Case 9 Nose Reconstruction
9.1 Description
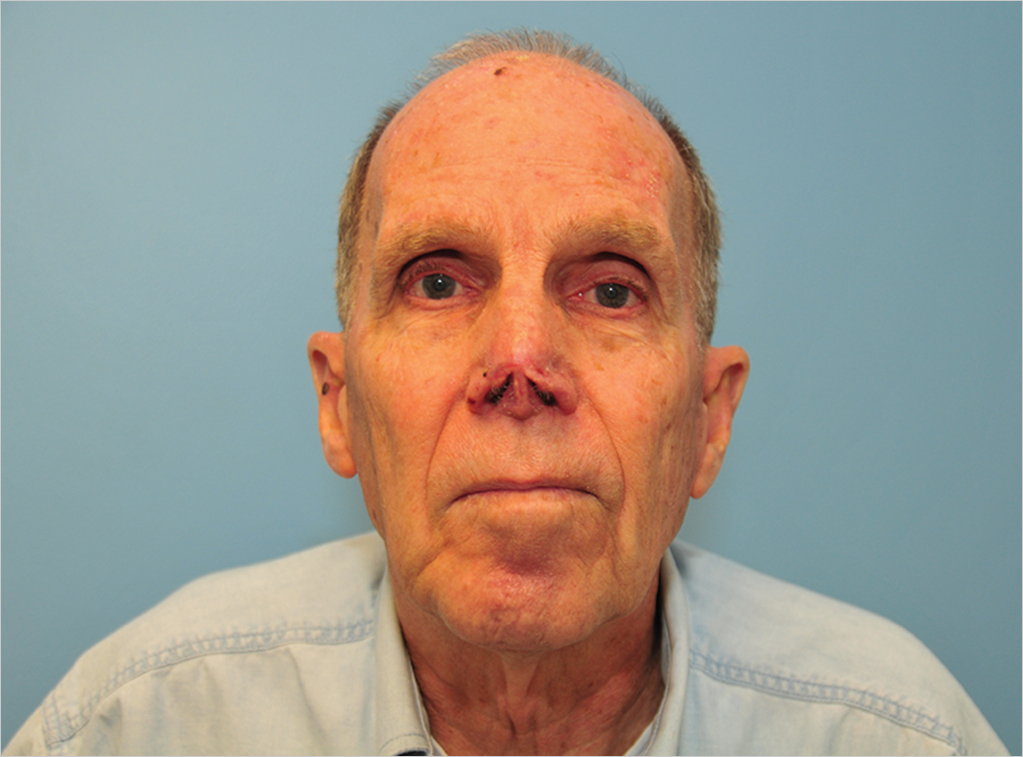
Evidence of amputation of the nasal tip, involving skin, cartilage, and mucosa
The structural framework and nasal lining have been violated
Defect primarily involves one nasal subunit, the tip, but also looks to have some extension into the columella
9.2 Work-Up
9.2.1 History
Sun exposure history
History of facial surgery, especially surrounding the nose
Previous surgery may affect reconstructive options
Medical issues that may affect healing: History of radiation, chemotherapy, immunosuppression, smoking, and diabetes
Personal and family history of skin cancer
9.2.2 Physical Examination
Detailed evaluation of nose and surrounding face to assess the lesion or defect
Characterize findings associated with skin lesion (if present): Size, color, shape of lesion, skin irregularity, and hyperkeratosis
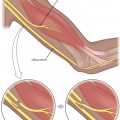
If resected, evaluate for size and shape of the defect, nasal subunits involved, depth of excision (cartilage or mucosal involvement), presence of perichondrium on cartilage, laxity of surrounding skin, and involvement of nostril sill
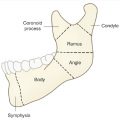
If there is cartilage loss, assess for donor sites: nasal septum, ear, rib
9.2.3 Diagnostic Studies
If patient presents initially without previous treatment, a biopsy should be performed at the time of evaluation to establish a diagnosis
Full-thickness incisional versus excisional biopsies may be performed.
Avoid shave biopsies as they may lead to incomplete assessment of the lesion, particularly in melanoma, where the depth of a tumor is critical to prognosis.
9.3 Patient Counseling
The nose is a complex three-dimensional structure and some deformity should be expected following excision, even with the best reconstruction.
While flap reconstructions may yield the most aesthetic results, it is reasonable for some patients (e.g., medically complicated, elderly) to opt for simpler skin graft reconstructions or even no reconstruction at all.
Skin graft may be a reasonable temporizing option until definitive pathology confirms negative margins.
9.4 Treatment
Consider Mohs surgery consultation, if available
The technique allows examination of entire surgical margin and cure rates of up to 98%
Board examiner may require that you excise the lesion yourself
In melanoma, surgical oncology consultation is recommended
9.4.1 Excision
(See Chapter 7, Table 7.2)
Basal cell carcinoma: 2–5mm margin
Squamous cell carcinoma
4mm margin if low risk: <2 cm lesion, well-differentiated, not invasive
6mm margin if high risk: >2 cm, poorly differentiated, invasive into fat
Melanoma: Excision margins determined by Breslow thickness
In situ: 5mm margin
≤1 mm: 1 cm margin
>1–2 mm: 1–2 cm margin
>2 mm: 2 cm margin
Sentinel lymph node biopsy: Consider for 0.8–1 mm thickness or <0.8 mm with ulceration. Recommended for >1 mm thickness. (Surgical Oncology consultation)
Stage III melanoma (positive lymph nodes) may require immunotherapy (Medical Oncology consultation)
Final excision margins
Fresh frozen pathologic evaluation is notoriously unreliable and cannot ensure negative margins
Most reliable method of confirming negative margins is with permanent sections. Unfortunately, these sections may take several days to obtain.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree