Chapter 2 The Lymphatic Anatomy of the Lower Eyelid and the Malar Region of the Face
A keen understanding of facial lymphatics is the missing link in the anatomy of facial injections. This knowledge equips the injector with a secret weapon in their armamentarium to prevent suboptimal aesthetic outcomes secondary to prolonged lymphedema. In particular, this emphasizes the importance of injection depth in the midface.
We would like to thank Dr. Shoukath and Professor Ashton for their fantastic work on facial lymphatics, a series of findings relevant to the injector and fat grafting surgeon. Iatrogenic persistent periorbital edema may be the result of lymphatic injury, lymphatic fouling, or possibly particle cohesivity in the case of hyaluronic acid fillers. Cannula techniques for volume placement in the prezygomatic space, when entered laterally in a mobile segment of the periorbital, should provide safety as the cannula is directed toward malar periosteum and then advanced medially. Sharp needle injection in the region of the bilamellar orbital retaining ligament poses some risk of injury or impingement of the deep lateral lymphatic channel. Based upon anatomic dissections in the region of the zygomaticomaxillary retaining ligament, the caudal border of the prezygomatic space is a series of osteocutaneous ligaments, rather than a membranous structure as is present cephalad in the orbital retaining ligament. As such, volume-based procedures near the caudal aspect of the prezygomatic space would theoretically be less prone to an impingement since the lymphatics do not pierce a dense anatomic structure.
—Jerome P. Lamb and Christopher C. Surek
Introduction
Our knowledge of the human lymphatic system is predominantly based on the pioneering work of Sappey 1 1 and his successors 2 in the 19th and early 20th centuries. This is because the lymphatic system is extremely difficult to study; the vessels are small and fragile, and the presence of multiple valves makes retrograde filling of the lymphatic system for radiographic analysis impossible.
Recent advances in the imaging of the lymphatic system, particularly the use of hydrogen peroxide, have allowed for new studies of lymphatic architecture that were previously not possible. 3 This is important because many of the questions concerning lymphatic anatomy are not answered by the existing literature. 4
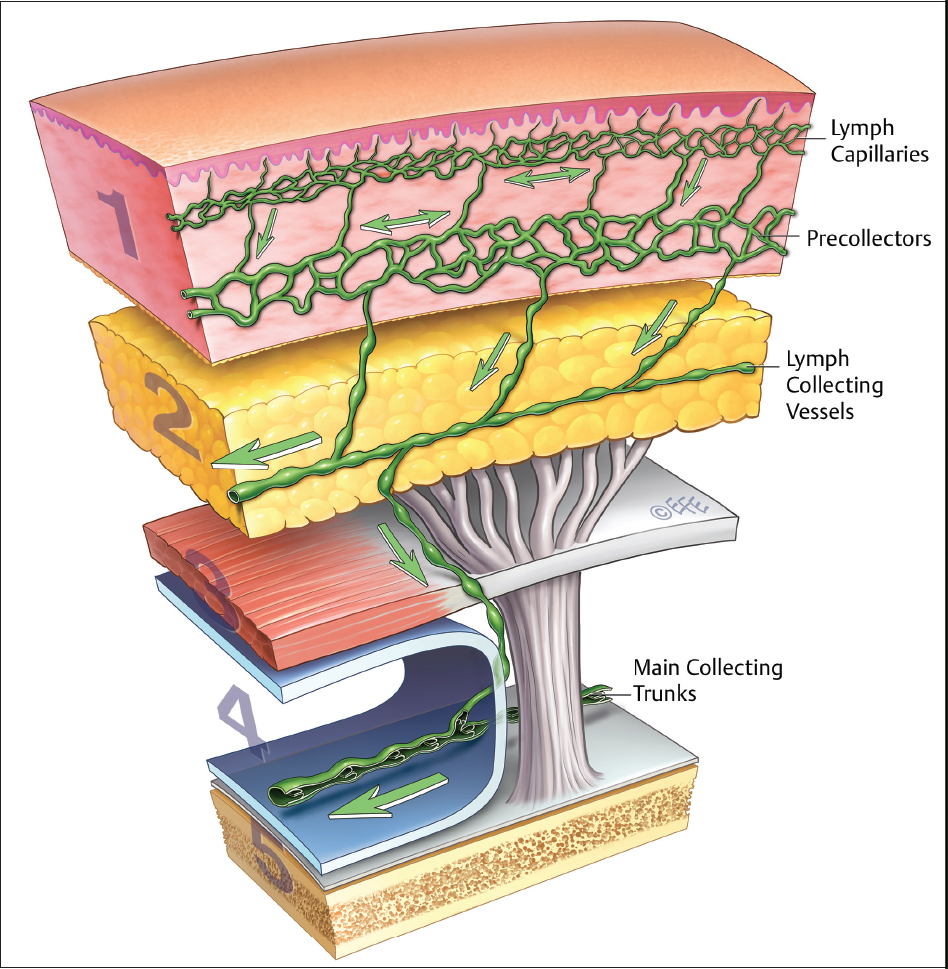
Analogous to the venous system, the lymphatic system of the human body is initially composed of a very fine capillary network, the vessels of which measure only 20 to 70 µm in diameter. 5 This network subsequently drains into larger “precollecting” vessels (70–150 µm) located in the deep dermis. Both the “capillaries” and “precollectors” are avalvular. From here, lymph is directed more deeply into lymph “collecting” vessels. These are larger, measuring 150 to 350 µm, and most importantly contain multiple valves that serve to direct lymph to a predetermined, singular and specific “sentinel” lymph node. 6
Facial Lymphatics
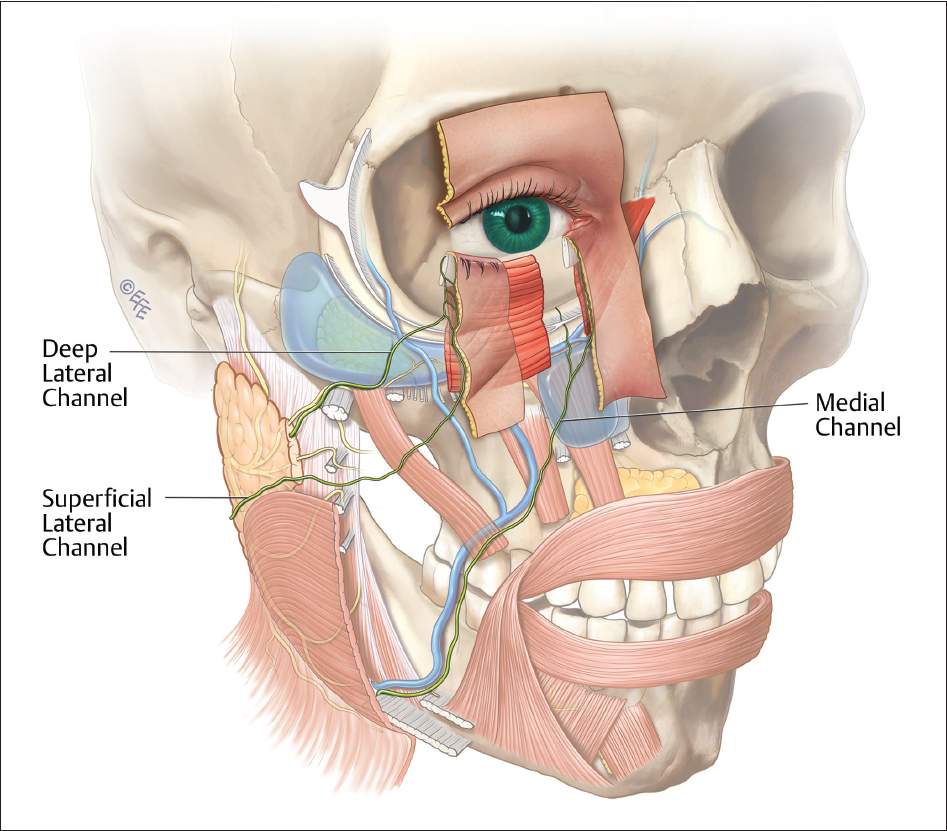
Within the face, lymphatic fluid is primarily directed to the parotid and submandibular lymph nodes. 7 It does so via a superficial and deep series of collecting vessels that are consistent and predictable in their location. Knowledge of the location of these collecting vessels is critical in facial revolumization procedures as the fragile and compressible nature of the collecting lymphatic vessels means that they can be easily occluded, leading to subsequent lymphedema in the tissue they drain ( Fig. 2.1 ).
The lower eyelid and its conjunctiva is particularly susceptible to lymphedema and chemosis. Indeed, the recent trend to more aggressive surgery around the lateral extent of the orbital retaining ligament (ORL) has been accompanied by an increase in postoperative periorbital chemosis. As an example, published complication rates of persistent chemosis beyond 2 to 3 weeks have risen from a traditional low rate of 0.8 to 1% 8 to up to 34.5% in one series recently published. 9 In each published series, the increased chemosis rate was accompanied by more aggressive surgery in the lower eyelid, the ORL, and the malar complex.
We know that arteries, nerves, and veins cross tissue planes at points of ligamentous fixation. We also know that the face can be divided into five distinct tissue layers ( Fig. 2.2 ) and that the location of nerves and arteries within these planes is consistent. 10 Elsewhere in the body, the precollecting lymphatic vessels are located in the deepest subsection of layer 2, called 2C. 5 The main collecting trunks travel in layer 4. 5 The face is no different. The capillary network within the conjunctiva of the lower eyelid and eye drains into precollectors in the deep dermis of the conjunctiva and travels superficial to the preseptal orbicularis oculi muscle in the same layer (2C). Broadly, these precollectors fall into two groups: those orientated toward the medial canthus (the medial system) and those directed toward the lateral canthus (the lateral system).
At the medial third of the ORL, the medial system of precollectors coalesces to form a collecting trunk, which turns inferiorly, and travelling within a discrete fat compartment, continues within the nasolabial fat compartment 11 to drain into the submandibular lymph node. The lateral group of precollectors coalesce at the lateral third of the ORL and turn inferolaterally within the lateral orbital fat compartment 11 to drain into the preauricular lymph nodes. 12 These two medial and lateral systems comprise the superficial lymphatic system.
As would be predicted, there is an additional system of lymphatic vessels running deep to the orbicularis oculi muscle, that is, in layer 4. This deep system drains the lower eyelid and upper mid cheek directly from precollectors traveling through the tarsal plate and Meibomian glands in the lateral third of the lower eyelid. This deep lymphatic system is joined by connections with the superficial lymphatic system by precollectors that travel directly through the preseptal orbicularis muscle to link the superficial system in layer 2 with the deep system in layer 4.
Lymphatic precollectors of the deep system travel beneath the preseptal orbicularis. Laterally, in the lateral lower quadrant at the junction of the ORL and the lateral orbital thickening (LOT), the precollectors pass through the superficial ORL and coalesce to form larger collecting lymphatics that travel in the suborbicularis oculi fat (SOOF) within the roof of the prezygomatic space. At the level of the most cranial zygomaticocutaneous ligaments (ZCL), that is, at the point of fixation, the collectors vertically descend into the preperiosteal fat surrounding the origin of zygomaticus major (ZM). There, the lateral deep collectors descend beneath the deep fascia to travel with the facial nerve to reach the preauricular lymph nodes within the parotid.
An equivalent medial deep facial lymphatic system has not been identified despite extensive searching. Given histological evidence of deep lymphatic vessels in the medial eyelid, it is probable that this system also exists but may be smaller or less developed than the lateral system.
Thus, there are three main lymphatic channels of the lower eyelid and mid cheek. Lymphatic channels within the medial lower eyelid coalesce to form a superficial medial system, while the lymphatics of the lateral eyelid form both a superficial and a deep lateral system of lymphatics. The medial system drains to the submandibular gland, and the lateral system drains to the parotid.
As would be predicted from elsewhere in the body, the capillary network and the precollectors located within the conjunctiva are avalvular and there is free communication between the medial and lateral eye. There is also a free communication between precollectors of the lower and upper eyelids around the lateral canthus. Our studies would suggest that the majority of lymphatic drainage from both the upper and lower eyelids is through the lateral system. 6 , 7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree