femoral artery crosses beneath the sartorius muscle and enters Hunter’s canal, a fibromuscular canal bounded laterally by the vastus medialis, inferiorly by the adductor longus and magnus, and anteromedially by the sartorius. The femoral artery exits Hunter’s canal through the adductor hiatus, entering the popliteal fossa, at which point its name changes to the popliteal artery.
In the proximal thigh, the femoral artery bifurcates 4 cm inferior to the inguinal ligament into the profunda femoris (also called the deep femoral artery) and the superficial femoral artery. Although there is some debate over the terminology of the femoral artery’s origin and distal progression, it is usually described as follows: the external iliac artery becomes the femoral artery after it crosses the inguinal ligament, then the femoral artery branches into the profunda femoris and the superficial femoral artery. The profunda femoris usually branches from the posterolateral aspect of the femoral artery then passes deep to the adductor longus muscle, between the insertions of the lateral and medial intermuscular septa, and runs posterior to the linea aspera of the femur (Figs 1.11 and 1.18).
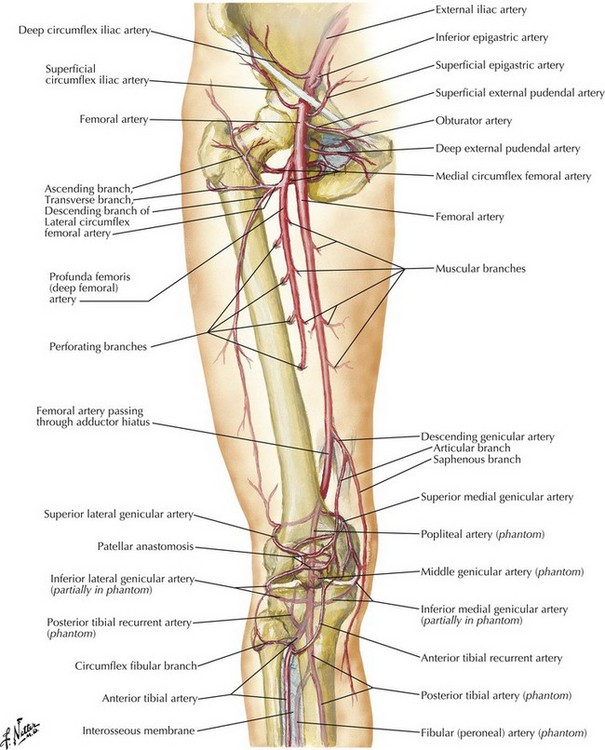
Fig. 1.18 Arteries of thigh and knee: schema.
(Netter illustration from www.netterimages.com. Copyright Elsevier Inc. All rights reserved.)
Profunda femoris
In the thigh, the profunda femoris is the predominant blood supply source. There are some important contributions to thigh musculature by the superficial femoral artery (the adductors, sartorius, and the vastus medialis) but the main vascular distribution for the three thigh compartment arises from the profunda femoris. The majority of the pedicles to thigh musculature arise in the proximal two-thirds of the thigh from the six major branches of the profunda femoris: the lateral and medial circumflex arteries and four perforating arteries (Fig. 1.18).
Lateral circumflex femoral arterial system
The lateral circumflex femoral arterial system is particularly relevant to the reconstructive surgeon due to the number of harvest tissue options that have been developed based on it. The traditional description of the lateral circumflex femoral artery is as the second major branch of the profunda femoris that winds superolaterally and divides into three branches at the lateral border of the femoral triangle, namely, the ascending, transverse, and descending branch (Fig. 1.19). The ascending branch travels along the intertrochanteric line, supplying the greater trochanter, the tensor fascia latae, anterior iliac crest, and the skin overlying the hip before connecting with the superior gluteal and deep circumflex iliac vessels. The transverse branch passes through the vastus lateralis and curls posteriorly around the femur, joining with the medial circumflex. The descending branch usually travels in the intermuscular septum between the vastus intermedius and the overlying rectus femoris. From these branches, cutaneous perforators either travel through the musculature (musculocutaneous perforators) or between the musculature along the intervening fibrous septa (septocutaneous perforators).
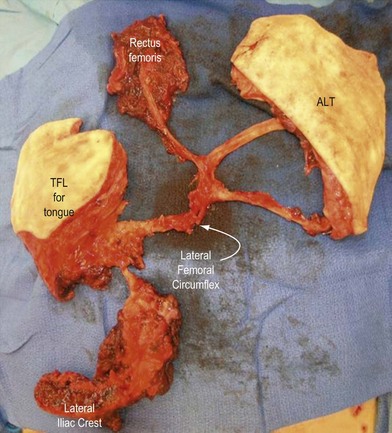
In spite of this multiplicity of anatomic variations, this system provides a robust interconnected blood supply to skin, muscle, fascia, and bone. This can be exploited for a plethora of flap compositions in a variety of orientations. In the particularly complex wound, the harvest of lateral circumflex femoral artery system can be designed to encompass composite flaps with multiple tissue types. If the lateral circumflex femoral artery system is properly dissected, a composite flap or rectus femoris, anterolateral skin and fascia, tensor fascia latae muscle, and iliac crest bone can be fashioned (Fig. 1.20).