Overview of Patient Population with HS Prior to Initiating Therapy
Hidradenitis suppurativa is a clinical diagnosis based on history, physical exams, patterns of recurrence, types of lesions, and scarring. No diagnostic test is currently available and biopsy results are relatively non-specific compared to clinical patterns. Once the diagnosis has been made, an assessment of severity and comorbidities should follow, as they will affect treatment choices.
Obtaining History Related to HS Onset and Family History
Onset of Hidradenitis Suppurativa Symptoms
Patients may develop signs and symptoms of hidradenitis suppurativa (HS) throughout most of the life span, with most reports ranging from 15 to 60 years old. Women, who make up 70% of the HS population, tend to present in their 20s and 30s, reporting symptoms that started years earlier. There may also be smaller peak that occurs in the post-menopausal population. HS is more common in African Americans and Caucasians and may occur less frequently in Asian populations. Since the majority of HS epidemiology studies are from North America and Europe, the current HS racial demographics may not be fully representative of the actual prevalence of HS.
There is, on average, a 7-year gap between symptoms and receiving a diagnosis. The delay in diagnosis may be due to multiple factors ranging from reluctance to disclose their symptoms/signs to misdiagnosis, such as folliculitis. Additionally, patients can have gradual development of HS symptoms prior to deciding to seek care.
Initial HS symptoms include the development of multiple recurrent papules or nodules in one or more locations. Inflammatory nodules may evolve into abscesses, fistulas, and/or sinus tracts. Pocketed scarring and sinus tracts are classic features and very helpful in distinguishing this disease from folliculitis, which also tends to present with smaller, more superficial lesions. Some patients may not present with these classic features early in their HS disease or if they have only mild disease, which can lead to delay in diagnosis if a thorough patient history is not obtained. While obtaining history, clinicians should ask patients to describe their lesions and whether they have noted changes over months to years. It is often helpful to provide examples to the patient of what HS lesions look like and the locations where they tend to appear. Patients often have historical pictures they can provide as well.
A thorough history of timeline of events prior to and after HS symptom onset can also be contributory. Changes to patient’s diet, medications, weight gain, stress, tobacco use, menses onset, pregnancy, and menopause onset as relevant may aid in determining triggers. For example, in women, flares due to hormonal fluctuation are common.
Family History of Hidradenitis Suppurativa Symptoms/Diagnosis
Hidradenitis suppurativa has autosomal dominant, albeit complicated, inheritance pattern with one-third of patients reporting a family member with HS-like symptoms. Furthermore, patients with early-onset HS disease are more likely to have a family history of HS compared to patients with normal-onset HS, which is defined at onset of puberty or later. Although some genes have been identified, they do not explain the majority of cases. If available, the family member’s affected HS lesion location(s), flare triggers, and treatment history may be useful: for a patient with extensive disease and a family history of chronic HS lesions with prominent scarring, early initiation of systemic therapy should be discussed.
The Physical Exam
Pertinent Locations
Hidradenitis suppurativa is predominant, but not exclusive to apocrine gland-bearing regions. Commonly affected areas include the axillae, inframammary area, lower abdomen, inguinal region, perineum, and gluteal region. Patients will describe having multiple papules that evolve into nodules, abscesses, and/or fistulas. Scarring is a prominent feature of moderate-to-severe HS, which may appear as pocketed, cribriform scars, and/or interconnected scars.
On initial exam, the physician should examine all locations where HS may appear to keep note of lesion progression, which is common. Patients may report not having any active lesions in an area, but still present with HS lesions, such as non-draining fistulas. This should be noted on exam to have a consistent Hurley staging and Physician’s Global Assessment. Both of these assessments are described in further detail later on in this chapter.
When examining the patient, the physician can assist the patient in positioning them to examine symmetrically affected areas, such as both axillae, at the same time to minimize pain and discomfort. This technique minimizes the amount of time a patient has to be in an uncomfortable position due to limited mobility from scarring. Additionally, patients should be given the choice to remove their wound dressing. If the patient prefers keeping the dressing on, then the clinician should make note of it and ask the patient to describe any active lesions they have at the site.
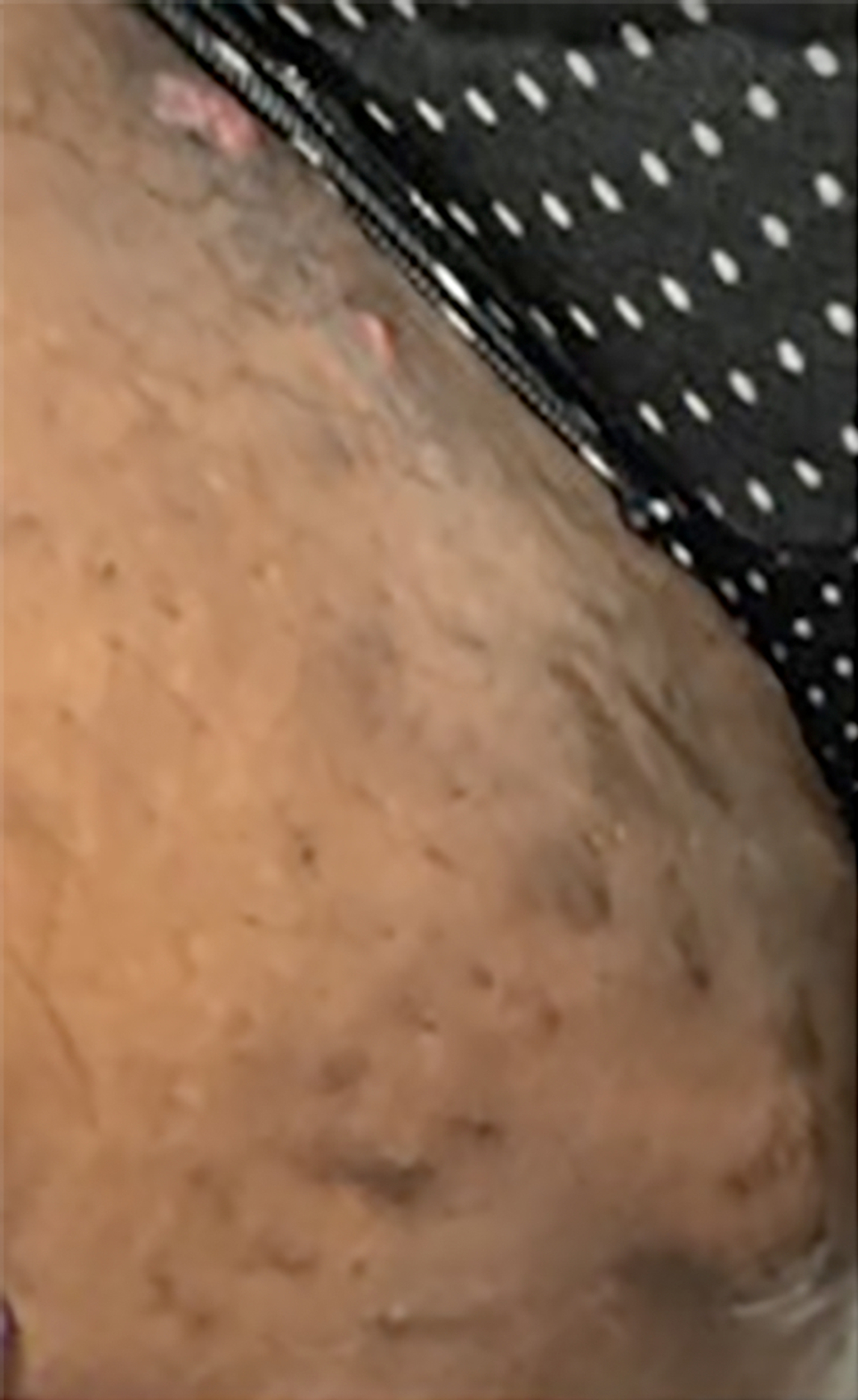
When the axillae and groin are affected, patients may describe having limited mobility due to pain and scarring. Fig. 7.1 demonstrates the classic tunneling scars with overlying fibrosis and post-inflammatory hyperpigmentation seen with hidradenitis suppurativa in the axilla. Another commonly affected area is the inframammary region. Fig. 7.2 demonstrates inframammary region affected with abscesses and papules with overlying erythema in a female patient (see Fig. 7.2 A) and male patient (see Fig. 7.2 B), respectively. The groin region is also affected in HS and female patients tend to present with isolated groin disease when they have limited disease extent. Fig. 7.3 shows a few inflammatory nodules with surrounding scarring tracts in a female patient.



Lesion Count
Lesion count assessment consists of assessing the number of nodules, abscesses, and/or fistulas present. Papules are not generally formally included in the assessment. Although papules may occur as a new early lesion, most HS lesions are large and deep (> 1 cm) such that a papule-predominant presentation may prompt evaluation for another condition such as folliculitis. When counting lesions, the clinician should determine whether the lesions are interconnected, which may be part of the same underlying process. When documenting lesions, the clinician should categorize the lesion for fully assessing disease severity. While there is currently no standardized HS lesional terminology, there are available validated terminologies that can be used.
When assessing the patient, the clinician should fully visualize all the affected areas, including regions where the patient may not have any active lesions. There may still be background disease that should be noted. The physical exam may be difficult for some patients due to lesion tenderness. Additionally, patients will often have wound dressings over their lesions that are removed for the physical exam. The clinician can allow the patient to remove their own dressings to avoid any unnecessary pain in the process. New wound dressings can be offered following the physical exam.
Lesion Description
Lesion characteristics are also used for determining disease severity. On exam, fistulas may drain spontaneously or on palpation. If a patient’s fistulas no longer drain on a subsequent exam, then the disease severity score may change. HS nodule assessment also will affect the disease severity score based on tenderness presence on palpation. Patients may report tenderness even without palpation; therefore, clinicians should minimize lesion palpation for the patient unless required for scoring in a clinical trial or other disease assessment. Scarring and post-inflammatory hyperpigmentation should also be assessed to monitor for signs of improvement overtime and with HS treatment.
Documenting Other Pertinent Features on Skin Exam
Other medical conditions that have higher prevalence in patients with HS compared to the general population include metabolic syndrome. On exam, patients may appear overweight and have skin findings, such as acanthosis nigricans, which supports metabolic dysregulation. In female patients, polycystic ovarian syndrome (PCOS) is another comorbidity seen in HS. Features on physical exam include darkened hairs on the face, peri-areolar area, and groin region.
Hidradenitis Suppurativa Disease Assessment
Detailed discussion of clinical assessment tools can be found in Chapter 13 , “Disease Evaluation and Outcome Measures.”
Hurley Staging
The Hurley staging system was developed initially for clinical staging prior to undergoing surgery. This staging system is now commonly used in the clinical and research setting for staging overall disease severity. Physicians use this to determine whether a patient may require systemic therapies for their disease. Different but overlapping treatment algorithms have been associated with each Stage in the literature, including follow-up visit planning and lab monitoring. Patients with more severe disease will require frequent clinic visits for monitoring, specifically in the first 4 to 6 months of starting a systemic therapy, such as adalimumab or infliximab, to monitor progress.
While disease activity may improve, the Hurley stage may remain unchanged due to the permanence of scarring and sinus tracts. If treatment has been optimized and the patient continues to have rare HS flares, then clinicians can start to focus on surgical options for scar and sinus tract management. The Hurley staging system is excellent for initial evaluation in helping determine the appropriate aggressiveness of the therapy, but should also be used with other dynamic assessments, such as the physician’s global assessment and Dermatology Life Quality Index (DLQI) which are discussed in the next sections.
Hidradenitis Suppurativa Physician’s Global Assessment
The hidradenitis suppurativa physician’s global assessment (HS-PGA) as initially used to evaluate the efficacy of adalimumab in patients with moderate-to-severe HS disease in a parallel randomized trial. This assessment consists of different stages with a score from 0 to 5. This includes clear (score: 0), minimal (score: 1), mild (score: 2), moderate (score: 3), severe (score: 4), and very severe (score: 5). This scoring system is calculated based on the lesion count and description. The clinician assesses the number of abscesses, draining fistulas, inflammatory nodules, and non-inflammatory nodules. Clinical improvement based on the HS PGA score is defined as improvement in the score by a minimum of 2 grade points to a score of clear, minimal, or mild. This scoring system is highly useful for adjusting a patient’s treatment based on their physical exam findings.
Dermatology Life Quality Index Assessment
The DLQI assesses the patient’s perspective of their disease. It is rapidly performed, designed for clinical use, and allows patients to further define treatment success for their chronic disease. The DLQI includes questions inquiring about symptoms and impact on personal relationships, leisure, daily activities, treatment, and occupation. Patients may have higher scores for questions related to pain, personal relationships, and occupation. Lesion pain with associated limited mobility leads to missing work, social events, and relationship commitments.
Pain Assessment
While pain is assessed in the DLQI assessment, clinicians can also monitor patient’s pain secondary to their HS at every visit. Patients will often have recurrent pain that worsens during HS flares. The numeric rating scale (NRS) for pain of 0 to 10, with 0 being no pain to 10 being the worst pain experienced, can be used to track treatment progress and determine if management should be adjusted. The visual analogue scale (VAS) for pain is another scale that uses defines two extreme endpoints of no pain to worse pain possible. The distance from no pain to where the patient marks their pain determined the pain severity level.
Other Important Considerations Regarding Therapeutic Choices
Hidradenitis Suppurativa Flare Triggers
There are multiple known triggers for HS flares. These include menses, androgen-containing oral contraceptives (OCPs), dairy intake, stress, heat, sweating, friction, and pregnancy.
Female predominance in HS has led to multiple theories and studies evaluating potential roles of hormones. In our experience, those who present with peri-menstrual flares often have their disease limited in location with the groin and thighs predominantly affected. These patients often respond well to anti-androgen therapy, such as spironolactone. The disease course improves after menopause for most women with this type of disease, but some may have persistent disease.
Another identified flare trigger in our population is androgen-containing OCPs that do not have opposing estrogen. OCPs can also be discussed with a patient’s obstetrician-gynecologist (OB/GYN) to determine which one is the best option for them. Hormonal modulation is discussed in the next section.
Pregnancy often leads to HS flares, a finding that also supports the role of hormones in this chronic disease. Patients will often report worsening of their HS during and particularly after pregnancy. While treatment options are limited during pregnancy, treatment can be switched to other similar therapies to avoid HS flares. Certolizumab is often used in place of adalimumab during pregnancy because it is not transported across the placenta. Clinicians will want to collaborate with patients’ OB/GYNs to discuss treatment options during pregnancy. HS considerations in women is further discussed in Chapter 31 , “Hidradenitis Suppurativa in Women.”
Diet continues to be a popular topic in HS patient support groups. Often, patients will present for initial evaluation and report changing their diet. Approaches include eliminating food they consider promoting inflammatory processes such as dairy, carbohydrates, or nightshades. Extrapolating from acne, it is possible that dairy (especially androgenic whey proteins found in skim milk and some protein powders and bars) can trigger HS flares and elimination seems reasonable to try. To date, there is insufficient evidence for other food categories. Weight loss appears to beneficial for the preponderance of patients, although large skin folds can foster continued problems.
Heat, sweating, and friction are well-described triggers for HS flares. Heat and sweating exacerbate the affected HS lesions due to their location, including the axillae, inflamed region, and groin region. Friction also can irritate the lesions and prevent them from healing due to constant movement of the affected areas. During evaluation, the clinician should discuss with the patient what types of dressings they have tried. Wound dressings are constantly being developed to manage frequent lesion drainage and prevent friction. Weight loss also may help decrease friction in the affected HS areas.
Another trigger commonly shared by patients at initial and follow-up visits is stress. They describe having treatment improvement but then developing HS flares due to a stressful event. Clinicians may wish to discuss with patient how frequently this occurs to be able to adjust the treatment regimen. A short course of antibiotic can be provided with refills as well. This will help shorten the duration of the patient’s HS flare.
Hormonal Modulation
Birth control choice can be very important in patients with HS. Some patients describe gradually developing HS lesions after starting a new birth control: high-androgen containing OCPs and androgen-only birth control, even in the intrauterine device (IUD) form, can trigger and worsen HS. Clinicians should inquire of any potential contraindications to a type of birth control, such as having migraines with auras or long-term smoking. Additionally, birth control compliance should be discussed with patients to determine which birth control would be the best option for the patient.
Low-androgen OCPs, such as ethinyl estradiol-drospirenone and ethinyl estradiol-desogestrel, can benefit females who have perimenstrual flares with limited disease. This type of OCP can be used with spironolactone or by itself to prevent flares in this patient group. Copper-containing IUDs do not contain hormones and can also be a birth control option for patients.
Following discussion with patients about birth control, clinicians may determine whether changing birth control is recommended and also whether the patient plans on becoming pregnant in the near future. Patients may have an IUD or birth control implant that they prefer to remove at a later point. If this is the case, the clinician can provide the patient with a list of optimal birth control options once the patient chooses to change birth control.
Obtaining Information of Other Medical Problems
A thorough medical history should be obtained prior to initiating systemic management. This includes inquiring about history of malignancy and, depending on the agents, central nervous system disorders and cardiac disease. Since some immunomodulating therapies used for HS can increase risk of infection, clinicians should also ask about history of hepatitis infection and any opportunistic infections, such as tuberculosis.
The risk of developing malignancy while on systemic therapy will vary by agent, but if a treatment with immunomodulating effect is being contemplated, clinicians should determine a patient’s baseline risk. Annual skin exams are generally recommended in these circumstances with special attention to the perianal area in men, where squamous cell carcinomas (SCCs) have been reported to develop.
Infection, including hepatitis B reactivation and tuberculosis, may occur while on biologic therapies. Clinicians should obtain information about any past treatment patients underwent if they have a history of these infections. Infectious disease may be consulted regarding infection management options prior to treatment initiation. Baseline labs for these infections are discussed in the last section of this chapter.
Another demographic that is common and associated with HS is the smoking population. Some studies have suggested that patients who smoke are less responsive to therapy; however, evidence about whether smoking is associated with the pathogenesis of this skin disease is still non-definitive.
Socioeconomic Factors
Patients with hidradenitis suppurativa are affected by lower socioeconomic status than age and gender-matched controls in studies performed in the United States and in the Netherlands. This status can affect management options, effective follow-up, and lead to a negative cycle of events including decreased work productivity, short- and long-term disability, and increased work absenteeism, all of which can result in cumulative life course impairment.
Clinicians should work closely with their patients to address factors that may be leading to inability to go to work. One of the most common factors associated with HS is pain associated with a patient’s lesions. Patient may miss work due to inability to complete tasks without experiencing recurrent pain, and aggressive medical management is often essential to get pain under control.
Impact of Disease on Patient’s Quality of Life
Assessing Socioeconomic Factors During Visits
HS is a chronic disease that can impact a patient’s quality of life. Pain and drainage secondary to HS are often reported as reasons patients miss work. In clinical management, socioeconomic status should be assessed for its potential impact on patient care. Inquiry about the patient’s occupation and the daily tasks they perform may yield important information about patients who miss work due to experiencing HS lesion pain and drainage, especially while doing physical work.
There are various healthcare resources for optimizing care in patients with low socioeconomic status, including offering free counseling services for weight loss, diet, and smoking cessation. Additionally, the physician can provide different online sources for patients to find low-cost wound dressings and medication discounts. When discussing management options with the patient, low health literacy should be taken into account with low socioeconomic status. The physician may provide an HS overview handout with simplified explanations and go over it with the patient during the initial visit.
Physicians can offer short-term treatment regimens in addition to maintenance therapy for patients to optimize their quality of life. In addition to medical management, physicians may be requested to provide letters of medical necessity on behalf of their patients to adjust their work tasks to lower the risk of HS-related pain and/or drainage. Requested changes may include changing the patient’s work desk to a standing work desk if the patient reports HS-related pain secondary to HS lesion in the groin and buttocks region. Additionally, patients may benefit from having their work tasks spaced out if they include physical work, to prevent constant HS lesion-related pain.
Disability Secondary to Hidradenitis Suppurativa Disease
Patients may also seek disability status due to the effects of their disease. In a 2018 U.S. cohort study comparing patients with HS ( n = 1204) to those without ( n = 6020), patients with HS had statistically significant more disability-related costs and days missed from work compared to the control group.
Physicians can collaborate with the patient’s primary care doctor, who, in our practice, is usually the provider who corresponds with the patient when applying for disability. As mentioned in the previous section optimizing the patient’s medical care can assist them in being able to improve their ability to go to work. Physicians can adjust a patient’s medication regimen while the primary care doctor can determine whether the patient requires pain medication as well. It may take weeks to months to optimize the patient’s medication regimen. Once this is achieved, the patient’s pain medication can be gradually tapered.
Determining Management Options
Treatments Based on Hidradenitis Suppurativa Disease Level of Severity
The Hurley staging system and HS PGA scoring system can be used in combination for determining treatment options. The HS PGA scoring system is good for assessing the patient’s current disease severity.
Patients with mild HS disease may only require topical treatment with maintenance or short-term antibiotic courses. Topical treatment options include clindamycin and clobetasol. Antibiotics used for maintenance include doxycycline, minocycline, and amoxicillin. Short-course antibiotic options includes Augmentin, which may used with a prednisone taper. Additionally, spironolactone is often used for patients with mild HS disease located predominantly in the groin region, which was discussed earlier in this chapter. Spironolactone can be used for females with peri-menstrual HS flares. If pursuing this option, the clinician should make sure the patient is on some form of contraception due to the potential birth-defects associated with spironolactone. Low-androgen containing OCPs can also be used for patients with peri-menstrual flares.
Patients with moderate HS disease may be started on maintenance antibiotics with short-term intermittent prednisone taper based on HS flare frequency. Based on the Hurley staging, patients can also be transitioned to biologic therapy. Adalimumab is currently considered the first-line biologic for moderate-to-severe HS disease. However, if patients do not respond to this biologic, the 40 mg/wk dosing can sometimes be increased off-label to 80 mg/wk. Patients should be aware that it can take a few months to determine treatment efficacy for each dose change. If patients report having HS flares that are uncontrolled with their current therapy, they can be offered intralesional kenalog injections at the affected lesion sites.
Patients with severe HS disease should be assessed for starting systemic therapy. Therapies to consider include adalimumab, infliximab, methotrexate, tofacitinib, and acitretin, among others. Adalimumab will generally be the first treatment choice followed by infliximab if adalimumab is not effective. Infliximab, can be increased to 10 mg/kg every 4 to 6 weeks if needed. Methotrexate is another treatment option for patients with persistent HS disease. Other biologics that are currently being studied for HS includes secukinumab and guselkumab. There are currently three clinical trials for secukinumab. Guselkumab is currently being studied in one clinical trial and two open-label studies for HS. Cases reported in the literature for secukinumab or guselkumab used dosing similar to psoriasis and demonstrated improvement. Methotrexate has been shown to be more effective as monotherapy compared to being used with other systemic therapies for HS. Tofacitinib has been shown to work for some patients, but there is less long-term and large cohort evidence for supporting its use. Patients who have been unresponsive to common HS systemic therapies may respond to tofacitinib after several months. Acitretin is another systemic therapy option that is primarily used for patients with comedonal pattern to their HS disease.
Treatment Options Based on Patient’s Comorbidities
Inflammatory bowel disease has been reported in patients with HS as a comorbidity. Patients who have Crohn’s disease, for example, may be on infliximab or adalimumab for their condition at the time of initial HS evaluation. Since these biologics can also help their HS disease, they can be continued on this regimen and potentially have the dose and frequency increased if their disease does not improve. Another comorbidity to consider is PCOS. Patients may be placed on metformin, which may help their HS. Spironolactone is also used for hirsutism related to PCOS. Patients can be started at a low dose with gradual dose increase based on response.
Patient Co-Management with Other Specialties
Management of patients with HS often involves continued communication between the clinician and the patient’s other providers. Multi-disciplinary care team may include surgical specialists, OB/GYNs, gastroenterologists, and primary care doctors. If a patient’s treatment regimen is being changed, the clinician should notify the patient’s other providers when this change may affect their other comorbidities.
Patient Follow-Up and Lab Monitoring
Treatment Initiation and Baseline Labs
Prior to starting biologic therapy, patients should obtain baseline labs. This includes complete blood count with differential, complete metabolic panel, tuberculosis test, hepatitis B and C panels, and HIV screening test (in patient populations determined to have baseline risk). For patients who will be starting spironolactone, potassium levels should be checked if they have risk factors for hyperkalemia, such as a cardiac comorbidity. Adalimumab serum trough levels and anti-drug antibodies detection are available for monitoring. However, these levels are not typically used in the routine clinical setting.
Abnormal Labs in Hidradenitis Suppurativa
Hidradenitis suppurativa presents with an inflammatory chronic state that can be seen in monitoring labs. Patients will often have elevated white blood cell (WBC) count, elevated platelet count, and/or low hemoglobin lab values on baseline labs. These lab results are all inflammatory markers that are also seen in other inflammatory chronic diseases. One way to evaluate infection versus chronic elevation is by comparing the patient’s baseline and general WBC trends with the current WBC count. If there is a clinically significant increase in WBC count, then it may be important to further evaluate the patient for an underlying infection. Trending elevated platelet counts and low hemoglobin lab values also support the general pattern that accompanies elevated WBC count. If patient has other risk factors that could contribute to an elevated platelet count or low hemoglobin, these factors should be further evaluated.
Follow-Up Based on Current Treatment Regimen and Response
Patients should have follow-up visits based on their disease severity and current treatment regimen. Patients on systemic therapies should be seen more frequently to assess treatment response. At systemic therapy initiation, patients can be seen every 3 to 4 months followed by every 6 months after treatment response. Patients on maintenance therapy with stable disease can be seen every 6 months or sooner if needed for HS flares.
Monitoring According to Treatment Regimen and Comorbidities
Patients on systemic therapies require lab monitoring. It is recommended that patients undergo tuberculosis screening annually after starting immunosuppressive therapies. They should also be monitored for any signs of infection or malignancy for further evaluation. The clinician can perform an annual full-body skin exam for patients on biologic therapy for skin cancer screening, including evaluating for squamous cell cancer in severely affected HS lesions. Clinicians should continue collaborating with the patient’s other providers for the patient’s comorbidities. This includes notifying them of any pertinent treatment changes, such as changing the infliximab dose in a patient with Crohn’s disease. Multi-disciplinary care can optimize the patient’s care by including everyone’s input, including that of the HS clinician (dermatologist), patient, and other providers (i.e., patient’s primary care doctor). Since HS is a chronic skin condition, clinicians have the opportunity to develop a great rapport with their patients and ultimately become part of the patient’s primary medical care follow-up.
Conclusion
HS has variable patient presentation, including age of onset and disease severity. Taking medical history is a major component of clinical evaluation and can help determine risk factors for flare, comorbidities, and inform treatment planning. The physical exam, in addition to the DLQI and pain assessments, provides a baseline assessment that ideally is reassessed at every visit in a standardized manner to evaluate treatment efficacy. Socioeconomic status and health literacy should be integrated into management planning and discussion in order for patients to receive optimal care. The dermatologist also can play an important role, providing management input for their patients in interdisciplinary team HS care. Follow-up depends on treatment choice, disease severity, and lab monitoring. HS management is a rewarding experience for clinicians, as it allows them to develop plans that greatly aid patients while developing long-term rapport.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








