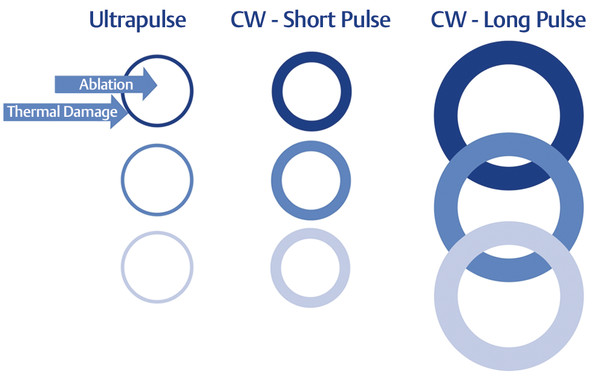
Why Complications Occur Complications occur as a result of different factors, some controllable and others unpredictable. To better understand the intrinsic risk of any ablative treatment, laser–tissue interaction and the requirements of efficient tissue ablation should be reviewed. When skin is treated with a 10,600-nm CO2 laser beam, water in the skin is heated to 100°C and the heated tissue is vaporized. The heat conducted to adjacent tissue results in a zone of coagulation necrosis at a depth and width dependent on the fluence and dwell time (time for the pulse to be delivered). Fluences greater than 4 to 5 J/cm2 applied in ≤ 1 ms, the thermal relaxation time (TRT) of human skin, are necessary to ablate the epidermis.10 When dwell time exceeds the TRT of skin, the surrounding tissue undergoes prolonged, less efficient heating that may result in unexpected and undesired effects including superheating of tissue and char formation. For the CO2 laser the accepted dwell time or pulse duration to achieve ablation without superheating the surrounding tissue is approximately 0.7 ms. In order for any ablative device to reach a given depth, the length of exposure is increased in the continuous wave (CW) laser, or the number of pulses is increased in the pulsed laser. When the pulse duration is increased beyond the TRT of skin and the thermal effect of the laser–tissue interaction outpaces the velocity of ablation, the result is wider zones of thermal injury. This unseen effect of prolonged pulse width alters treatment density significantly, as illustrated by ▶ Fig. 19.1. Fig. 19.1 The effect of pulse duration on treatment density in fractional carbon dioxide (CO2) laser resurfacing. Each circle represents a microthermal wound created by the fractional laser beam. The pulse duration is shortest with the ultrapulse and longest with the long-pulse continuous wave (CW) laser. The circumferential lines represent the areas of thermal damage (i.e., thick lines denote greater thermal damage than thin lines). As the pulse duration increases, the circumferential lines become thicker, the areas of thermal damage increase, and the treatment density increases. At the long pulses the wound areas begin to overlap, resulting in further increases in thermal damage. At this stage the treatment has become fully ablative (i.e., 100% density). This effect is believed to account for the unexpected adverse effects at long pulse durations of fractional resurfacing procedures. (Reproduced with permission from Duplechain JK. Neck rejuvenation: surgical and non-surgical. Facial Plast Surg Clin of North Am. 2014; 22(2): 2003–2016.) The effect of multiple pulses and pulse width (single, double, or long) within the TRT of skin also deserves discussion. Current fractional lasers permit users to deliver single or multiple pulses over the same area. In a 15-patient study, Bailey and colleagues11 showed that the mean penetration depth of single-pulse fractional CO2 laser energy was greater in abdominal skin (mean 582 μm) than in facial skin (mean 415 μm). Data are presented in ▶ Table 19.1. In a subsequent study using a fractional CO2 laser, Oni et al12 compared penetration depths of the same anatomical areas using a single pulse of 30-mJ energy in both areas versus a double pulse of 15-mJ energy in both areas (▶ Table 19.1). The collective data of the two studies revealed several important relationships. With a single pulse at 15 mJ, depths of injury of facial and abdominal skin (415 and 582 μm, respectively) were similar. With double pulsing at 15 mJ, injury to abdominal skin (822 μm) was more superficial than with a single pulse at 30 mJ (1,345 μm). The difference in depths was 523 μm. A similar comparison for facial skin shows a much smaller difference (881 μm – 854 μm = 27μm), suggesting that laser injury patterns in facial and abdominal skin are not the same. The widths of laser-induced injury in the face and abdomen were also measured. The data showed that for facial skin, the widths of injuries induced by double and single pulses (493 and 312 μm, respectively) at 15 mJ differed by 181 μm, much larger than the 27 μm observed for facial injury depths. When facial injuries induced by single pulses at 30 and 15 mJ were compared, the difference in widths was even larger (534 μm – 312 μm = 222 μm). Pulse Energy (mJ) Mean MTZ depth (μm) Mean MTZ width (μm) Face Abdomen Face Single 15a 415a 582a 312a 30b 854b 1,345b 534b Double 15b 881b 822b 493b Data from: MTZ, microthermal zone. (a) Bailey SH, Brown SA, Kim Y et al. An intra-individual quantitative assessment of acute laser injury patterns in facial versus abdominal skin. Lasers Surg Med 2011; 43: 99–107 (b) Oni G, Robbins D, Bailey S, Brown SA, Kenkel JM. An in vivo histopathological comparison of single and double pulsed modes of a fractionated CO(2) laser. Lasers Surg Med 2012; 44: 4–10 This information is presented to demonstrate that lasers operating well within accepted guidelines of efficient skin ablation can still be problematic―especially for different anatomical areas―when higher energy single-pulsed or multipulsed parameters are utilized. A thorough understanding of the effects of varying parameters is key to delivering safe, uncomplicated treatments. The proper selection of patients for laser resurfacing requires input from the patient and the provider. The provider must know the limitations of the instrument being utilized, and whether this tool is capable of delivering the results the patient is seeking. The adage of “under promise and over deliver” is as true in skin rejuvenation as in any procedure performed. Resurfacing can commonly be performed as an adjunct to other procedures such as facelift, blepharoplasty, or other cosmetic processes; however, consideration to which techniques have already been performed is vital to administering safe adjunctive laser resurfacing. The probability of complications should be carefully evaluated in potential candidates for laser resurfacing. Patients of all skin types are suitable for CO2 laser resurfacing.13 Specific risks are often associated with a particular skin type and should be discussed individually. For example, patients with Fitzpatrick skin type IV and above should be counseled more so about the possibility of hyperpigmentation. Patients with a thick epidermis and dermis will see improvement in texture but are unlikely to see as much skin tightening as a patient of northern European ancestry (Fitzpatrick skin type I, with a thin epidermis). Patients may have conditions or lifestyles for which laser treatment is contraindicated. Such contraindications may be relative or absolute and vary with the practitioner’s experience. In general, patients are typically not treated if they cannot avoid sun exposure for at least 1 week. After 1 week, patients may apply a physical sunblock with a titanium or zinc base and resume daily (but reduced) sun exposure. They are advised to minimize sun exposure for about 3 weeks and to avoid extended exposure for 6 weeks. Since this restriction may be problematic, patients who request more aggressive resurfacing are usually treated during the winter period. Subjects with ongoing acne or active skin infection are not treated. The acne should be stable and in remission for at least 3 months before CO2 treatment. Resurfacing subjects with an active skin infection could result in severe and serious complications including cellulitis and severe scarring. All patients with or without a history of herpes simplex virus (HSV) are treated prophylactically with an antiviral medication and continued until re-epithelialization has occurred. Absolute contraindications for ablative skin resurfacing include isotretinoin use within 1 year of the desired procedure, history of keloid formation, immunosuppression (acquired or drug-induced) and neuropsychosis (e.g., facial picking). Although cosmetically unacceptable to patients, postoperative erythema is part of healing14 and is expected after CO2 laser resurfacing10 in all patients.2,15 Diffuse persistent erythema may be associated with allergic or irritant contact dermatitis (▶ Fig. 19.2)16,17 and superficial infections17 including bacterial or fungal. Fig. 19.2 A 61-year-old woman who underwent carbon dioxide (CO2) resurfacing and was treated with a petrolatum aftercare product. The erythema and pustules are often associated with this type of product. The residual thermal damage or heating with either a CO2 or Er:YAG laser treatment is most likely responsible for prolonged erythema. Single-pass ablative treatments alone are unlikely to result in significant erythema unless comorbidities such as infection occur. Ross and coworkers,18 in their 13-patient study of wrinkle reduction and adverse effects, compared microscopic and clinical injuries resulting from four-pass treatment with an Er:YAG laser and single-pass treatment with a CO2 laser. Periorbital and perioral areas of the face were treated on one side with the Er:YAG laser and on the other side with the CO2 laser. Both lasers produced ablation of 60 μm of the epidermis and residual thermal damage of the upper 20 μm of the dermis. These results showed that with the treatment parameters used in the study, a single pass with the CO2 laser produced injuries similar to those of four passes of the Er:YAG laser. Erythema was significantly less (p < 0.04) after 2 weeks on the CO2 laser-treated sides than on the Er:YAG-treated sides and the differences resolved 6 weeks after treatment. Tanzi and Alster,19 in their 100-patient study of subjects who underwent either single-pass CO2 or multiple-pass Er:YAG resurfacing, reported postoperative erythema persisting for 4.5 and 3.6 weeks, respectively. The pulse frequency can also contribute to the degree of erythema. High-frequency treatments reduce the treatment time, but when frequency rates approach the TRT of skin, overheating of the skin can occur. For example, at a frequency of 600 Hz, the laser fires every 1.5 ms. Cooling time between pulses is approximately 0.8 ms, assuming the pulse duration is 0.7 ms, the TRT of human skin. At 250 Hz, the cooling time is 3.3 ms, or 412.5% longer than the 0.8 ms cooling time at 600 Hz. This longer cooling time allows for some of the thermal component of the injury to dissipate before the next pulse is delivered. This helps prevent the buildup of heat, classically known as a heat sink. Some devices also provide random patterns of ablation so that no two pulses are adjacent. This may also help prevent excessive erythema. Transient erythema after treatment with a fractional laser8,9,20 and all types of nonablative treatments21 has been reported. Erythema persisting longer than 4 days on the face and longer than 7 days on the neck and chest has been noted in 1.1% of patients after ablative fractionated CO2 laser treatment.5 With fractionated resurfacing, erythema is considered prolonged if it persists longer than 4 days with nonablative treatments and longer than 1 month with ablative procedures. The risk of prolonged erythema after fractionated laser resurfacing increases with multiple passes and inadvertent pulse stacking.20 ▶ Fig. 19.3 shows a patient in whom erythema persisted more than 6 weeks after fractional CO2 laser resurfacing. The contributing factors were thought to be long pulse width and high density with inefficient ablation. Fig. 19.3 A 55-year-old woman who underwent fractional carbon dioxide (CO2) resurfacing. Cross marks and stamping effect of the fractional device are significant at 6 days after treatment. Erythema persisted more than 6 weeks due to high density and energy settings. Treatments of erythema include hydrocortisone 1% cream used sparingly and for a short time10 and, to reduce inflammation, topical ascorbic acid after re-epithelialization is complete.15,22 Hydrocortisone 2.5% cream and hydrocortisone valerate 0.2% cream have also been suggested for erythema and pruritus. Many physicians apply steroid creams after re-epithelialization has occurred because healing may be delayed if the steroid is given before re-epithelialization is complete.23 The use of topical steroid creams during the re- epithelialization following resurfacing has been implicated in increased infection rates.24 If scarring develops, intralesional triamcinolone 10 mg/mL or 5 fluorouracil along with pulsed dye laser treatment is recommended promptly because delay in treatment may lead to hypertrophic scarring.10,15 These treatment options may help reset healing by decreasing the production of collagen, reducing the amount of extracellular matrix deposition, and/or modulating certain growth factors implicated in wound healing.25 Intense pulsed light has been used successfully to remove erythema and hyperpigmentation after CO2 laser resurfacing of the periorbital area.26 Persistent erythema following laser resurfacing requires vigilant treatment because patients are often homebound for several months, resulting in significant dissatisfaction toward the physician. Hyperpigmentation occurs approximately 4 weeks after CO2 laser resurfacing in more than 30% of all patients and nearly 100% of dark-skinned patients.27 It may also occur in skin types I, II, and III, even without sun exposure.13 Hyperpigmentation is often due to inadvertent sun exposure shortly after laser treatment.28 The amount of heat deposited into the skin is considered a primary source of hyperpigmentation by many. Frequency, density, and prolonged heating of the skin all contribute to this problem (▶ Fig. 19.4). Since pigmentary changes may be emotionally disturbing, patients should be warned of this possibility before the procedure.22,28,29 Hyperpigmentation usually resolves within several months without treatment but may persist for 6 to 9 months.28 Resolution may be expedited with topical glycolic, retinoic, or azelaic acid; hydroquinone; light glycolic acid peels (30–40%); or both; and regular use of broad-spectrum sunscreens.22 The postoperative use of an antihyperpigmentation regimen (4% hydroquinone bleaching agent, kojic acid or mild lactic acid peeling, and sunscreen) has been shown to reduce the incidence of hyperpigmentation from 21 to 6%.14 Pretreatment with glycolic acid cream or hydroquinone with tretinoin cream appears to provide no reduction in incidence of hyperpigmentation after either CO2 or Er:YAG laser treatment,22 although this is controversial.13,15 However, patients should apply sunscreen with 15 or higher sun protection factor at least 4 weeks before resurfacing and continue regular use after treatment to maintain their clinical improvement.22 Fig. 19.4 (a) A 32-year-old, Fitzpatrick skin type IV woman who underwent fractional CO2 laser resurfacing 3 weeks post-treatment. (b) Note persistence of hyperpigmentation at 6 weeks after treatment, believed to be related to excessively long pulse width and high density. Hyperpigmentation after treatment with a nonablative 1,500-nm fractional erbium-doped laser has been reported9 in a small percentage of therapy. In the study of 961 successive treatments, 0.73% of treatments of both facial and nonfacial areas resulted in hyperpigmentation in dark-skinned patients and persisted for a mean of 50.57 days. Techniques to resolve this condition are similar to those of nonfractional lasers. For fractional laser resurfacing, eight studies (most with the 1,500-nm erbium-doped laser) have reported hyperpigmentation in 1 to 32% of patients, depending on the laser system, treatment parameters, and skin types.20 Procedure is similar to that of nonfractional laser-induced hyperpigmentation. Caused by excessive fibrosis and disruption of melanogenesis,30 hypopigmentation is noticeable skin lightening that may occur 6 to 12 months after CO2 laser resurfacing,22 after erythema and hyperpigmentation have resolved. Frequencies after resurfacing range from 1 to 20%.31 The risk of hypopigmentation is increased with depth of penetration into the reticular dermis28 and with the amount of thermal injury to the treated areas.22 It is most pronounced in the presence of melanosis or hyperpigmentation, as in Asian and Hispanic patients.28 Unlike hyperpigmentation, hypopigmentation may be irreversible and is treated by targeting surrounding depigmented areas with glycolic acid peels or light trichloroacetic acid peels to blend the pigmentary differences between the pale skin and untreated depigmented skin.22 Hypopigmentation may occur in areas treated aggressively or previously treated by phenol peeling or dermabrasion.27 Lines of demarcation may be minimized by treating the entire face rather than specific areas (▶ Fig. 19.5).13,31,32 Melanogenesis may be induced in hypopigmented areas by applying topical Oxsoralen with limited exposure to ultraviolet light to stimulate pigment recovery.22,31 Fig. 19.5 A 55-year-old man treated with fractional carbon dioxide (CO2) laser resulting in lines of demarcation and permanent hypopigmentation. Areas were re-treated with a superficial ablative CO2 laser with some improvement.
19.4 Patient Selection
19.5 Complications
19.5.1 Erythema


19.5.2 Hyperpigmentation

19.6 Hypopigmentation

Complications in Laser Resurfacing: Avoidance, Recognition, and Treatment
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








