Chapter 41 Buttock contouring with liposuction and fat injection
![]() For additional online content visit http://www.expertconsult.com
For additional online content visit http://www.expertconsult.com
Preoperative Preparation
Markings of Esthetic Units
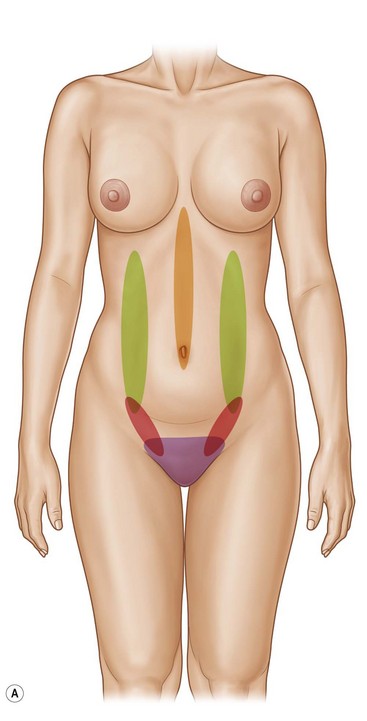
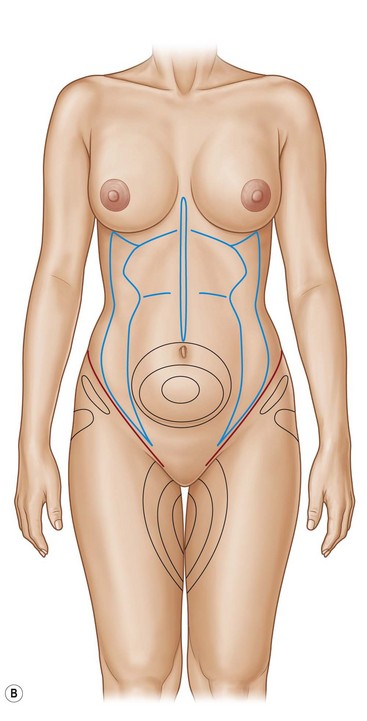
The abdomen is defined by three major muscle groups that can be appreciated on the surface anatomy; the rectus abdominus, the external oblique and the transversalis muscle (Fig. 41.1). The union between these muscles is called the raphe and it is these raphes that need to be accentuated during contouring in order to highlight and define the underlying anatomy.
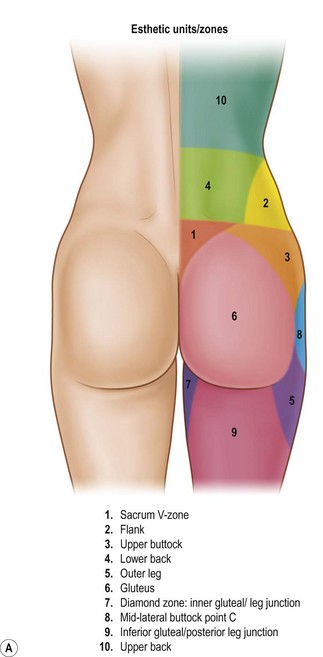
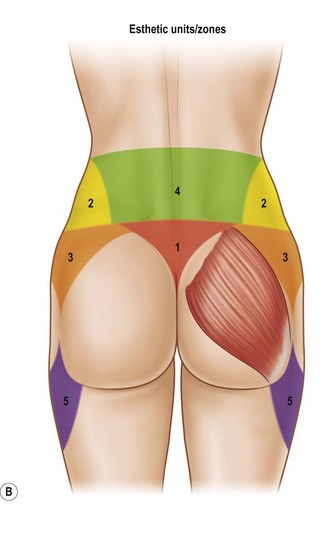
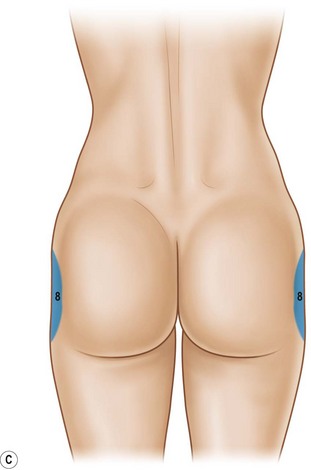
When it comes to the posterior zones, there are 10 esthetic units found to the posterior region, with 6 that truly define the buttock frame/ shape (zones 1–5 and zone 8)1 (see Fig. 41.2A). The midlateral buttock (Zone 8) becomes of particular interest since it is the only zone out of the six that may require fat transfers to smooth the contour. This zone has no muscle, therefore fat transfers are into the less vascularized subcutaneous tissues requiring more care and precision with the fat grafting technique.
Three landmarks areas are identified in the buttock; the first is the posterior superior Iliac spine (dimples in the parasacral areas); this represents the height of the gluteal muscle I am trying to achieve. With these points marked it is easy to identify and mark the second landmark – the “V” zone, also known as zone 1. This is the space identified by the most superior point of the intergluteal fold and both posterior iliac spine dimples; the connection of these points creates an equilateral triangle. When this zone is suctioned it adds tremendous contour to the esthetic of the buttock. Third, I identify any depression in the midlateral buttock (zone 8) (see Fig. 41.2C). Sometimes these depressions extend all the way to the anterior leg; therefore, care is taken to mark the lateral extent of the deficiency, and finally any dimples or irregularities are marked. Zone 3 is evaluated and I try to mentally quantify how much fat I want to remove using the very sophisticated categories of very little, none, or a lot. Photos are taken of the markings since these become extremely helpful because often these marks are erased during surgery.
Preparation in OR
The patient is prepped circumferentially while in the standing position using room temperature Hibiclens solution (Fig. 41.3). A sterile sheet is placed on the OR table on top of a water-based warming pad (HTP-1500 Heat Therapy Pump and Pad, Adroit Medical System). The best setting is 41.6 °C (107 °F).
FIG 41.3 Appears ![]() ONLINE ONLY
ONLINE ONLY
It is during this time that the fat collection canister is prepared since the fat needs to be collected during the suction process. There are a number of collection systems for obtaining fat cells (Fig. 41.4), all of which have pros and cons.
FIG 41.4 Appears ![]() ONLINE ONLY
ONLINE ONLY
These are very large Lukens trap devices that collect the aspirate by connecting one suction tube from the patient to the bottle and another tube that goes from the bottle to the suction machine (Fig. 41.5). Once this is all in place the procedure can begin.
Suctioning Details
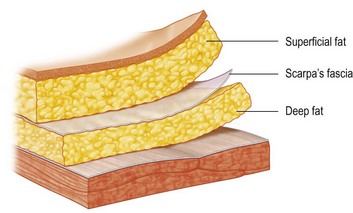
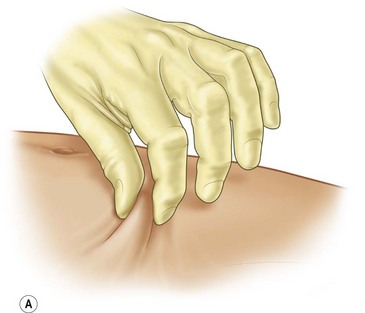
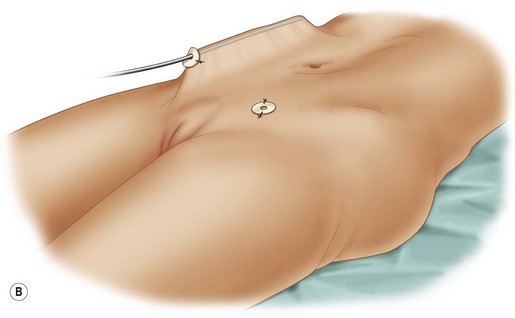
The technique involves a visualization exercise whereby the surgeon visualizes the deep and superficial layers in the mind. Suctioning will then proceed in a layered and anatomic sequence, but throughout the process the physician is visualizing the position of the cannula in the respective layer (Fig. 41.6).
• Vaser ultrasound machine at a power of 80% pulsed with a 3-ring probe to soften the fat, starting at approximately 1–2 cm depth and below.
• Power-assisted specialized Mendieta cannula (5 mm) with the suction turned off (as recommended by Dr. Simeon Wall, Jr) for pre- and post-tunneling.
In cases of mild to no dermolipographing, technology is not needed since the skin molds extremely nicely and irregularities are extremely rare (Fig. 41.7A, B). I leave about 1 cm of fat under the dermis.
FIG 41.7B Appears ![]() ONLINE ONLY
ONLINE ONLY
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree