10 Cheek and lip reconstruction
Synopsis
Lip reconstruction
 Accurate three-layered closure of lip defects is imperative to preserve function.
Accurate three-layered closure of lip defects is imperative to preserve function.
 Local tissue should be used whenever possible.
Local tissue should be used whenever possible.
 Small defects can be closed by direct repair:
Small defects can be closed by direct repair:
 Intermediate defects are best reconstructed with local flaps.
Intermediate defects are best reconstructed with local flaps.
 Total or sub-total lip defects are best reconstructed with free tissue.
Total or sub-total lip defects are best reconstructed with free tissue.
Introduction
Because it represents the principal aesthetic feature of the lower face, subtle changes in the appearance of the vermillion border, labial commissures, or Cupid’s bow are readily visible. For that reason, surgical resection of lip cancer, or trauma resulting in lip laceration or soft tissue loss, frequently result in alterations of normal lip appearance and function that can have a profound and lasting effect on the patient’s self-image and quality of life. Neuromuscular injury or dysfunction can cause asymmetry at rest and particularly during facial expression. This can lead to distressing functional disability. Loss of labial competence may be characterized by impairment in the ability to articulate, whistle, suck, kiss, and, probably most importantly, to control salivary secretions with consequent drooling. Surgeons have long appreciated the significance of lip function and aesthetics and many creative surgical techniques have been devised to reconstruct various lip defects. These techniques have evolved, and newer procedures have been developed that effectively address small to moderate defects. However, while many of the current techniques work well for small to moderate lip defects, the ultimate reconstructive approach for larger defects of the lip has remained elusive, and currently available methods provide results that are less than optimal.1 While the lips have a very specific appearance and are such a prominent part of our physiognomy, the cheek, by comparison is, to a large extent, without a distinguishing feature. The nasolabial fold establishes the junction or interface between the cheek and lip and is an important part of the aesthetic appearance of the face. Symmetry of the nasolabial folds is also important in presenting a harmonious appearance to the face. While cheek reconstruction does not compare in intricacy and visual impact with lip, nasal, or eyelid reconstruction, symmetrical and balanced reconstruction is, nevertheless important. The slightly more lateral position of the cheek in the face allows for some leeway in our reconstructions. Both cheeks are never seen, in their entirety, together. This is in contrast, for example, to the lips where right and left sides are instantly comparable. As long as the nasolabial folds are symmetrical, a reasonably accurate replica of the intact contralateral cheek will result in a very satisfactory reconstruction, while a less than accurate lip reconstruction will provide a less than satisfactory result. The cheek consists of a soft tissue envelope of skin, subcutaneous tissue, muscle, and buccal mucosa draped over a bony framework, the most prominent part of which is the malar eminence. The parotid gland and duct as well as the facial nerve are embedded within this soft tissue. The texture of the cheek differs between male and female. In the female, it is smooth and soft. In the male, it is partially hair-bearing and less smooth. Probably the most important feature to consider when planning cheek reconstruction is skin color. While reconstructions in general terms are planned based on factors such as defect size and flap availability, in the head and neck in general and in the face in particular, we must also consider the fact that our reconstruction is going to be clearly visible. A cheek reconstruction can be marred, for example, if the skin color is strikingly different from the rest of the face. One final point is important to consider here; while we can think of the cheek as a separate aesthetic unit, reconstruction of the cheek will frequently impact on nearby units, e.g., the pull on the lower eyelid from a cheek advancement flap. Reconstruction of the underlying bony skeleton is obviously also an important part of cheek reconstruction. The integrity of the contour of the underlying bony skeleton is important in maintaining facial symmetry. Bony reconstruction of the cheek is seldom an isolated necessity, particularly in the context of tumor ablation and reconstruction. In this situation, we are generally dealing not only with the bony cheek but with the whole maxilla. This brings us into the area of orbital palatal and nasal reconstruction. A detailed description of maxillary reconstruction is beyond the scope of this chapter but it is important to realize that the two – cheek and maxilla – cannot always be separated.
History
In 600bc, Sushruta, an Indian surgeon, published the first written description of lip reconstruction.2 Most of the reconstructive techniques in present use are modifications or refinements of techniques that were described in the medical literature over the past 2 centuries. In 1857, Victor von Bruns described the use of bilateral superiorly based nasolabial flaps for reconstruction of the lower lip.3 These full-thickness flaps, however, led to denervation, not only of the remaining lower lip, but of the upper lip as well. Von Bruns actually refined his technique and ultimately described a technique almost exactly similar to that described by Karapandzic.4 This technique eliminated full-thickness extension of the flap through the labial mucosa, emphasizing preservation of sensory and motor nerve fibres. Gillies fan flap is a refinement of another approach advocated by von Bruns that employed two quadrilateral, inferiorly-based nasolabial flaps.3,5 Understanding the rationale of these techniques is important because refinements of these various techniques continue to appear in the literature.
Anatomic and functional considerations in lip reconstruction
The laminar structure of the lips consists of three layers: mucosa, muscle, and skin. Externally, the cutaneous portion of the lip surrounds and transitions into the mucosal lip. This transition between these two regions is characterized by the mucocutaneous ridge, or vermillion border. At the midline of the upper lip, there is a V-shaped indentation of the mucocutaneous ridge that is known as Cupid’s bow. Above Cupid’s bow, a vertical groove-shaped depression called the philtrum is bordered on either side by elevations known as philtral ridges or columns (Fig. 10.1). The vermillion forms the major aesthetic feature of the upper and lower lips. The vermillion is composed of modified mucosa that lacks minor salivary glands. The characteristic color of the vermillion stems from a rich blood supply that underlies a very thin epithelial structure. The maxillary and mandibular divisions of the trigeminal nerve provide sensation to both upper and lower lips. The boundaries of the upper lip are defined by the base of the nose centrally and by the nasolabial folds laterally. The inferior margin of the lower lip is defined by the mental crease (labiomental crease) that separates the lip from the chin.6 The upper and lower lips differ, in that the lower lip is composed of a single aesthetic unit while the upper lip has multiple subunits. According to Burget and Menick’s description,7 each side of the upper lip has two aesthetic subunits: the medial topographic subunit is one-half the philtrum, whereas the lateral subunit is bordered by the philtrum medially, the nostril sill and alar base superiorly, and the nasolabial fold laterally. Another way to think about the upper lip is that it is composed of three subunits, the philtrum centrally and the lateral lip elements on either side of the philtrum (Fig. 10.1).8
The thickness of the lip largely results from the underlying orbicularis oris muscle, which forms a functional sphincteric ring and is essentially sandwiched between the skin on the outside, and the mucosa on the inside. The orbicularis oris has two functions that, at first might seem diametrically opposed but that, on reflection make sense. The superficial fibers of this muscle function to protrude the lips away from the facial plane, whereas the deep and oblique fibers approximate the lips to the alveolar arch.9 The middle portion of the buccinator muscle extends anteriorly to the corner of the mouth and decussates so that the upper fibers of the mid-buccinator merge with the orbicularis fibers of the lower lip, and the lower fibers merge with the orbicularis fibers of the upper lip.9 Several muscles elevate the lip. The two most important elevator muscles are the zygomaticus major and the levator anguli oris; the zygomaticus minor and the levator labii superioris also contribute to this function. The depressor muscles include the depressor anguli oris and the platysma, with minor contributions from the depressor labii inferioris. Variations in the contraction of all of these muscles result in the versatility of movement of this region and the myriad of shapes and expressions that contribute not only to facial aesthetics and animation but also to function. The modiolus is just lateral to the oral commissure. It is a 1 cm-thick fibrovascular region of muscle fiber intersection of the levator muscles and the depressor muscles that attach firmly to the dermis approximately 1.5 cm lateral to the oral commissure. The modiolus can be located by compressing the skin and mucosa of the commissure using bidigital palpation with the thumb and index finger.10 The appearance of the labial commissures is significantly affected by movement of the modiolus on each side, which results from the summation of opposing contractile forces of the levator muscles (zygomaticus major and levator anguli oris) and the depressor muscles (depressor anguli oris and platysma).11,12 Sometimes there is a dimple here. When present, the dimple results from a dermal insertion arising from the inferior muscle bundle of a bifid zygomaticus major muscle.13,14 The elevators and depressors of the lips are innervated by the buccal and mandibular branches of the facial nerve, respectively. Disruption of the musculature that attaches to the modiolar region (or their neural supply) can alter the appearance of the labial commissure at rest and during function secondary to imbalanced muscular contraction. This gives a very abnormal appearance to the mouth and is one of the greatest complaints of patients with facial paralysis. Modiolar motion can be analyzed to measure the success of facial reanimation in these.15
The blood supply to the lips comes from the facial arteries, which give rise to the inferior and superior labial arteries. The variability of these vessels, both in terms of course as well of presence, has been shown by anatomic studies and dissections. The superior labial arteries from each side generally anastomose in the midportion of the upper lip, coursing between the mucosa and orbicularis muscle in some patients and through the muscle in the others.16 The inferior labial artery, on the other hand, routinely courses between the mucosa of the inner aspect of the lip and the muscle.16 Two separate cadaveric studies found that the inferior labial artery was absent on one side in 10% and 64%, respectively, of the cadavers evaluated.16,17 The bilateral presence of inferior labial arteries was not always predictive of an end-to-end anastomosis between these vessels, and other arterial branches from the facial arteries were frequently identified (e.g., labiomental, sublabial arteries).16,17 Even though the variable arterial distribution of this region could, at least in theory, affect the survival of reconstructive procedures involving the lip, local flap reconstruction has been performed for centuries with predictably excellent survival rates. Although the lips are an important aesthetic feature of the lower face, they also play an important role in facial expression. Oral competence is necessary for eating and drinking, and intact neuromuscular function is essential for speech articulation and other functions such as whistling and sucking. The lower lip functions as a dam that retains saliva and prevents drooling. The upper lip contributes to oral competence by providing opposition to the lower lip to effect closure.18 Sensation allows the lips to monitor the texture and temperature of substances prior to oral intake.
Lip function
The lips are an important aesthetic feature of the lower face and any deformity of the lips is instantly recognizable. Even minor deformities are easily noticed. More important though are the functional characteristics of the lips. The lips play a very important part in speech articulation, as any of us who have tried to speak after extensive local anesthesia at the dentist can attest. Also the lips are vital for the maintenance of oral competence.18 Sensation allows the lips to monitor the texture and temperature of substances prior to oral intake.
Patient selection and presentation
Goals of lip reconstruction
The goals of lip reconstruction (Box 10.1) are several. The most important of these is function. No matter how good a reconstructed lip looks, if it cannot maintain oral competence, the reconstruction is a failure. Maintenance of oral competence is vital. Similarly important is maintenance of an adequate oral aperture to facilitate oral hygiene and/or to accommodate removable dentures. The labial vestibule is an important feature of labial anatomy and its preservation or re-creation is important for oral hygiene, dental care and denture fitting. In order to achieve these functions, preservation of labial sensation is important and because of the vital role of the lips in facial aesthetics, maximization of cosmesis is one of the key goals of reconstruction.19
In situations where the orbicularis oris muscle has been disrupted, it is vitally important to restore continuity of that muscle if at all possible. Careful re-approximation of muscle edges with intact motor innervation usually results in complete restoration of dynamic orbicularis function. Although some authors contend that the upper lip functions primarily as a curtain that could be replaced with a static flap reconstruction, there is no doubt that a completely intact sphincter with active function and sensation yields the best functional result.7,20 In cases where reconstruction of the sphincter is not feasible, an adynamic reconstruction must be pursued that provides some degree of oral competence. In repairing or reconstructing the lips, one of the main dangers is resulting microstomia. While patients can function reasonably well with a small degree of microstomia, it is very important to minimize it as may not only interfere with function but it can also hamper oral hygiene and patients should be counseled prior to surgery that denture insertion and removal may be difficult, or, quite simply, not possible. Decreases in the shape or depth of the labial vestibule can exacerbate oral incompetence and drooling, and may preclude patients from wearing a removable prosthesis. Preservation of labial sensation is vitally important to maximize oral competence and to fulfill its other sensory roles.
Early lip reconstruction techniques focused primarily on primary closure of the surgical defect, whereas more contemporary techniques attempt to address the importance of an aesthetic, functional result. Reconstruction of the aesthetic subunits as described by Burget and Menick7 is helpful, and aesthetic features such as Cupid’s bow and the philtral columns must be carefully restored. Failure to restore these landmarks results in an abnormal appearance that is instantly detectable. One of the features that is readily picked up by the human eye is asymmetry. Surgery that results in asymmetry is typically more noticeable than symmetric alterations. As an example, rounding of both commissures is less obvious than rounding of one side. Whenever possible, the height, projection, and relationship between upper and lower lips should also be preserved or replicated. This is most easily achieved by using tissue from the adjacent or opposing lip.21,22
Patient selection is, arguably, less important than reconstructive choice. In the case of trauma, the damage is already done and the surgeon’s task is to repair and reconstruct the lip so that it is as functional and aesthetically pleasing as possible. For patient’s facing lip resection for disease, the task is no different, i.e., the surgeon must reconstruct the lip to be as functional and aesthetically pleasing as possible. However, in the latter case, the surgeon has the luxury of planning what reconstruction will best suit the patient. The choice depends on multiple factors, such as prognosis, general medical condition, availability of local tissue, history of prior radiation as well as co-morbidities. The lips are somewhat unique however, in that the need to reconstruct the lips is very different from, as an example, the need to reconstruct a breast. Oral competence is vital for normal eating, articulation and communication, so the option not to reconstruct the lip is really nonexistent. The algorithm presented later in this chapter (see Fig. 10.17, below) can be used as a guide in selecting the most appropriate procedure for a given defect.
Operative technique
Defect-specific reconstruction of the lip
Following injury to the lips or following surgical resection for disease, there are several options for reconstruction of the lips:9,23 The first choice, of course, is to use the remaining lip segment and if the defect size allows, this is by far the best option. This choice assumes that there is enough lip to effect the repair while not creating microstomia. Another consideration is whether or not the defect is full thickness and whether all three elements, skin, muscle and mucosa, need to be replaced. Regardless of what the defect is, local tissue is the best option because it replaces what has been lost and is the perfect match in terms of color, thickness and composition. Defects of the upper lip of less than 25% can be closed by direct approximation. For the lower lip, a slightly larger defect, up to 30%, can be closed directly. Once again, care must be taken to ensure accurate closure of all layers. Repair of the orbicularis oris and reconstitution of the circumoral sphincter is the most important aspect of a functional repair.
Defects of the vermillion
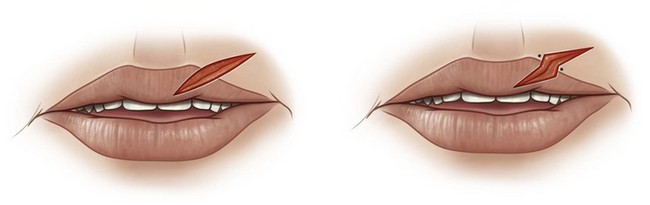
There are a few important points of which to be cognizant when repairing a lip. One is the appreciation of the fact that the human eye can detect asymmetry remarkably accurately. The lips are very symmetrical and the different elements of the lip blend with each other in a very pleasing and aesthetic way. The junction between vermillion and white lip, for example, is smooth and seamless. When the line of the vermillion is broken or when a segment of vermillion impinges on the white lip, the abnormality is immediately obvious. When dealing with lacerations, there is not a lot, in terms of repair options, that the surgeon can do. However, being precise in repair of the vermillion border and white lip roll will produce a scar that is imperceptible. When resecting a lesion that crossed the vermillion, however, there are some options. As surgeons, we know that scars contract and a straight-line scar that crosses the vermillion will not only contract but may possibly produce a visible deformity. In order to avoid this, breaking up the scar by incorporating a step in the excision may prevent this contraction, make the repair easier and minimize the risk of a visible scar (Fig. 10.2).
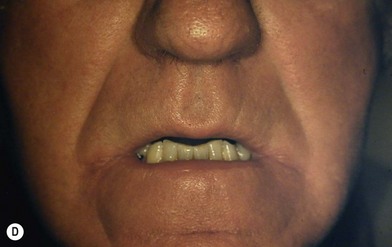
Vermillionectomy is a procedure that is done to remove very superficial lesions in the vermillion, such as superficial squamous cell carcinoma, or to remove dysplastic tissue with malignant potential such as actinic cheilitis. Following vermillionectomy, a procedure that is also known as a lip-shave, reconstruction is achieved by advancing the buccal mucosa to cover the defect and to re-establish the mucocutaneous junction (Fig. 10.3).1 If there is any degree of tightness, back-cuts are made to facilitate further advancement of the mucosa. This type of vermillion reconstruction can sometimes result in excessive thinning of the lip from mucosal retraction or scar contraction, and decreased mucosal sensation.6,24 However, in general, the results of lip shave are excellent. Other approaches to reconstruction of the vermillion include the mucosal V-Y advancement flap, the cross-lip mucosal flap, and transposition flaps harvested from the buccal mucosa or the ventral surface of the tongue.6,25 Buccal mucosal flaps tend to be more erythematous than natural vermillion, resulting in a color mismatch with the remaining vermillion.24 Mucosal tongue flaps require a second procedure 14–21 days later to release and inset the flap. A musculomucosal flap that includes buccal mucosa and buccinator muscle anteriorly pedicled on buccal branches of the facial artery and innervated sensory branches of the infraorbital nerve has been advocated as one option to remedy the loss of sensation in defects that also include loss of orbicularis muscle.26
Small full-thickness defects
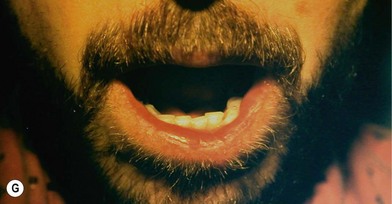
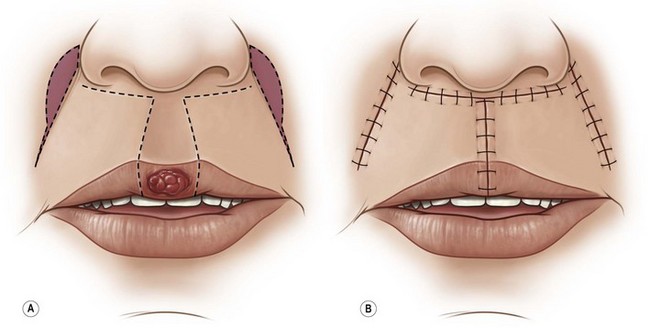
Primary closure of defects that involve as much as one-quarter of the upper lip or one-third of the lower lip can be achieved (Box 10.2).18 A V-shaped wedge design usually permits closure of smaller defects, whereas a W-plasty placed at the base of the V facilitates the closure of larger defects. Furthermore, this modification will generally allow for the scar to be kept above the mental crease. This improves the cosmetic appearance of the repair, as it preserves the integrity of the chin aesthetic subunit (Fig. 10.4). Wedge-shaped defects of the lateral lip should be more obliquely oriented so that the line of closure parallels the relaxed skin tension lines. If a W-plasty is incorporated into a lateral lip defect, the angle formed by the lateral V-shaped subunit of the W should be larger and more obliquely oriented than the medial subunit to properly align the closure.6,19 Careful attention to meticulous closure of all three layers will ensure optimal cosmesis and function. If actinic cheilitis of the adjacent lip is present, vermillionectomy can also be performed in combination with the wedge excision, using a labial mucosal advancement flap to recreate the vermillion border (Fig. 10.5). This technique provides an elegant reconstruction of the vermillion, and the cosmetic outcome of this procedure is usually excellent. The aesthetic result following repair of a V-type excision is often less satisfactory in the upper lip, because the upper lip is able to withstand much less tissue loss before tightness becomes clinically apparent and the normal overhang of upper and lower lip is lost as a consequence of closure-induced tension. In addition, the anchorage of soft tissues around the pyriform aperture to the underlying bony skeleton limits compensatory movement of the remaining lip. This problem can be minimized by using a T excision, which facilitates advancement of the lateral lip elements. The symmetry of Cupid’s bow is easily lost with even minor excision in the region of the philtrum. Webster’s27 technique of crescentic perialar cheek excision is an extension of the T-excision technique that increases upper lip movement without disturbing the lateral muscle function (Fig. 10.6). If the defect is created lateral to the philtral columns, primary closure may produce deformity and notching. For this reason, it is occasionally preferable to use a lip-switch flap from the lower lip, even when the defect makes up less than 30% of the lip’s width. This is particularly the case in younger patients whose tissues are less lax and where cosmesis is often of even greater importance.
Box 10.2
Wedge resection of the lip: technical tips
• Up to 25% of the upper lip can be resected and repaired directly.
• Up to 30% of the lower lip can be resected and repaired directly.
• Careful approximation of the muscle layer ensures a functional repair.
• Consider a W resection for larger wedges in order to keep the scar above the mental crease.
Intermediate full-thickness defects
For all the reasons already described, local flaps are the best option for reconstructing larger defects involving up to two-thirds the width of either upper or lower lip. These flaps involve either a lip switching maneuver, rotation of tissue from one lip to another or recruitment and advancement of adjacent tissue, such as cheek tissue to achieve the reconstruction. Lip-switch (cross-lip) flaps are axial flaps based on the labial arteries (Box 10.3). They replace tissue like with like, replacing the trilaminar defect in one lip with tri-laminar tissue from the other. The classic Abbé flap can reconstruct medial or lateral lip defects with a full-thickness composite flap that reconstructs all three layers and restores continuity of the vermillion.28
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree