Reconstruction of complex full-thickness nasal defects requires the reconstitution of the mucous internal nasal lining, the cartilaginous framework, and the aesthetic contour of the cutaneous nasal covering. Goals of reconstruction include restoration of a functional nasal airway and redefinition of the contours of the nose as well as its relationship to the cheek and lip with the least amount of morbidity to the patient. This article details a multistaged approach to repairing such a defect using an ipsilateral septal mucoperichondrial flap, multiple cartilage grafts, a paramedian forehead flap, and a cheek flap in a woman who had undergone Mohs surgery.
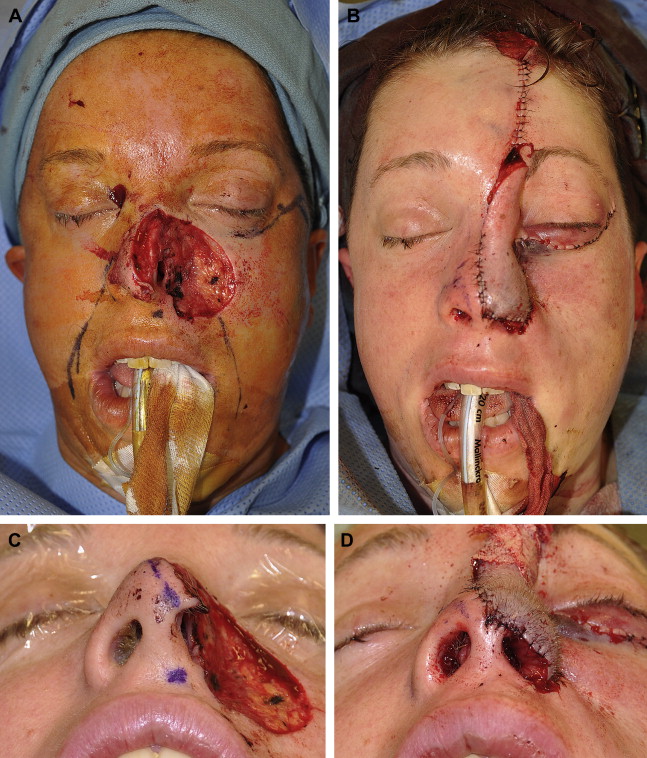
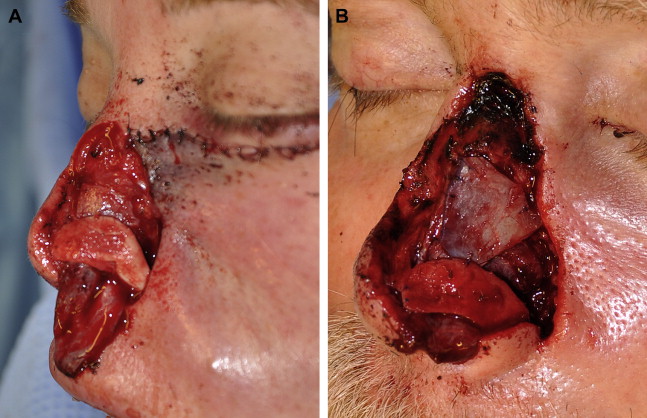
A 37-year-old-woman presented with a 4-year history of a left alar nasal lesion. The lesion tested positive for an infiltrative basal cell carcinoma. At the initial presentation, her ala was significantly retracted and she had a 4 cm ×2-cm indurated mass centered at the alar-facial sulcus that encompassed her entire left nasal ala and extended superiorly to the inferior nasal sidewall and laterally to the medial cheek. She underwent Mohs micrographic resection that resulted in a composite medial cheek and full-thickness nasal defect that included her left hemitip, dorsum, sidewall, and ala ( Fig. 1 ).
First stage: nasal and cheek reconstruction
Options for reconstruction included a staged initial reconstruction of the cheek to set a platform for nasal reconstruction followed by a multistage nasal reconstruction of the full-thickness nasal defect. The second option was to perform simultaneous reconstruction of the cheek and nasal defect. Setting the nasal platform by first reconstructing the cheek alone may increase the total number of procedures; however, it decreases the risk of the nasal platform being displaced laterally and inferiorly as the cheek flap heals and contracts. The patient had a strong desire to minimize the number of operative procedures and total time for reconstruction, thus it was decided to perform the first stage full-thickness nasal reconstruction while simultaneously reconstructing the medial cheek defect.
Cheek Defect Reconstruction
The medial cheek defect was reconstructed using a cheek flap that extended from the lateral aspect of the wound just inferior to the medial canthus into a subciliary crease that extended to the lateral orbital rim. After undermining and mobilizing the cheek flap, it was secured medially to the ascending process of the maxilla by passing a 3-0 polydioxanone suture through drilled holes because no periosteum was left after the Mohs procedure. A 5-0 polydioxanone stabilization stitch was also placed at the lateral orbital rim. Once the medial cheek defect was reconstructed, attention was directed at reconstructing the nose.
Intranasal Lining Repair
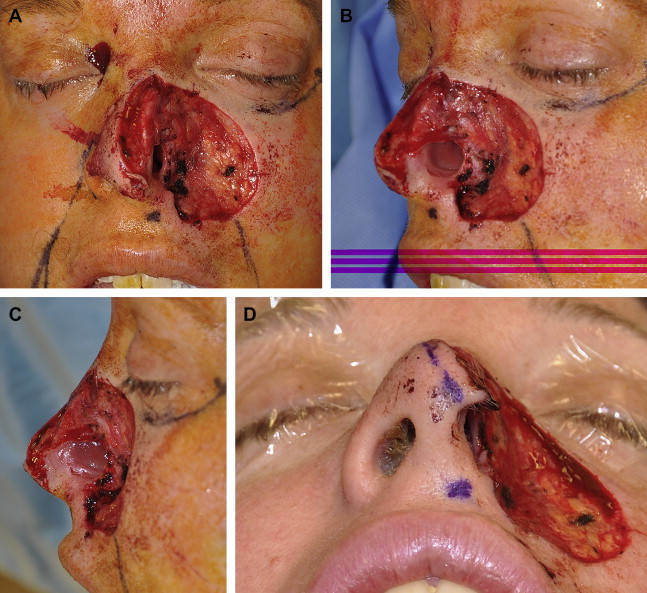
Repair of the mucosal nasal lining is essential for optimal restoration of nasal function and form. The lining flaps not only help restore nasal airflow but also provide a bed of vascularized tissue to support the integration of cartilage and bone grafts that reconstruct the shape and rigidity of the nose. The patient’s mucosal defect comprised the lower middle nasal vault, ala, and hemitip. Options for relining such a defect included the use of a bipedicled lining flap combined with a contralateral septal hinged mucoperichondrial flap, an inferior turbinate flap, or a caudally based ipsilateral septal mucoperichondrial flap. The defect size precluded the use of a bipedicled vestibular advancement flap, and a contralateral hinged flap alone would not reach the caudal border of the defect. The lateral wall defect bordered the head of the inferior turbinate, potentially compromising the vascularity of an inferior turbinate flap, thus an ipsilateral septal mucoperichondrial flap was harvested for reconstruction of the nasal lining. The caudally based flap is based on the septal branch of the superior labial artery and is best used to line the defects of the unilateral tip, ala, and lower middle vault. The flap is designed as large as possible typically ranging from 4 to 5 cm in length and 2 to 2.5 cm in width and can be narrowed to 1.3 cm at its base, the caudal septum.
After infiltration with local anesthetic containing epinephrine, 2 parallel horizontal incisions were made dorsally and along the nasal floor. The dorsal incision began just posterior to the anterior septal angle, maintaining 1 cm of mucosa for the cartilaginous dorsal strut and extending posteriorly past the bone-cartilage junction. The inferior incision began just posterior to the nasal spine, extending the same distance posteriorly as the dorsal incision, and then a vertical incision was made between the 2. A right-angled blade, such as an otologic round knife or a No. 66 Beaver blade is helpful for the vertical incision. The flap was elevated using standard septoplasty techniques ( Fig. 2 ). Once the septal flap was elevated, and before insetting the flap along the lateral nasal wall, septal cartilage was harvested, maintaining a 1-cm dorsal-caudal strut. The flap was then rotated laterally and inferiorly and inset by placing 5-0 chromic gut sutures from the superior border of the mucosal defect to the submucosal surface of the hinged flap ( Fig. 3 ).
Nasal Framework Repair
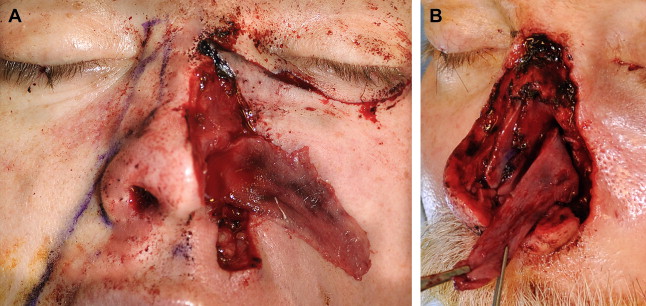
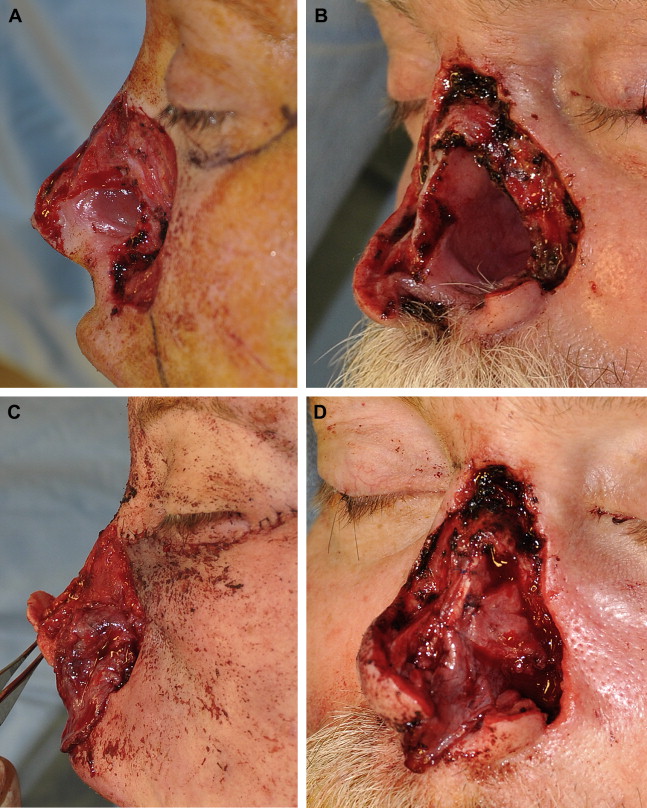
The nasal framework provides external contour to the nose and a patent nasal airway upon inspiration. After portions of the framework are removed, structural grafts are required to reconstruct the shape of the nose, to prevent collapse of the airway upon inspiration, and to prevent cephalic retraction of the alar margin upon healing. Unlike internal lining or cutaneous covering reconstruction, structural grafts of the nose are often nonanatomic, especially when repairing the nasal sidewall and ala. Grafts may span the entire subunit to prevent alar retraction as well as collapse of the middle vault and ala.
This patient had a defect of the entire cartilaginous nasal sidewall and ala (see Fig. 1 ). The cartilaginous middle nasal vault was reconstructed with a piece of septal cartilage that recreated the upper lateral cartilage, and the ala was reconstructed using a conchal cartilage graft that comprised the entire subunit. The alar conchal cartilage graft was designed to extend to the caudal nasal margin to prevent retraction of the new ala. The medial aspect of the conchal cartilage graft was secured to the remaining medial crura of the left lower lateral cartilage with a 5-0 polydioxanone suture ( Fig. 4 ). Both grafts were fixed to the underlying septal lining flap and to each other using a 5-0 polydioxanone suture. A columellar strut graft of septal cartilage was also placed between the remaining medial crura to provide additional tip support, given the resection of the majority of the left lower lateral cartilage.
Cutaneous Nasal Covering Reconstruction
The cutaneous defect encompassed almost the entire left side of the nose (see Fig. 1 ). A paramedian forehead flap was designed using a template from the contralateral intact side for re-creation of the left hemidorsum, lateral nasal sidewall, ala, and hemitip. Conventional teaching describes that if 50% of a convex nasal subunit is missing, the entire subunit should be reconstructed, but adequate cosmesis can be achieved by reconstructing only half of the tip and dorsal subunits.
The supratrochlear artery, on which the paramedian forehead flap is based, is consistently found 1.7 to 2.2 cm lateral to the midline of the glabella. This location correlates closely to the medial aspect of the eyebrow. The flap pedicle is recommended to have a width less than 1.5 cm because a narrower pedicle has less risk of strangulation. Thus, the flap pedicle with a width of 1.1 cm was based at the medial aspect of the eyebrow. A combination of the patient’s low hairline and distal nasal defect required a significant portion of the alar and hemitip subunits of the flap design to include hair-bearing skin ( Fig. 5 ). Options to minimize the amount of hair-bearing skin transposed with the flap include angling the flap laterally in an oblique manner or lengthening the inferior incision inferior to the superior orbital rim. For flaps wider than 3 cm (which was the case for this patient), obliquely angling the flap can produce a more unsightly lateral forehead scar as well as increase the risk of medial brow elevation as the forehead scar heals by secondary intention. Thus, the forehead flap was not angled for this patient.

The flap was incised and elevated in a subcutaneous plane underneath the templated portion of the flap and then transitioned into a subgaleal plane to the base of the flap. Once the flap was elevated, additional thinning of the flap was done briefly to the level of the subdermis to ensure symmetric thickness and to partially depilate the flap. In smokers, the flap is not thinned as aggressively. The flap was then transposed to the nasal defect and secured to the recipient nasal skin using a 6-0 nylon suture and a subdermal 5-0 polydioxanone suture along each lateral edge of the flap. Minimal subdermal sutures are required because the flap should not be under any tension. If the flap requires additional length, horizontal releasing cuts can be made through the frontalis muscle to the level of the subcutaneous tissue along 1-cm intervals, which can result in an additional 1.5 cm of length. Additional length can also be achieved by extending the pedicle incision inferior to the medial eyebrow and orbital rim. The distal portion of the flap was wrapped around the margin of the conchal cartilage graft and secured to the septal mucoperichondrial internal lining flap using a 5-0 chromic suture. An additional 2-mm alar marginal septal cartilage graft was placed in a pocket between the forehead and septal flaps just distal to the conchal cartilage graft to provide additional resistance to alar retraction.
The forehead donor site was closed after undermining widely from one border of the anterior temporalis muscle to the other. The muscle and galea were closed using a 3-0 polydioxanone suture followed by a 6-0 nylon suture for the skin. The superior portion of the donor site could not be closed and was left to heal by secondary intention ( Fig. 6 ). However, the anterior hairline could be reapproximated, and because the flap had been raised in a thin subcutaneous plane at the hair-bearing aspect of the flap, some hair follicles remained at the exposed donor site and regrew through the healed wound ( Fig. 7 ). This patient also had thick hair that easily hid the area of alopecia.