Nasal reconstruction after resection for cutaneous malignancies poses a unique challenge to facial plastic surgeons. The nose, a unique 3-D structure, not only must remain functional but also be aesthetically pleasing to patients. A complete understanding of all the layers of the nose and knowledge of available cartilage grafting material is necessary. Autogenous material, namely septal, auricular, and costal cartilage, is the most favored material in a free cartilage graft or a composite cartilage graft. All types of material have advantages and disadvantages that should guide the most appropriate selection to maximize the functional and cosmetic outcomes for patients.
One of the most common locations for skin cancer is the nose; the unique 3-D structure of the nose poses a challenge for reconstruction. Nasal defects after resections of cutaneous malignancies are frequently disfiguring and distressing to patients. Without proper reconstruction, it is nearly impossible to hide these aesthetic and functional deformities. The goals of nasal reconstruction are twofold. First, the surgeon must restore the functional and breathing capacity of the nose and maintain or regain the structural integrity of the defect site. Second, the surgeon must strive for an aesthetically pleasing result that is in harmony with rest of the face in terms of texture, color, and form.
The nose may be divided into layers for the purpose of planning reconstruction: (1) cover (skin, subcutaneous tissue, and muscle); (2) structure (upper and lower lateral cartilages, septum, nasal bones, and tip-supporting mechanisms); and (3) internal lining (vestibular skin and nasal mucosa). This article focuses on reconstruction of oncologic defects involving the nasal covering and structure, emphasizing the use of cartilage grafting in such repair.
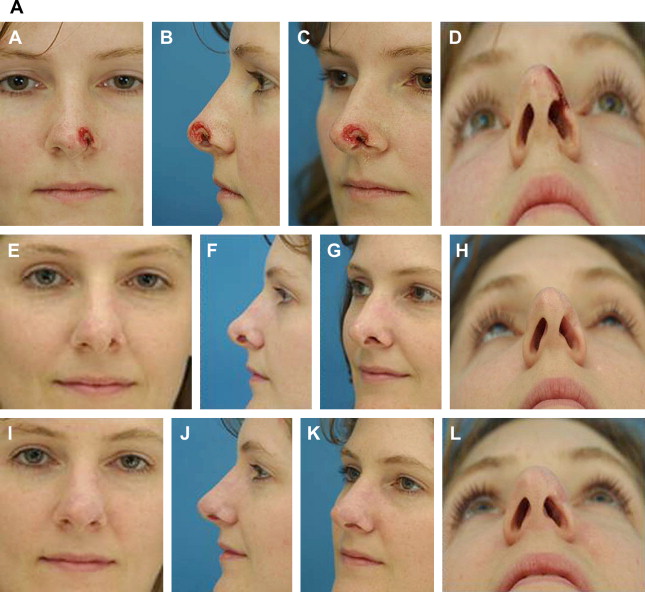
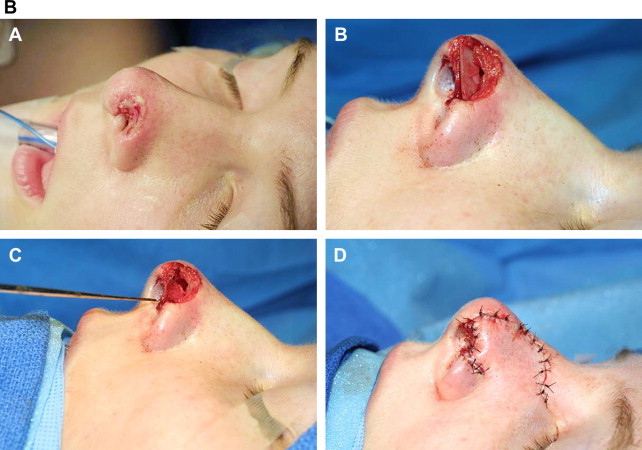
Critical analysis of a defect should precede reconstruction of any wound. The defect’s size, including depth, and location have an impact on nasal function. When the depth is such that native structural support has been removed, the defect uniformly requires reconstruction with composite or cartilaginous grafting. During the analysis stage, the location of the defect is also of utmost importance. The alar rim is one of the free margins that represent an immobile landmark. Normal wound healing and contracture tend to pull the alar rim up and create a notch deformity; thus, appropriate planning is necessary.
The patient’s age, general health, and aesthetic goals must be included in the decision-making process. A thorough medical history, including prior skin cancer, nasal surgery, and head and neck irradiation, should be completed. Both head and neck irradiation and intervening scars may compromise skin flap vascularity. The use of tobacco products cannot be overlooked because it increases the risk of skin flap and graft failure. Although the mechanism of the harmful effects is multifactorial, the nicotine causes vasoconstriction of cutaneous blood vessels with resultant decreased tissue oxygenation.
After resection of malignancy, often large defects are left where the structural integrity of the nose has been disrupted to get adequate margins. In cases of skin, soft tissue, and cartilage losses, the reconstruction requires a graft that restores the forces of the nasal infrastructure but also withstands the substantial mass of soft tissue that may be transferred.
Grafting materials may be categorized as autogenous tissue, alloplasts, and homografts. The senior author Constantinides, favors the use of autogenous materials for nasal reconstruction. Autogenous material is advantageous for several reasons : it has superior long-term survival, is readily available in the head and neck region, and has flexibility when inside the nose. It has proved a safe, effective, and reliable grafting material that does not stimulate an immune response. As a result, autogenous grafts have low rates of extrusion. Autogenous tissue can cause donor site morbidity, however, and potentially resorb over time. Although most commonly seen with rib grafts, warping remains the most feared complication when using any autogenous graft. Situations arise, however, when harvesting such tissue may be deleterious to a patient or is not in sufficient quantity to correct a given defect. Under these circumstances, homografts are a viable alternative. Alloplastic materials also have been used with varying success to augment the nose and serve as a secondary, less acceptable alternative to autografts.
There have been many reconstructive methods described to restore nasal defects after skin tumor excision, including primary repair, healing by secondary intention, skin grafts (split and full thickness), local flaps, composite grafts, free cartilage grafts, and microvascular free flaps. Split-thickness and full-thickness skin grafts can be applied in cases where the defects are superficial, but often the defect left by removal of the tumor is too deep to achieve satisfactory results. Local skin flaps serve as another reconstructive option for coverage of a defect of the nose. Not only are they associated with surgical ease and shorter operating time but also they match the color and texture of nasal skin. Donor sites for local flaps for facial skin defects usually provide the best option for reconstruction. Potential drawbacks, however, include additional facial scars, which may be difficult to camouflage, and the possibility of additional procedures (two stages of repair). In addition, dog-ears or a trapdoor phenomenon can result from local flaps requiring a second procedure to create a desired outcome. Microvascular free flap reconstruction requires additional training and expertise, long operative time, and substantial effort. Discussion of this type of reconstruction is beyond the scope of this article.
Free cartilage grafts
Free cartilage to reconstruct the nose after tumor removal can be harvested from the septum, concha, or rib. These cartilage grafts with their overlying perichondrium can provide valuable structural support that may have been lost after tumor removal. Structural grafting is necessary for two reasons. First, it is needed to provide rigidity to the sidewall or dorsum, thus preventing collapse and nasal obstruction. Secondly, it creates or maintains form, especially along the alar rim and tip. Septum and rib grafts are hyaline cartilage, which is strong and stiff yet pliable, and thus can be carved to provide rigid scaffolding for reconstruction.
Septum
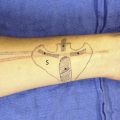
Septal cartilage is the graft of choice for reconstructive rhinoplasty surgeons. It is easily accessible during surgery without the morbidity of an additional donor site. It is a relatively straight stiff graft that is more robust than auricular cartilage so is easier to carve and shape precisely. After tumor removal, the straight septal cartilage is ideally used for the middle vault and the nasal sidewall areas. It can also be used, however, for nasal tip grafting, strut grafts, batten grafts, lateral crural grafts, spreader grafts, shield tip grafts, and buttress grafts. Thus, septal cartilage is versatile and valuable for reconstructive surgeons. The thin nature of the quadrangular plate means that stacking of septal grafts may be needed to recreate enough volume; however, the septal cartilage thickens posteriorly. Unlike many investigators, the authors have found that septal cartilage is ideal for all areas of reconstruction, including the tip and alae ( Figs. 1 and 2 ). Although it is flat, its strength and resiliency can lend great advantage to restoring various missing components of the tip.
Discussion of the technique for septoplasty harvest is beyond the scope of this article, but regardless of the approach, the amount of septal cartilage to be removed should be dictated by the amount of cartilage required for surgery. It should be remembered that least 1.5 cm of both dorsal and caudal septal cartilage struts should remain in place to adequately support the nose. If more cartilage is needed than can be safely obtained from the nasal septum, alternative sources of autologenous donor cartilage are sought.
Auricular Cartilage Grafts
Auricular cartilage is readily available and can be harvested easily with minimal cosmetic deformity. It gives good support but, despite its similar thickness compared with the upper and lower cartilages of the nose, it is softer and more pliable than septal cartilage. Like septal cartilage, auricular cartilage is versatile. It can be used as a substitute for septal cartilage when the septum has been harvested previously. Due to its more brittle nature, however, it can be more difficult to sculpt than septal cartilage. This is especially true in older patients, so extra care should be taken during harvesting and subsequent manipulation.
Conchal grafts can be used as a single layer implant or sutured together to increase girth and rigidity. Additionally, because conchal cartilage is curved and less rigid than cartilage harvested from the septum, it is most appropriately used for smaller defects or for contour improvement of the nasal tip. Both concha cavum and cymba can be used. The concha cymba can be divided lengthwise to recreate a missing lower lateral cartilage bilaterally. Structure and support is achieved better with septum or rib cartilage. It has been shown that auricular cartilage frequently does not maintain the structural integrity and rigidity to withstand the contractile forces that follow reconstruction. Coverage of a free cartilage graft requires vascularized tissue; local flaps are ideal. Regional melolabial or paramedian forehead flaps are both useful for coverage of free cartilage grafts; both require a second-stage procedure to divide their pedicles.
Rib Cartilage Grafts
Costal cartilage is an excellent structural graft for large and severe nasal defects due to its ample supply. Although it has historically been used by facial plastic and reconstructive surgeons to address structural defects secondary to congenital deformities, trauma, infection, or previous operations, it is also a valuable graft for reconstruction for malignancy. It is especially useful in patients who have had previous rhinoplasty or septoplasty or who have larger defects. Costal cartilage is strong, abundant, durable, and pliable; it offers the ability to replace or augment missing tissue with similar tissue and recreate the nasal anatomy as close to normal as possible.
Cartilage can be harvested from either the fifth, sixth, seventh, or eighth rib for nasal implantation Most rib harvests can be done through skin incisions that are less than 4 cm. The underlying musculature is separated rather than divided by dissecting longitudinal to muscle fibers. Once the rib is encountered, the perichondrium is incised and carefully elevated away from the underlying cartilage. Great care should be taken to avoid penetrating the perichondrium along the undersurface of the rib so that violation of the pleura is avoided. After harvesting sufficient cartilage, the wound is closed in a layered fashion. A drain is not necessary. A straight portion of the rib is harvested and only the central core used because the eccentric portions of the rib graft increase the chance of warping. Proper graft fixation may also reduce the risk of malposition and warping.
Graft resorption and warping are the most common complications that arise. Other disadvantages of using a rib graft include graft displacement, potential iatrogenic pneumothorax, chest wall scarring, and postoperative pain. In addition, calcification of cartilage in older patients can make carving and shaping nearly impossible.
Crushed Cartilage
Small defects after malignancy resection may require augmented cartilage grafts to achieve the cosmetic results desired. Solid carved pieces of cartilage often become noticeable with time, especially under thin nasal skin. Crushed autogenous cartilage grafts may offer a wa y to conceal small nasal dorsal and tip irregularities. Many investigators have concluded that crushed cartilage can be used to attain aesthetic goals with a fair degree of predictability. Although the viability of crushed cartilage has been questioned, Cakmak and colleagues showed that moderately crushed cartilage still shows good chondrocyte viability and proliferation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree