CHAPTER 60 Complications and corrections of lipoplasty
Introduction
Lipoplasty or liposuction is a surgical procedure used to treat and reshape the body. It is an elective procedure that is typically performed on healthy patients who wish to improve their contour. Liposuction is becoming the most common procedure performed by plastic surgeons in the entire world, and is a very safe procedure today. However, it carries with it certain risks and complications, including a death rate of 1/5000 procedures.1 Risks can be minimized or avoided by a well-trained surgeon and surgical team.
History
Dujarrier first attempted to remove subcutaneous fat with a uterine curette, but tragic complications eventually evolved to necrosis and amputation, possibly due to vascular injury or infection.2 It was the first complication described for a lipoplasty attempt.
No technical innovations were achieved until 1982, when Joseph Schrudde used a delicate curette to correct lipodystrophy, significantly reducing blood loss.3
The senior author was one of the pioneers of the careful approach of the superficial layer of the abdomen which was, before this, responsible for many contour irregularities, as a consequence of treatment of the deeper layer. The same author included the back region and, progressively, included other areas, noting significant retraction of the skin and a better contour. He also observed that, with no superficial approach, it was difficult to obtain good results in the presence of scars or depressions.4 It was Gasparotti5 who named this technique “superficial liposuction” and promoted it internationally. The development of new techniques, new cannulas, better anesthesia and the better training of the surgeon are helping to ensure patients’ safety and the efficacy of the procedure.
Complications
Table 60.1 Factors that increase risk in lipoplasty
| 1. Injecting too much fluid and local anesthesia |
| 2. Removing too much fat |
| 3. Performing too many procedures in the same surgical act |
| 4. Wrong indication for the procedure |
| 5. Inadequate monitoring |
*Grazer FM, de Jong RH. Fatal Outcomes from liposuction: census survey of cosmetic surgeons. Plast Reconstr Surg 2000;105:436–446.
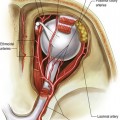
Deep vein thrombosis and pulmonary embolism
Therefore, a mandatory preoperative evaluation to identify factors of risk for thrombosis, as well as the use of elastic stockings, pneumatic systems of intermittent compression, adequate hydration and early mobilization are usually sufficient to prevent venous thrombosis in healthy patients undergoing lipoplasty.
Lidocaine and adrenaline toxicity
The FDA defines 7 mg/kg as the maximum safe dose of lidocaine with epinephrine (and 5 mg/kg for lidocaine only) for regional anesthesia. Literature on liposuction reports the use of lidocaine in doses of up to 33–35 mg/kg,1 but always in solutions with adrenaline and with low concentration of lidocaine (0.1%) in large volume infiltration. Since the subcutaneous area is able to retain lidocaine, it is be restricted to the infiltration site, and only the exceeding molecules (1 mg of lidocaine for 1 g of tissue) would be available to be submitted to conventional pharmacokinetics. Hepatic function is an important factor that interferes in the concentration of lidocaine. Even drugs which interact with lidocaine in the hepatic cytochromes, such as antidepressants, might raise the serum concentration of lidocaine, causing signs of toxicity in the central nervous and cardiac systems. The hepatic metabolization of lidocaine and adrenaline reaches its serum peak within three hours after infiltration, returning to normal values after 12 hours.6
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree