Introduction
HS represents a prime candidate to bridge diseases of the integument and comorbid systemic disease, as a chronic inflammatory disease of the pilosebaceous unit characterized by inflammatory nodules, suppuration and abscess formation resulting in pain and disfigurement. In addition to its locally destructive course, HS has gained recognition for its association with individual comorbid diseases as well as all-cause mortality. Indeed, patients with HS have been observed to have a higher global comorbidity burden than both healthy patients and patients with psoriasis. Systemic disease states with Charlson Comorbidity Indices similar to HS include systemic lupus erythematosus, dermatomyositis, and ankylosing spondylitis.
The chronic inflammatory state in HS may represent shared pathways yet to be characterized, which link HS to comorbid conditions. At present, biomarker expression in tissue and serum of HS patients appears complex and its description likely remains incomplete. Cytokine expression profiles in lesional skin have demonstrated increased levels of tumor necrosis factor (TNF), interleukin (IL)-1β, IL-6, IL-8, IL-10, IL-12, IL-17, and IL-23. The serum of HS patients has also shown elevated levels of C-reactive protein, TNF, IL-17, and IL-6.
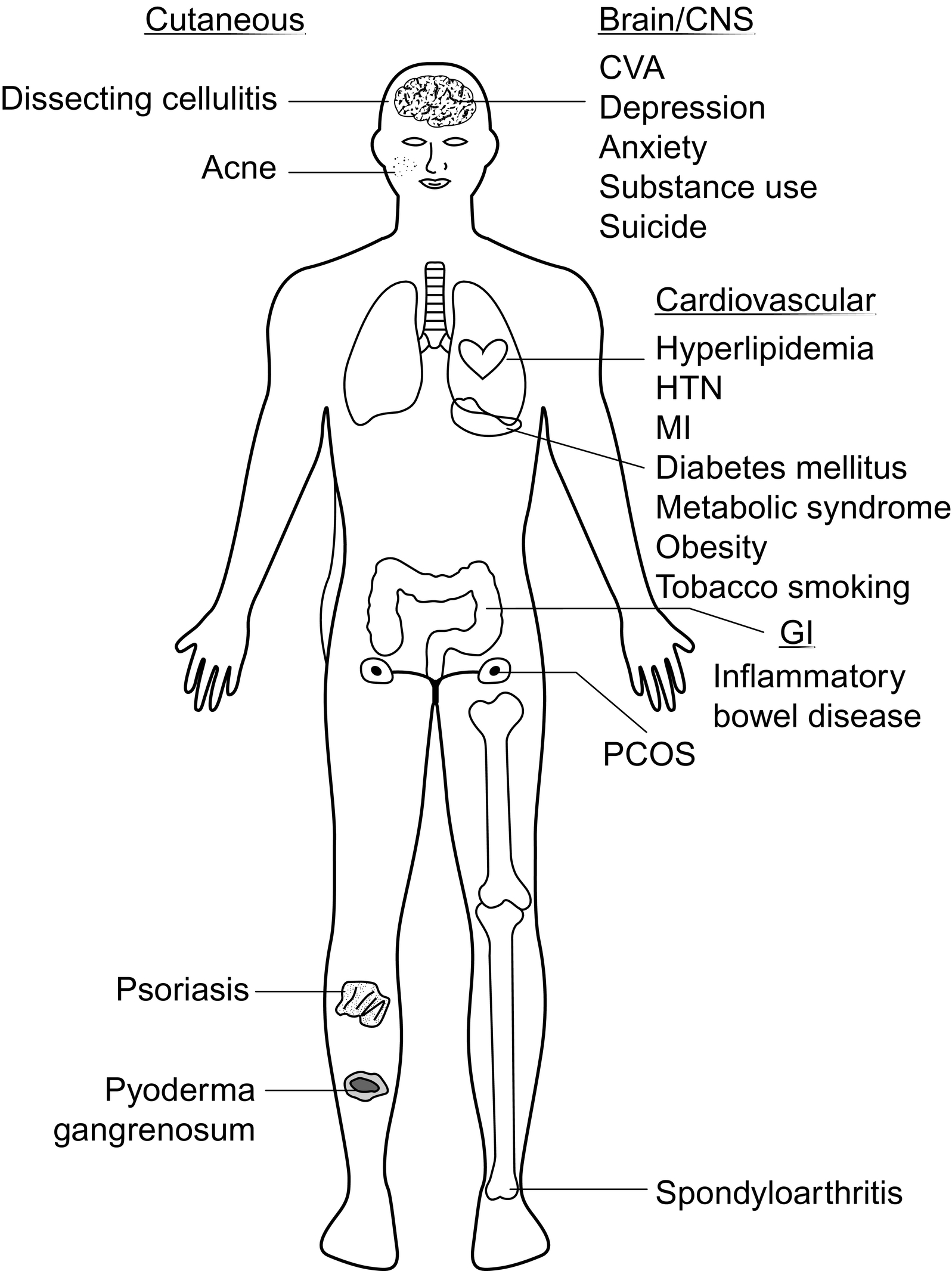
Comorbid conditions observed to be associated with HS range across almost every organ system, from the skin to the gastrointestinal tract to the cardiovascular system ( Fig. 8.1 ). HS symptoms may be the first to prompt patients to seek healthcare, providing an opportunity for comorbidity screening and the interdisciplinary management of HS patients with the goal of supporting overall health and clinical outcomes. Therefore, awareness of comorbid associations by physicians treating HS patients is highly relevant. This chapter includes an evidence-based summary of comorbid associations in HS. It is important to note that comorbidities in HS is a dynamic content area for which further evidence-based updates in the coming years may be necessary.
Associated Inflammatory Skin Diseases
Pyoderma Gangrenosum
Pyoderma gangrenosum (PG) is a neutrophilic dermatosis characterized by painful ulcerations with undermined and violaceous borders. This rare disorder can greatly impact quality of life and can cause significant morbidity in afflicted patients. Both HS and PG exhibit intense neutrophilic predominant inflammation and have overlap in treatment modalities, including anti-TNF agents. The cytokines IL-8 and IL-17, which are involved in promoting tissue neutrophilia, are overexpressed in both disorders.
The prevalence of PG among patients with HS has ranged from 0.2% to 0.4% as compared to only 0.01% in patients without a diagnosis of HS. This represents prevalence of PG 18 times higher in HS patients. In addition, patients who have concomitant HS and Crohn’s disease (CD) are more than 21 times as likely to have PG as compared to HS patients without comorbid CD. The development of PG in HS patients typically occurs 2 to 19 years after HS diagnosis. This may implicate ongoing immune dysregulation in HS patients which ultimately contributes to the development of PG. This is an area needing further investigation.
Psoriasis
Psoriasis is another chronic inflammatory disease of the skin with similar inflammatory mediators as HS, including TNF, IL-12, IL-23, IL-17. Both diseases have also shown response to a similar profile of targeted therapies, including TNF-alpha, IL-17, and IL-12/23 inhibitors. While the two disease phenotypes are vastly different, the overlap in inflammatory pathways may be due to a link between HS and psoriasis.
Evidence for the association between HS and psoriasis has been somewhat inconsistent in the literature. In a cross-sectional study with 68,836 psoriasis patients, the prevalence of HS was found to be significantly increased in the psoriasis group (0.3%) as compared to controls (0.2%). A statistically significant association between HS and psoriasis was found in a multivariate analysis adjusting for smoking, obesity, healthcare utilization, and Charlson Comorbidity index.
However, another large population-based study found no statistically significant difference in psoriasis prevalence. The prevalence of psoriasis among HS patients was 1.0%, whereas that among controls was 0.9%. Additional studies are needed to confirm this association.
Associated Disorders of Follicular Occlusion
Acne Vulgaris and Acne Conglobata
Both acne vulgaris and HS are chronic inflammatory disorders involving the pilosebaceous unit. Acne conglobata refers to a more severe inflammatory variant which results in tender inflammatory nodules, and in some cases double comedones and sinus tract formation, which is also appreciated in HS. For this reason, HS is often also referred to as acne inversa. The prevalence of acne vulgaris/conglobata in patients with HS ranges from 4.5% to 15.2%, which is significantly higher than the prevalence noted in patients without HS (0.9% to 6.2%). The odds of a patient with HS developing acne vulgaris/conglabata is up to 5 times higher than an individual without HS. While acne vulgaris and acne conglobata can often be treated with isotretinoin, there is limited therapeutic benefit of this medication as a monotherapy in HS. A modified treatment approach should therefore be used in patients with both diseases.
Pilonidal Disease
Pilonidal disease is a chronic inflammatory disorder of the pilosebaceous unit resulting in abscesses, cysts, and/or sinus formation in the sacral region. There is considerable overlap in the clinical manifestations of this disorder with HS, perhaps pointing to common inflammatory pathways which likely contribute to their association with one another.
The prevalence of pilonidal disease in HS patients ranges from 1.4% to 2.3%, compared to 0.1% to 0.3% in non-HS patients. HS patients have 5 times the odds of developing pilonidal disease compared to non-HS patients. There is some evidence to suggest that HS patients with more severe disease are more likely to have pilonidal disease compared to HS patients with milder disease.
Dissecting Cellulitis of the Scalp
Dissecting cellulitis of the scalp (DCS) is a chronic inflammatory disorder of the pilosebaceous unit and is part of the follicular occlusion tetrad along with HS, acne conglobata, and pilonidal disease. DCS is characterized by pustules, abscesses, inflammatory nodules, and significant tunnel formation on the scalp that ultimately results in scarring of affected areas. Overlap among these four entities in the follicular occlusion tetrad may be the result of a common pathogenesis, for which the exact trigger remains to be elucidated. Hyperplasia and overactivity of the pilosebaceous unit is noted first, then followed by follicular occlusion, development of double-ended comedones, and bacterial colonization. Subsequent rupture of occluded follicles results in an inflammation response with suppuration and eventual tunneling with scarring. This shared underlying proposed mechanism may be the basis for the association between HS and DCS. Some consider DCS to be a manifestation of HS involving the scalp.
The prevalence of DCS in patients with HS is 9.2%, compared to that of 0.7% in non-HS patients representing a 13-fold higher prevalence in HS patients.
Associated Cardiovascular Disorders
Major Adverse Cardiovascular Events
Major adverse cardiovascular events (MACE) are the sum composite of myocardial infarction (MI), cerebrovascular accident (CVA), and cardiovascular mortality. This definition may vary to include heart failure, percutaneous coronary intervention, coronary artery bypass grafting, and all-cause mortality. Both psoriasis and HS are inflammatory skin disorders that have been linked to a higher risk of MACE. The association between HS and MACE is thought to be the result of an increased systemic inflammatory burden consisting of elevated circulating TNF and IL-6 that contribute to thrombosis, endothelial injury, and atherosclerosis. HS patients have been observed to have a 23% increased risk of incident MI and a similar increase in risk for the development of CVA when compared to non-HS patients. This is an adjusted risk that accounts for covariates related to MI and CVA; examples include obesity, hypertension, diabetes mellitus, and tobacco smoking. The risk of cardiovascular-related death is higher in HS patients compared to that in severe psoriasis patients, which may point to a higher systemic inflammatory burden in HS patients, more severe involvement with disease covariates, or less robust control of these covariates.
Hypertension
The importance of hypertension as a comorbidity lies in the damage it causes to the cardiovascular system with consequent impact on the heart, kidneys, and brain. In one study, the prevalence of hypertension among HS patients was 34%, compared to only 3% in non-HS patients. After adjustments for age, sex, and smoking status, patients with HS were found to be twice as likely to have hypertension. However, not all studies have confirmed this association. Most adult patients have their vitals screened at the start of the primary medical visit, and as such it is important to ensure HS patients are linked to a primary care provider for this type of screening, as well as many others.
Tobacco Smoking
Nicotine has been shown to induce infundibular epithelial hyperplasia and hyperkeratosis, alter the cutaneous microbiome, stimulate release of TNF by keratinocytes and Th17 cells, disturb polymorphic neutrophil granulocyte chemotaxis, and immunomodulate macrophage function.
One study described “relaxation” and the “alleviation of negative feelings” as major motivators to smoke. The high prevalence of anxiety and depression in this HS patient population may also contribute to tobacco use.
The prevalence of tobacco smoking in HS patients has been observed to be as high as 80%. HS patients have four times greater odds of being active tobacco smokers and six times greater odds of having ever smoked. In one study of 4 million tobacco smokers in the United States, a temporal relationship between smoking and the development of HS was established, suggesting that tobacco smoking could be a risk factor for HS. While evidence supporting smoking cessation as a means to improve disease course is limited, reducing or eliminating tobacco exposures has proved beneficial for overall health.
Associated Metabolic Disorders
Metabolic Syndrome
Metabolic syndrome is an aggregation of multiple factors that contribute to an elevated risk of cardiovascular disease. There are multiple definitions for metabolic syndrome, with the primary components being truncal obesity, hypertension, dyslipidemia, and insulin resistance. HS, like other chronic inflammatory diseases, has been linked to an increased prevalence of metabolic syndrome. The biological link between HS and metabolic syndrome may be explained by the downstream systemic effects of adipose tissue secretion of pro-inflammatory mediators in obesity, along with insulin resistance in the setting of chronic inflammation.
In five studies, the prevalence of metabolic syndrome among HS patients ranges from 10.4% to 50.6%, compared to 7.1% to 30.2% among controls. Pooled adjusted odds of metabolic syndrome among HS patients range from 1.8 to 2.2 times that of controls.
Obesity
Obesity is defined as a body-mass index greater than 30 kg/m 2 and it is a significant risk factor in the development of comorbidities such as hypertension, type II diabetes, and coronary artery disease. While HS can affect people regardless of their BMI, it is predominantly seen in those who are overweight or obese. The connection between obesity and HS may be related to a higher systemic inflammatory burden from adipose tissue and/or from local factors such increased friction in intertriginous areas.
The prevalence of obesity among HS cohorts may be as high as 88%. In a meta-analysis of 8 studies, HS patients were observed to have a 3.5-fold higher odds of being obese compared to patients without HS.
The relationship between obesity and HS should not further stigmatize patients who are afflicted with HS. Given the negative impact of the condition on physical functioning, the authors acknowledge that HS may contribute to weight gain. There are also other risk factors likely to contribute to the development of HS. Indeed, there are numerous non-obese patients who also develop disease. Accordingly, it is essential that clinicians do not ascribe development of HS to obesity alone. We suggest approaching the topic of obesity in HS with the utmost sensitivity, only after establishing a patient-doctor relationship based on principles of empathy, trust, and overall health advocacy.
Type II Diabetes Mellitus
Type II diabetes mellitus results from insulin resistance over time and is linked to being overweight or obese. The association between diabetes and HS is thought to be multifactorial. A contributing factor may be TNF dysregulation, which leads to systemic insulin resistance by means of inhibiting the insulin receptor tyrosine kinase in muscle and fat, thereby preventing glucose uptake by these cells.
The prevalence of diabetes mellitus among HS patients ranges from 7% to 24%. Pooled odds ratios from several studies revealed that HS patients had 1.7 to 2.8 times the odds of having diabetes compared to patients without HS. This risk is independent of covariates, including obesity, which potentially implicates shared underlying pathways between HS and diabetes.
Hyperlipidemia
Hyperlipidemia (HLD) is an umbrella term that encompasses a wide range of disorders resulting in elevated lipid levels in the blood and a doubled risk for cardiovascular disease. It is one of the components of the metabolic syndrome and has been consistently observed to be associated with HS.
The prevalence of dyslipidemia among HS patients ranges from 3.3% to 45.3%, as compared with 1.6 to 18.7% among controls. In a meta-analysis of nine studies comprising 6174 HS patients, odds of hypertriglyceridemia and low HDL among HS patients were 1.7 (95% CI 1.1–2.5, P = .009) and 2.5 (95% CI 1.5–4.2, P < .001) times that of controls, respectively.
Associated Endocrine Diseases
Polycystic Ovarian Syndrome
Polycystic ovarian syndrome (PCOS) is characterized by hyperandrogenism, ovulatory dysfunction, and polycystic ovaries seen on ultrasound. Both PCOS and HS have in common a similar demographic composition, link to obesity and metabolic syndrome, and response to anti-androgen therapy. However, increased androgen levels have not been reliably appreciated in HS.
The prevalence of PCOS among women with HS is as high as 9.0%. Across studies, women with HS had 1.2 to 13.4 times the odds of having PCOS compared to controls.
Associated Gastrointestinal Diseases
Inflammatory Bowel Disease
Similar to HS, inflammatory bowel disease (IBD), including ulcerative colitis (UC) and CD, is characterized by chronic, recurrent inflammation involving epithelia, which is inhabited by commensal flora. HS and CD are further characterized by suppuration and granulomatous inflammation, which may eventuate in fistula and sinus tract formation. Dysbiosis has been implicated as a cause of IBD as well as a cause of HS, which may also help to explain the link between IBD and HS. These diseases may also share overlapping cytokine signatures, including IL-23/Th-17 and TNF, with response to corresponding targeted therapies.
There are a number of population-based studies that have evaluated the association between HS and IBD. In the largest study, the prevalence of CD among over 50,000 HS patients was 2%, compared to 0.6% among non-HS patients. Adjusted odds of having CD among HS patients were three times that of controls. In three other studies, prevalence of CD among HS patients ranged from 0.2% to 0.8%. Among HS patients, the adjusted odds of having CD was 1.2 to 2.0 times that of controls. The prevalence of UC among HS patients ranges from 0.3% to 1.3%. In adjusted analyses from three population-based studies, HS patients had 1.3 to 1.8 times the odds of UC compared to controls.
Associated Musculoskeletal Diseases
Spondyloarthritis and HS appear to share key inflammatory mediators including TNF, IL-1, and IL-17, suggesting there may be a biological link between these two conditions.
In a recent large cohort study, patients with HS had an increased risk for developing ankylosing spondylitis (incidence rate, 0.60 vs. 0.36 per 1000; HR, 1.65 [95% CI, 1.15–2.35]), psoriatic arthritis (incidence rate, 0.84 vs. 0.58 per 1000; HR, 1.44 [95% CI, 1.08–1.93]), and rheumatoid arthritis (incidence rate, 4.54 vs. 3.86 per 1000; HR, 1.16 [95% CI, 1.03–1.31]) compared to controls.
In other studies, the prevalence of spondyloarthritis among HS patients ranged from 0.3% to 28% as compared with 0.2% to 2.6% among controls. The adjusted odds of spondyloarthritis among HS patients ranged from 1.5 to 9.4 times that of controls.
Associated Psychiatric Diseases
Depression
Major depressive disorders are the number one cause of disability in the United States and worldwide, and it has significant impact on employment, school, and interpersonal relationships. The connection between depression and HS may be linked to the significant disease-specific impact of HS on quality of life. However, there is also evidence to support a potential link via an increased immune system activation, as has been observed in cytokine – induced sickness behavior in which a high level of pro-inflammatory cytokines results in depression and loss of energy.
The prevalence of depression among HS patients was calculated to be 21% from pooled data in a 2019 meta-analysis of 28 studies and analysis of case-control studies. HS patients had twice the likelihood of having depression compared to controls. The prevalence of depression may be greater among patients with higher Hurley stages.
Generalized Anxiety Disorder
Fear and unpredictability of pain, odor and discharge, as well as concern about the ability to participate in daily activities can lead to excessive worry among HS patients that may result in chronic functional impairment.
In a 2018 meta-analysis of 10 studies, the prevalence of Generalized Anxiety Disorder (GAD) among HS patients was approximately 5%. Several retrospective clinical and administrative database studies have also described a higher prevalence and likelihood of anxiety among HS patients compared to controls.
Substance Use Disorder
HS patients experience chronic pain and have significant physical, emotional and psychological disease impact which may increase risk for substance use disorder (SUD).
In a cross-sectional study of over 32,000 HS patients, the prevalence of SUD was 4.0%, which was significantly higher compared to 2.0% in controls. The most common forms of SUD were alcohol (48% of SUD cases) opioids (33% of SUD cases). HS patients had a 50% greater increase in risk of SUD compared to controls. In a separate retrospective cohort study involving over 20,000 HS patients, the 1-year incidence of chronic opioid use (COU) among opioid-naïve HS patients was 0.3%, double that of controls. In adjusted analysis, HS patients had a 50% greater risk of developing COU compared to the general population. Given the significant impact of HS and the related risks of substance use, heightened awareness of potential abuses should be maintained with use of screening tools and referral as appropriate.
Completed Suicide
Data from European national registries indicate a higher incidence of completed suicide among HS patients. In Finland, the incidence of suicide was 4.4% among HS patients, with odds of suicide almost three times higher than in the general population. In Denmark, HS patients were observed to have a suicide incidence of 0.3 per 1000 person-years, which translated to an adjusted risk of 2.4 times that of the general population.
Associated Genetic Diseases
Down Syndrome
Expression of amyloid precursor protein (APP) is increased in Down syndrome (DS). In the epidermis, APP plays a role in stimulating keratinocyte adhesion, migration, and proliferation. In this way, DS patients may be prone to keratinocyte hyperproliferation and follicular plugging.
In a cross-sectional study of nearly 12,000 DS patients, the prevalence of HS was 2.1%, compared to 0.3% in controls. Patients with DS had five times the risk of HS (adjusted odds ratio 5.24 [95% CI 4.62–5.94]) compared to patients without DS. Over 80% of DS patients had their HS diagnosed by age 29 years. In a retrospective single-center study, the prevalence of HS among DS patients was 24%, compared to 0.5% among controls.
Associated Inflammatory Syndromes
HS may be a component of rare genetic inflammatory syndromes, including pyoderma gangrenosum, acne and hidradenitis suppurativa (PASH) syndrome; pyoderma gangrenosum, acne vulgaris, hidradenitis suppurativa and ankylosing spondylitis (PASS) syndrome; pyogenic arthritis, PG, acne vulgaris, and hidradenitis suppurativa (PAPASH) syndrome; and psoriatic arthritis, pyoderma gangrenosum, acne, and hidradenitis suppurativa (PsAPASH) syndrome. These disorders arise from a disruption of the inflammasome and result in over-expression of IL-1 and TNF and a neutrophil predominant inflammation. A mutation in the PSTPIP1 gene is observed in PASH and PAPASH. For the other syndromes in this group, including PASS and PsAPASH, a specific mutation has not yet been identified. These HS-related syndromes underscore the importance of evaluating the constellation of symptoms and comorbid conditions which afflict HS patients.
Emerging Comorbidities
There have also been a number of additional observations of comorbid conditions in HS; examples include anemia, non-alcoholic fatty liver disease, obstructive sleep apnea, thyroid disease, and lymphomas. However, at present, the quantity and/or quality of data does not support routine screening of HS patients for these disorders unless suggestive signs or symptoms in an individual patient are present to warrant further investigation.
Conclusion
There are a number of comorbid conditions that can afflict patients with HS and contribute to poor health and impaired quality of life, beyond the significant impact of the disease itself. The discussion in this chapter is intended to support health advocacy efforts along with comprehensive care strategies for HS patients. Based on evidence, the authors suggest interdisciplinary screening for comorbidities discussed herein. Dermatologists may examine the skin for cutaneous associations and consider streamlined approaches for management of HS and any associated skin conditions. Dermatologists may also perform a simple review of systems or screening laboratory tests for other comorbidities. However, given the large comorbidity burden among HS patients, dermatologists may best advocate for optimizing overall health by ensuring HS patients are linked to primary care. Primary care doctors should be prompted to screen for comorbid conditions that do not already fall within standards of care based on age and other risk factors.
While there have been significant advances in our understanding of HS comorbidities in recent years, several knowledge gaps still exist; examples include risk of squamous cell carcinoma and the influence of HS on pregnancy course and outcomes. There is also a need to identify which comorbid conditions afflict children and adolescents with HS. Additionally, little is known about disparate disease and comorbid outcomes across demographic groups. Study of health disparities is particularly important in HS, which disproportionately affects women and Black patients in the United States. With identification of novel immune targets and the development of advanced therapeutic agents that effectively address inflammation in HS, there will be opportunity to also understand whether treatment of HS allows for better control of comorbid conditions or reduces risk of developing comorbid disease.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








