Chapter 9 Combined abdominal contouring and mastopexy
• This is the most common combination in body contouring surgery.
• The population is comprised of females between their 30s and 50s.
• Several technical improvements have been described in the last 50 years.
• Liposuction techniques have laid the foundation for lipoabdominoplasty.
• There is a good safety profile for the combination of these procedures
Introduction
The combination of abdominoplasty and mastoplasty is very common, especially for patients post pregnancy or post weight loss with abdominal laxness, striae, muscle rectus diastases, and breast ptosis. It is most commonly performed in women in the age range 30–50. Many traditional abdominoplasty and mammaplasty techniques have been published in the last 50 years with extraordinary results, but with the introduction of liposuction, described by Illouz1 in 1980, we had a new tool for body contouring surgery. This opened up a new treatment method for lipodystrophies in the epigastric, flank, dorsum, trochanteric, and buttock areas. The procedure combining abdominoplasty and liposuction was called “lipoabdominoplasty,” and since then many new techniques and modifications have been proposed.
Since abdominoplasty was first described by Callia2 and Pitanguy,3 many refinements have been published in the literature.4–14 In 1975, Sinder15 described the superior epigastric incision approach to estimate a safe inferior abdominal flap excision. Planas16 published a similar procedure in 1978 and Serson Neto17 and Pontes18 described the geometrical inferior flap block resection. Mammaplasty, when combined with abdominoplasty, can take the form of breast augmentation, mastopexy, or breast reduction. For breast augmentation we prefer to use silicone texturized prostheses. For breast reduction we prefer the Silveira Neto dermoglandular rotation flap, published in 197619 and subsequently improved by Uebel in 1978.20 For mastopexy we use the Pitanguy21 or Ariê22 techniques with a superior pedicle flap. There are many other techniques in the literature but these are the most used by us in body contouring surgery – very simple procedures that maintain physiological function and good esthetic results. Stemming from those techniques, we have introduced some important approaches and details to ensure consistency. This will be discussed further in this chapter.
Abdominoplasty
Preoperative Preparation
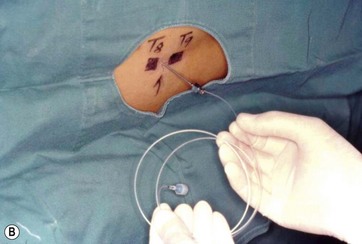
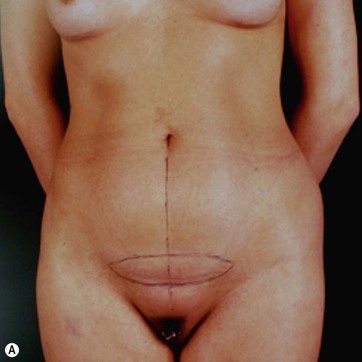
In a standing position we take pictures with a digital camera (10 megapixels) and we mark the incisions of the abdomen wall and breasts, as well as all the areas to be treated with liposuction. We estimate the amount of skin and breast tissue to be removed, and in the sitting position we estimate the amount of skin and fat to be removed from the abdominal wall (Fig. 9.1A–E).
With the patient in a sitting position, we estimate the amount of skin resection needed.23 We identify the lateral inguinal folds (Fig. 9.2A, B) and a low abdominal curved line is delineated approximately 8 cm from the labia major vertex.
FIG 9.2B APPEARS ![]() ONLINE ONLY
ONLINE ONLY
With the patient in a standing position, a line drawn from the superior umbilical region is connected to both extremities and the areas to undergo liposuction are outlined (Fig. 9.3).
Anesthesia
High epidural anesthesia via catheter is almost always used, with insertion in the thoracic 11–12 spinal level and connected to a continuous infusion pump. A 15 ml solution of 7.5 mg/ml ropivacaine HCl (Naropin) and 30 mg sufentanil citrate is infused into the epidural space and an analgesic solution is prepared for postoperative administration via the infusion pump (100 mg sufentanil citrate and saline solution 0.9%, 100 ml at a speed of 5 ml per hour.24 Elastic bandages are applied to the legs to prevent thrombovenous embolism (Fig. 9.4A–D).
FIG 9.4A–D APPEARS ![]() ONLINE ONLY
ONLINE ONLY
Surgical Technique
Tumescent Infiltration and Assisted Liposuction
All areas to be lipoaspirated and undermined are infiltrated with a saline solution containing epinephrine at 1 : 500 000 concentration to avoid excessive bleeding (Fig. 9.5A, B).


FIG. 9.5 All areas to be treated are infiltrated with a saline solution with epinephrine 1 : 500 000.
FIG 9.5 APPEARS ![]() ONLINE ONLY
ONLINE ONLY
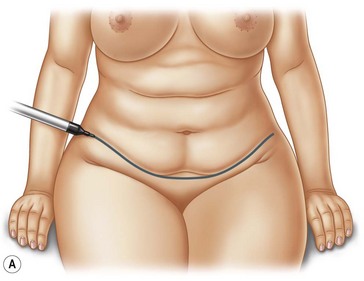
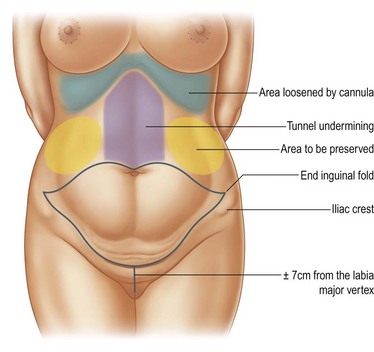
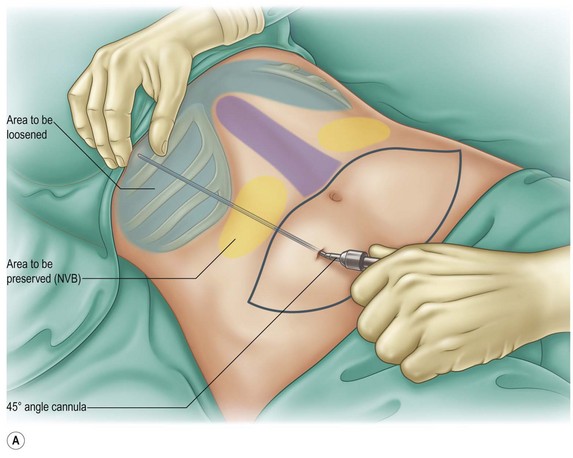
The patient is positioned prone and the flank and trochanteric areas are manually lipoaspirated with a 3 mm cannula. The patient is then rotated to the supine position and extensive liposuction is performed on the entire abdomen and epigastric areas. It is important to reach the inframammary region and the xiphoid appendix, extending to the chondrocostal border to fully loosen this area, as described by Avelar25 and Saldanha.26 For this maneuver we use an angular cannula, described by Reggazzo (personal communication), to prevent internal perforations. The only region to be avoided is the lateral superior flank, in order to avoid damaging the neurovascular bundles that give arterial, venous, and neural support to the flap (Fig. 9.6A, B) (Fig. 9.7A, B, C).
FIG 9.6, 9.7C APPEARS ![]() ONLINE ONLY
ONLINE ONLY
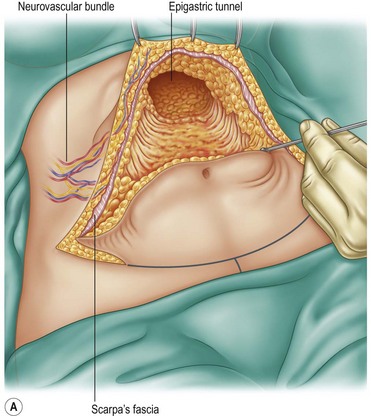
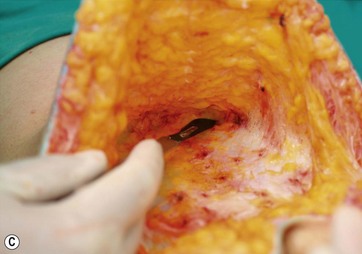
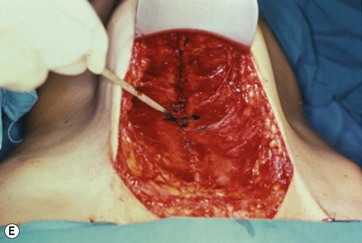
Supraumbilical Incision and Epigastric Tunnel Undermining
A supraumbilical incision is first done and an epigastric tunnel is undermined to the xiphoid appendix. It is important to preserve the lateral superior flank area and to avoid damage to the neurovascular bundles that support the entire flap (Fig. 9.8A, B, C).
FIG 9.8B, C APPEARS ![]() ONLINE ONLY
ONLINE ONLY
We have already described this27,28 and proposed the mini-abdominoplasty technique (Fig. 9.9A–F and Fig. 9.10A–H), stressing the importance of preserving the lateral columns when undermining the long xiphopubic tunnel and total umbilical stalk section.
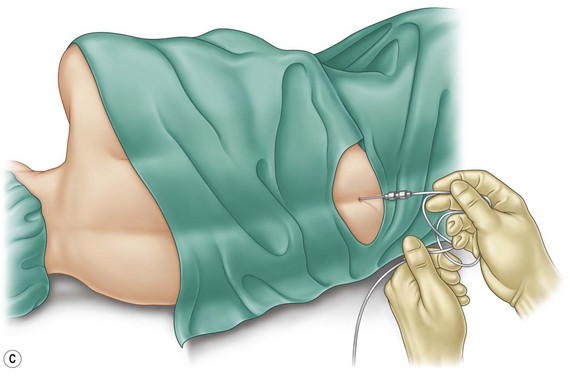
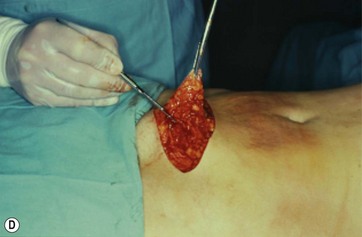
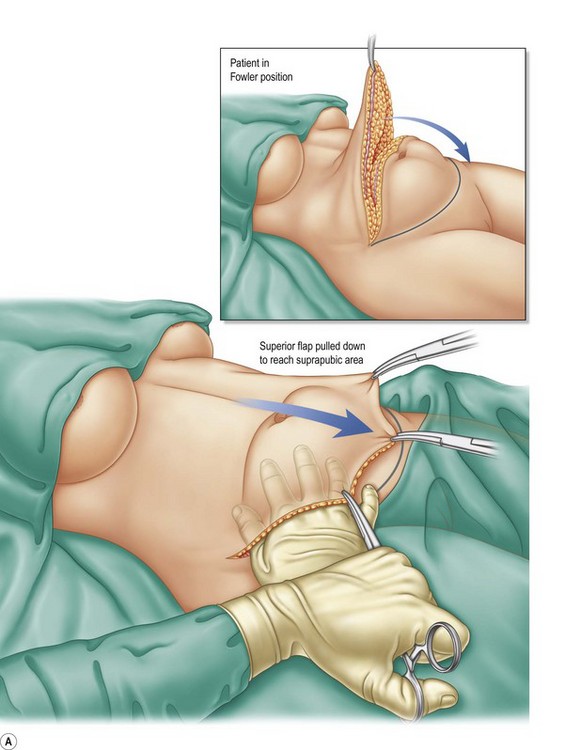
Pull-down Approach
The patient is placed in a Fowler position and the flap is pulled down to reach the inferior suprapubic line delineated previously, and to estimate whether the inferior flap resection can be done en bloc without problems (Fig. 9.11A–C). This maneuver is critical to determine whether the defect can be closed without stretching. The inferior suprapubic line can then be moved up or down, depending on the laxness and elasticity of the skin and patient biotype. Normally it is approximately 7–8 cm from the labia major vertex.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree