Chapter 40 Buttock implants
![]() For additional online content visit http://www.expertconsult.com
For additional online content visit http://www.expertconsult.com
A Gluteal Implant Augmentation
Key Points
• Ideal candidates are thin patients with an athletic build and little or no ptosis.
• Determine the patient’s expectations and evaluate the size of the proposed implant with templates.
• The day before the surgery the patient should be given an enema and begin antibiotics.
• Mark the patient in a standing position.
• Make two incisions, one for each implant, leaving 2 centimeters between them.
• Subcutaneous undermining in the sacral area is minimal and the skin and underlying tissue at the midline remain untouched.
• Subfascial undermining and flap elevation begins at the lateral border of the sacrum.
• Create both pockets before placing any implants.
• No sitting is allowed for the first month after surgery.
• If infection of the pocket is determined, treatment requires temporary removal of the implant.
• Infection of the wound is locally treated. Prophylactic antibiotic is used.
Evolution of Technique
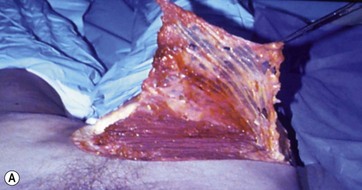
In 1973, Dr. William Cocke and G. Ricketson described the use of mammary implants for correction of lateral gluteal depressions. The implants used had Dacron patches on the underside for better fixation, although other types of breast implants were also used. This was the first description of the placement of gluteal implants in the subcutaneous plane. However, the use of mammary implants in a subcutaneous plane produced less than optimal esthetic results (Fig. 40.1). The implants are noticeable through the skin and do not give a natural appearance.
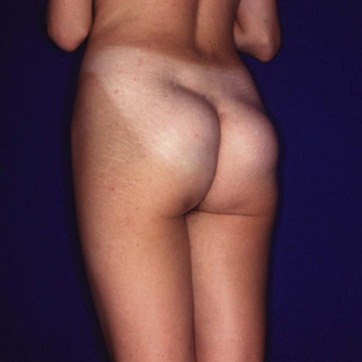
FIG. 40.1 Use of mammary implant in a subcutaneous plane produced less than optimal esthetic results.
Subcutaneous Plane
First attempts at gluteal augmentation placed implants in the subcutaneous space (Fig. 40.2); breast implants were used until the first implant designed by González-Ulloa specifically for gluteal augmentation was released by Dow Corning. However, this subcutaneous space had numerous anatomic restrictions, making it unsuitable for this operation. Results were unnatural, and the visibility of the implant restricts the usefulness of this space for gluteal augmentation (Fig. 40.3A, B, C).
Correction of these cases implies having to change the dissection plane to either intramuscular or subfascial and closing the subcutaneous space permanently. In Fig. 40.4A, B, and C the correction of the patient shown in Fig. 40.3 has been performed, placing a polyurethane covered gluteal implant in a subfascial plane (photos were taken 6 weeks postoperatively).
Submuscular Plane
In 1984, Dr. Robles from Argentina described a new technique for gluteal augmentation that used a submuscular approach. This approach preserved the aponeurotic system that holds gluteal skin in position; however, it introduced a new anatomic problem with the potential risk of injury to the sciatic nerve. This nerve emerges from the submuscular space, at the level of the proximal lower third of the gluteal region and at the inferior border of the piriform muscle. To avoid injury to this nerve, an implant could not be placed below this level (Fig. 40.5). Furthermore, implants had to be small in diameter and could not be placed close to the infragluteal fold.
Intramuscular Plane
Another anatomic space described for gluteal implants was the intramuscular space (Fig. 40.6), which was developed by disrupting the gluteal muscle fibers. The goal was to leave a 3 to 4 mm thickness of gluteus maximus muscle attached to the aponeurosis. Ideally, this could help to minimize risk to the sciatic nerve, but disruption and avulsion of the muscle fibers produced a high incidence of seroma. It was also very difficult to estimate the quantity of muscle on top, and the possibility of injuring the sciatic nerve was not totally eliminated because undermining was done blindly with no anatomic landmarks to guide the surgeon.
Additionally, skin markings for this operation were done with the patient in a sitting position; thus the inferior part of the gluteal region would remain empty. Although the threat of injury to the sciatic nerve was remote, the esthetic result, similar to that of the submuscular approach, was suboptimal. The inferior border of the implant was high, and the lower part of the gluteal region was empty and loose with the appearance of a double contour (Fig. 40.7A, B, C). Furthermore, the operation was painful, with a difficult postoperative period, because the patient had to maintain a vertical position for several days.
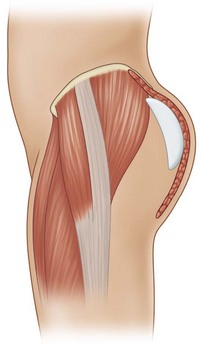
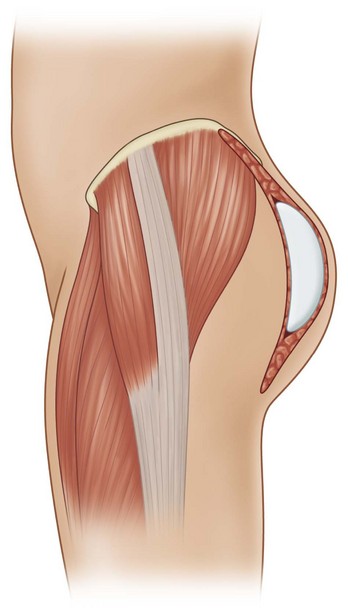
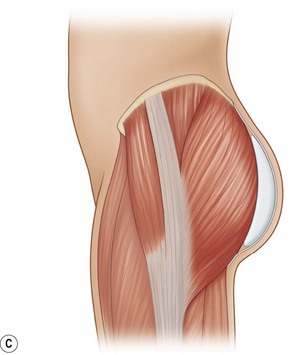
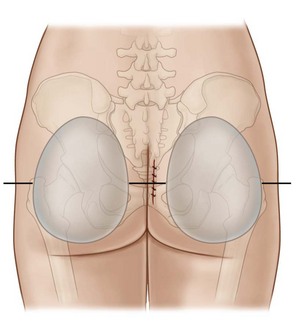
Subfascial (Subaponeurotic) Plane
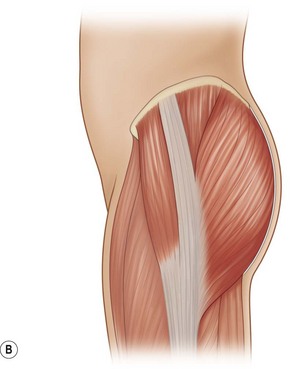
The gluteal aponeurosis is very strong at its origin and insertion. This fascia covers the gluteus maximus muscle (Fig. 40.8A, B), the larger and more superficial regional muscle responsible for projection of the gluteal area, and the anterior two thirds of the gluteus medius muscle, which shows on the upper third of the gluteal region. The gluteal aponeurosis insertions are on the posterior iliac bone, the sacral bone, and the coccyx bone, and on the lateral limit inserts on the greater trochanter and extends to the iliotibial line.
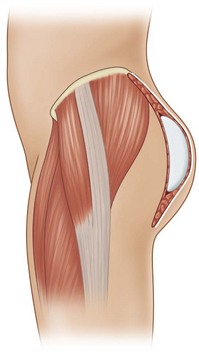
This large aponeurosis covers the entire gluteal region and at the same time molds the gluteal augmentation; it is stronger at the insertion sites and softer in the middle, helping to achieve a natural result (Fig. 40.9A, B).
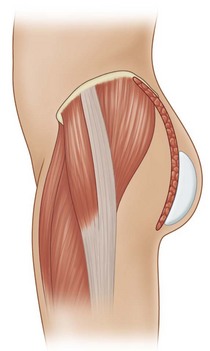
The aponeurosis expansions are distributed in a transverse direction, along the axis of the muscle fibers throughout the gluteal region. Because they originate on the deep part of the gluteal aponeurosis, the attaching fibers convert the superficial surface of the gluteus maximus into a uniform space shaped like the muscle. The aponeurotic expansions to the skin are preserved, and the subaponeurotic space allows proper positioning of an implant without risking injury to the deep neurovascular structures (Fig. 40.10A, B).
Indications
• Young patients with an athletic build with little or no ptosis.
• Morbidly obese patients are not candidates for this surgery unless they lose weight, after which the laxity of tissues converts them into good candidates if they undergo excisional procedures to correct the back and gluteal regions.
• Those patients who lack projection of the gluteal region and desire to improve the shape of the gluteus.
• Unilateral implant placement is occasionally needed to correct an asymmetry or reconstruct subcutaneous tissue lost through infection trauma, or neurological problems that result in muscle atrophy.
• Subfascial augmentation with anatomically shaped implants can correct minor degrees of gluteal ptosis. But, as with breast surgery, implants are not the solution to severe ptosis.
• The implants used today minimize the risk of displacement, having a textured surface, or a polyurethane foam cover that minimizes the occurrence of capsular contracture.
• Patients must be informed preoperatively about restrictions for sitting in the postoperative period, in which they will be limited to sitting only when going to the bathroom for the first month postop. If these instructions are not followed, the chance of wound dehiscence and other complications is elevated. If you predict that the patient will not comply with the instructions, you should not proceed with the surgery because serious complications may occur.
Why Is the Subfascial Plane Recommended?
The subfascial plane is the most superficial anatomical space that can hold an implant capable of molding and shaping the buttocks using the gluteus maximus muscle as a platform for the implant. This space is limited inferiorly by the infragluteal fold where the gluteal aponeurosis attaches to the posterior thigh fascia (Fig. 40.11). In addition, the likelihood of implant displacement is minimal because the subfascial space is closed.
The gluteal aponeurosis sends expansions to the skin, which insert onto the deep portion of the dermis; these expansions work as a system to maintain the skin and subcutaneous tissues adherent to the gluteal region in the same way the skin of the palm of the hand is attached to the deep tissues. These aponeurotic expansions are distributed transversely. They originate on the deep part of the gluteal aponeurosis and cover the superficial part of the gluteus maximus muscle in a muscle group divided by these expansions. To maintain this system intact, subcutaneous undermining should be avoided. We prefer a subaponeurotic space that can be carefully undermined on top of the gluteus maximus muscle. This undermining allows perfect positioning for the implants without possible injuries to the deep neurovascular structures while preserving the aponeurotic expansions to the skin. After the implants are placed, this space is anatomically contoured by the gluteal aponeurosis, and it is limited inferiorly by the infragluteal crease where the gluteal fascia is attached to the posterior thigh fascia (Fig. 40.11B, C).
Implant Decision
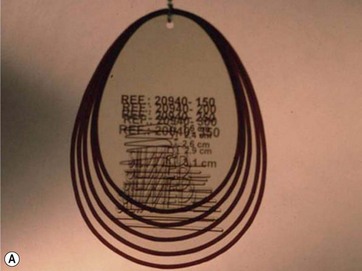
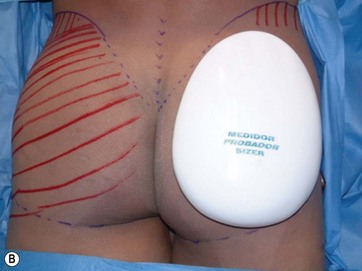
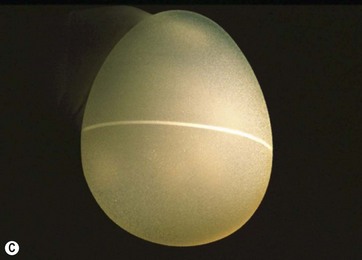
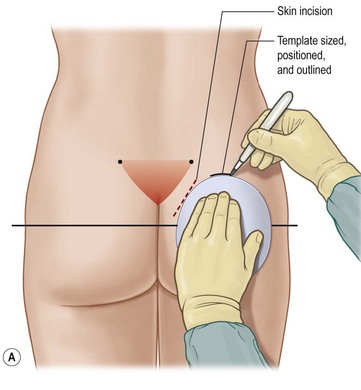
This procedure employs small anatomic implants for gluteal augmentation, as well as bigger implants for larger patients who want a better contour of the gluteal region. Gluteal contour is gained by insetting anatomic implants on top of the gluteal maximus muscle and under the gluteal aponeurosis. The anatomic decision making system designed for this operation consists of templates (Fig. 40.12A) for the preoperative skin markings, sizers for transoperative measurement (Fig. 40.12B), and gel-filled implants (Fig. 40.12C). Further explanation of decision making for individualized implant selection will be elaborated in the technique portion of this chapter.
FIG 40.2D, E Appears ![]() ONLINE ONLY
ONLINE ONLY
Implant Characteristics
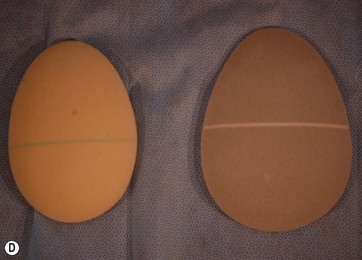
New designs of gluteal implants have been launched onto the market recently. The design recommended can vary depending on the desires of the patient and their anatomy but the most important factor to keep in mind when deciding on a type of implant is making sure that the transverse length of the buttocks is not increased, that is why a narrow base with adequate projection is desired (Fig. 40.12D, E; De la Peña Design implants on the left with a polyurethane cover).
Preoperative Preparation
Markings
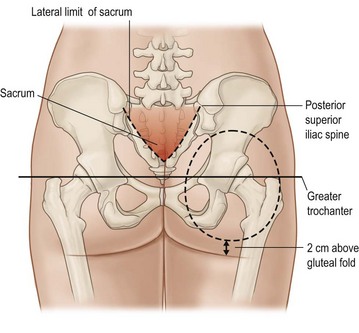
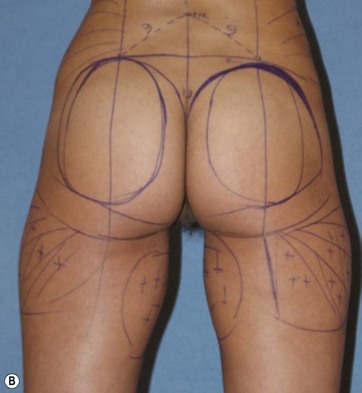
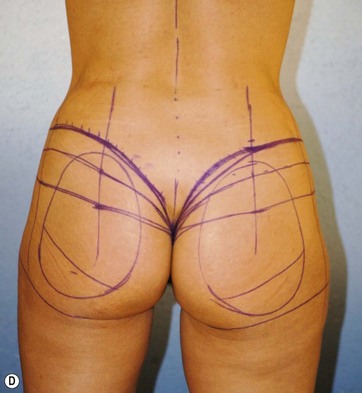
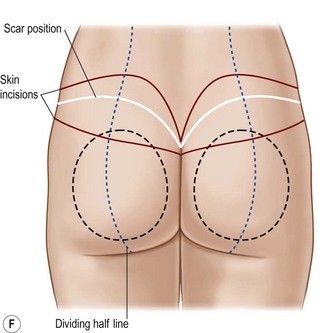
With the patient in the upright position, skin markings are made using a custom-designed template. The template must fit perfectly into the gluteal region leaving 2 cm above the infragluteal sulcus and 2 cm lateral to the external rim of the sacral bone (Fig. 40.14). The sacral triangle must be preserved; it is an esthetic landmark of this region. The implant should never be placed on top of the sacral bone.
Laterally the template will extend to the external border of the gluteal region, leaving at least 2 cm from the external line (Fig. 40.16A); this is the line that continues up from the iliotibial line of the thigh. Liposculpture lines are drawn at the same time when indicated (Fig. 40.15B).
1. Skin quality of the lower back, gluteal region and flanks.
2. Length or cephalocaudal distance of the buttocks.
Proposed Classification for Gluteal Ptosis (Fig. 40.15C)
No ptosis: The infragluteal fold entails only the middle third of the posterior aspect of the transition area from the buttocks to the leg.
Grade I: Evident laxity of the skin with the infragluteal fold extending more than one third of the posterior aspect of the transition area from the buttocks to the leg.
Grade II: Lax gluteal tissue at the level of the infragluteal fold.
Skin markings in patients with ptosis is different (Fig. 40.15D–F) because there is an excision of skin in the upper part of the buttock and lower part of the back from where the surgery is carried out, but the subfascial plane is created in the same manner when compared with gluteal augmentation only.1–4
Liposculpting and Gluteal Implants
Anesthesia
After the incisions are made and the subfascial space has been reached, tumescent infiltration with a modified Klein solution is performed (Fig. 40.16). This has two advantages: It produces hydrodissection of the subfascial plane, making it easier to create the pocket for the implant and produces vasoconstriction with less bleeding, giving a better visualization of the anatomical structures.
Surgical Procedure
The procedure is outlined in Box 40.1.
Box 40.1
The Basic Surgical Technique
1. Skin approach in the intergluteal fold.
2. Subcutaneous undermining over the sacral region.
3. Subfascial dissection where the template area is marked.
4. Placement of the implants so that they fit loosely in the pocket.
5. Closure of the different spaces with care to ensure that the subfascial space is waterproof.
6. Approximating of the subcutaneous dissection over the sacral bone.
7. Closing the incision so that the intergluteal fold is recreated.
Surgical Technique
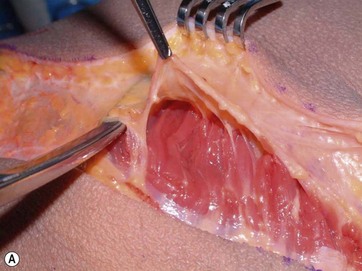
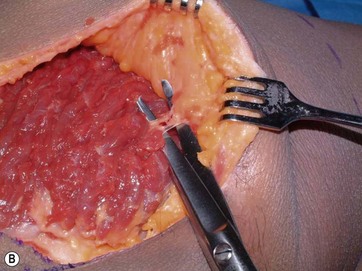
The surgical incision begins at a point 3 cm above the anus corresponding to the level of the coccyx and extends cephalad approximately 6 cm. The incision then proceeds laterally to the presacral fascia on the subcutaneous tissue until the external rim of the sacral bone is reached. At this time an incision is made parallel to the external rim of the sacral bone on the gluteal aponeurosis and reaching the subfascial space (Fig. 40.17A). Care is taken not to cut any of the muscle fibers. Infiltration of Klein’s solution is done under the aponeurosis; this facilitates identification of the avascular plane under the fascia. The multiple septae from the aponeurotic expansions are identified and infiltration is done between this network (Fig. 40.17B). Because these are aponeurotic expansions, they are not easily disrupted so they all need to be cut to ensure hemostasis (Fig. 40.17C). The goal is to raise a fasciocutaneous flap in the gluteal region.
FIG 40.17A Appears ![]() ONLINE ONLY
ONLINE ONLY
Sharp dissection continues; lighted retractors and long instruments for retraction, cutting, and coagulation are essential to divide all aponeurotic expansions over the muscle. Bleeding is minimal if undermining proceeds carefully, with simultaneous coagulation with dissection. Perforator vessels from the superior and inferior gluteal arteries are identified and legated (Fig. 40.17C). To facilitate undermining, it is advisable to maintain the dissection from medial to lateral and from cephalic to caudal, maintaining a wide field of exposure extending from the initial subfascial undermining (Fig. 40.18A). It is also important to remember to restrict the undermining to the level of the skin marking, thus preventing it from extending beyond the infragluteal crease.
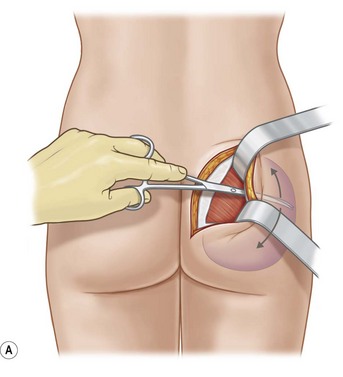
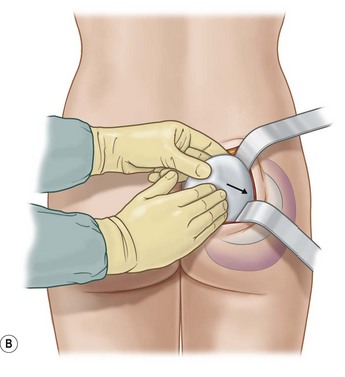
FIG. 40.18 It is advisable to maintain the implant in saline solution with antibiotic until the end of surgery.
Once dissection is completed, we use implant sizers to confirm the size of the implants to be used and to determine if any further dissection is needed. These sizers are developed as part of the anatomic system for gluteal augmentation; they are white smooth-surfaced gel-filled implants, each with the corresponding size mark and with the “sizer legend” on top. These are not the definitive implants; however, they are handled with the same no-touch technique used for the final implants. It is advisable to maintain the implant in saline solution with antibiotic until the end of surgery (Fig. 40.18B).
Once the final implants are selected, closed suction drains are inserted to help maintain the adhesion of soft tissues to the implant. The selected implants are placed. These implants have a transverse line on their equator so that they can be seen through the incision and to ensure perfect placement and alignment (Fig. 40.19).
The implant must fit loosely in the pocket, and closure of the aponeurosis must be without tension. Tissues are rearranged to comfortably drape over the implant. It is advisable to dissect both pockets before inserting any implant so that the augmented gluteus does not interfere with the dissection of the contralateral pocket (Fig. 40.20A, B).
Optimizing Outcomes
Box 40.2
Optimizing Outcomes
For optimal results apply the following steps:
• Skin approach in the intergluteal fold.
• Subcutaneous undermining over the sacral region.
• Subfascial dissection where the template area is marked.
• Placement of the implants so that they fit loosely in the pocket.
• Closure of the different spaces with care to ensure that the subfascial space is waterproof.
• Approximating of the subcutaneous dissection over the sacral bone.
• Closing the incision so that the intergluteal fold is recreated.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree