Fig. 46.1
Mixing stem cells and adipose tissue
This “biological filler” could be injected to correct both deep and extremely superficial lower-volume areas in a more natural way and without risks. The results of the operations performed appear to remain stable over time with the use of stem cells due to the standardized grain size of the fat mechanically treated through a small kitchen whisk when it was first treated. This technique of adipofilling is the object of research to increase the survival of fat grafts with the latest equipment for the handling and processing of adipose tissue, which is aimed at improving the engraftment of the cells injected and cell selection methods, self-duplication, and survival improvement, creating an alternative to what we had until today, which was the lipotransfer and buttock prostheses.
The techniques aimed at filling localized areas of the body with adipose tissue are commonly called lipofilling or, by the author, called buttock biomolding with autologous adipose stem cells. In recent years, these techniques have used tissue removed during liposuction and have been put into practice in order to offset the reduction or sagging of the integument and in plastic surgery as a filling in certain facial or body areas to increase their volume after traumatic loss of primary or secondary tissue. Secondary tissue loss is usually caused by protease inhibitors of the AIDS treatments. Recent advances in stem cell research have revealed that adipose tissue contains a large number of stem cells, which leads to considerable implications in the practice of medicine as a good and safe alternative for the patient and the doctor who applies it, obtaining greater degree of satisfaction and a more durable, sustained effect through time.
46.2 History (Fig. 46.2)

Fig. 46.2
Friends and colleagues at the 54th World Congress, Argentina, 2012. Left to right: Giorgio Fischer, Roberto Blum, Julio Ferreira, Angelo Rebelo, Pierre Fournier, Melvin Shiffman, and Arturo Grau
Adipose tissue has been used as a filler since the early twentieth century, but the results obtained with its use have always been disappointing since the grafted material is usually reabsorbed. In 1987, Bircoll [1] introduced the use of adipose tissue as material for breast augmentation, but he was widely criticized for the bad experiences and complications for steatonecrosis. It was for this reason that a panel made up by experts from the American Society for Plastic and Reconstructive Surgery issued a statement discouraging its use.
Coleman [2] standardized an atraumatic procedure that allows the achievement of good and reproducible results with the use of adipose tissue grafts, which is basically what the author has done today with better technology for processing and obtaining adipose tissue, especially stem cells. It consists of an atraumatic collection of fat (with 20 cm long blunt cannulas with a 2 mm diameter hole and 60 mL Toomey syringes) with the inclusion of what was said by Fournier, one of the fathers of liposuction, adding 1 mL of saline solution to make the negative pressure of the extraction less traumatic and obtain more adipocyte without damage. Additionally, Shiffman told us that the extraction should be done gently. The author advises that the extraction of fat should not be performed with an ultrasonic or liposuction laser machine that produces further damage to the adipocytes. It must be done manually.
One of the first investigations carried out by colleagues suggests centrifugation at 1,286 g (3,000 rpm with the Coleman centrifuge) for 3 min to separate the adipose cells from blood components and disrupted cells and transfer the tissue where the graft will be implanted using blunt cannulas of about 2–3 mm in multiple passes, using 1 mL in each pass. The importance of depositing micrografts had been highlighted by Bircoll [3], and for Coleman, it is the most important part of the procedure. After Coleman’s work, the author started working on that fat with the patient’s autologous stem cells in order to ensure that the implant stays longer and survives and to make it more durable.
46.3 Procedure
Tissue lobes are not as versatile as an injectable commercial filling. Graft lobular structure greatly hinders obtaining a uniform surface distribution, and it must be done with a special cannula, appropriate technique, and suitable material; in surgery, the most important thing is that the patient has to have fat, especially in the periumbilical region where the stem cells will be extracted. Furthermore, the survival of the injected lobular adipose tissue is not reproducible, since it can be affected by several factors: age, aspiration technique, vascularization of the implant area, tissue preparation, the size of adipocytes, the characteristics of the area where the tissue was removed from, metabolic diseases, habits like smoking, or drug treatments.
A thorough history and physical examination must be done, including an ultrasound of the area to be treated and MRI if possible. However, the most obvious cause of variability is still, in our view, the size of the lobes injected. The amount that should be used, at therapeutic doses, is 250 mL up to 350 mL in the case of the buttocks. Heavy fat should not be injected in that amount as is commonly done since with stem cells, the survival of adipocytes is the most important thing as the adipose tissue-derived stem cells will self-renew. In fact, it is well known that the smaller the volume to be filled, the faster and more secure the graft adherence and better if it associated with stem cells. In a large lobe of adipose tissue, cells in the central part tend to necrose, resorb, or calcify when done by the traditional method not associated with stem cells, which greatly limits the use of lipofilling in interventions for buttock augmentation because of the low survival level of the fat alone without associating it to stem cells.
The risk of visible and palpable abnormalities caused by superficial injections or injections of big amounts has been widely documented. What is advisable in the technique for buttock biomolding with stem cells is to use a 22 cm cannula with blunt tip of one single hole above the gluteus maximus muscle. The aforementioned effects appear to be caused by the difficulty of nurturing grafted lobes due to their excessive size. When they are greater than 20 mL extractions, owed to the negative pressure exerted by the operator, there is more damage to the stem cells and thus to adipocyte. In an attempt to circumvent these difficulties, the adipose tissue is removed through a small cannula, and small amounts are grafted in many tunnels created with the aid of a micro-tube in the case of breast or facial region. This involves making repetitive movements of the syringe, unlike the gluteus.
However, this maneuver is quite traumatic when not done with special cannulas in the proper area. To overcome these drawbacks and to ensure that the filling with adipose tissue is more versatile and less traumatic, the author developed a simple and inexpensive intervention that can dissociate the lobes of adipose tissue extracted from a liposuction or adipose tissue fragments from an abdominoplasty. The resulting cells and connective tissue may be injected as a filler using a traumatic blunt cannula to enrich stem cells, processing, centrifuging, separating the stem cells, and activating it with special laser.
The first and most important step is the preparation of the patient, with medical evaluation, blood tests, cardiac assessment as when performing liposuction, previous photographs, and the development of special millimetric panels to see the procedure before and after. It is performed in the operating room, and controls with thermography are performed every month the patient visits. Ultrasound is performed to indicate the percentage of fat in the area and magnetic resonance imaging to see if the autologous stem cells continue there with the fat and if there has not been reabsorption and to check the permanence of the results.
Liposuction is performed manually (Fig. 46.3) with Klein’s formulation of 500 mL of saline solution and 20 mL of Xylocaine with epinephrine and bicarbonate in a blister, and the hydrotomy with Klein’s solution is allowed about 15 min for vasodilation and vasoconstriction so that the manual removal of fat is purer and cleaner. Fat is removed at the level above or below the umbilical region, where it has been discovered that there is a greater number of stem cells, out of which 100 mL is extracted to perform the process, which lasts 4 h (Fig. 46.4).



Fig. 46.3
Manual extraction of adipose tissue by Dr. Blum

Fig. 46.4
Fat removed from the patient
Enzymatic means (Fig. 46.5) and centrifugation of the lipoaspirate release a heterogeneous population of cells called stromal vascular fraction (SVF), separating the fat, oil, and stem cells found at the bottom of the tube. This vascular fraction may be used directly mixed with the fat applied in this case in the gluteus (Fig. 46.6). Both ASC and SVF are performed in the operating room by trained doctors and proper equipment. These products are divided into those that are minimally manipulated (e.g., collection and use of SVF) and those that are more than minimally manipulated (including cell expansion of the ASC).


Fig. 46.5
Added enzymatic means for separation and obtaining stem cells
Fig. 46.6
Stromal vascular fraction
The entire procedure should be performed in line with the good hygiene practices of each country and the clinic must also be authorized to perform the procedure; as it is with outpatient facilities and independent facilities so that there is no problem worldwide (Fig. 46.7).
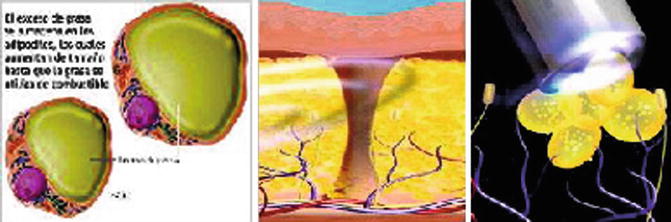
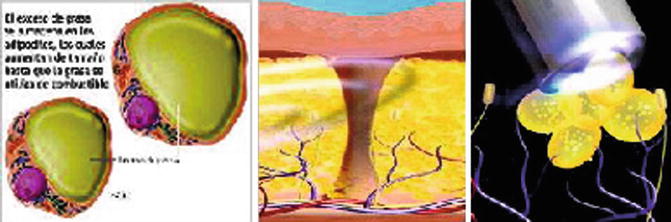
Fig. 46.7
Have healthy tissue and healthy individual to the process of stem cell autologous fat
The SVF falls into the category of minimally manipulated products that can be processed in the operating room. This processing can be manual or by designed machines. These devices can provide SVF within 1–2 h. The main problem is the high cost.
46.4 Assessing the Amount of Material to Be Grafted
As for traditional lipofilling, the donor areas and the areas of the face and/or body to be enriched with adipose cells and connective tissue must be marked. The amount of material needed to achieve the desired effect must also be assessed. In volume increase interventions, the total volume of adipose lobes extracted must be three times bigger than that required for surgical repair cases. In the case of buttocks, the therapeutic dose ranges from 250 to 350 mL of fat, and stem cells would be about 10 mL to apply each time with 5 mL on each side.
46.5 Anesthesia and Aspiration of Autologous Adipose Tissue-Derived Stem Cells (Vascular Stromal)
Anesthesia is administered using a modified Klein’s solution (physiological solution is replaced by Ringer’s lactate solution) because its pH level is more neutral than lactate. Lobules of adipose tissue are removed from the donor region by using a 60 mL syringe and a 2 mm long cannula with a single hole. The number of syringes depends on the amount to be injected. Avoid the use of larger-gauge cannulas, as the tissue aspirated is more likely to get damaged. Ultrasound or laser equipment is not used for the aspiration techniques, at least to extract stem cells. This certainty is based on geometrical considerations. The use of smaller-diameter cannulas implies that a smaller amount of aspirated material will be in direct contact with the walls of the cannula. It is therefore logical that a lower amount of this material will be subjected to potential damage due to friction against the walls. Once extracted, the lobules of adipose tissue are washed with Ringer’s lactate solution in a 25 mL sterile glass container or separately using a single syringe in a destruction process. The washing solution is extracted from the container through a cannula and will be changed repeatedly until it becomes colorless. This is what we commonly call wash where the lobules are cleaned. The washing removes residual blood and lidocaine, which potently inhibits glucose transport in adipocytes and their growth. Adipose tissue can also be obtained from the skin and excess fat for a tummy tuck, but the process is more complicated.
46.6 Transformation of Aspirated Adipose Tissue in Cells and Connective Components
The prescribed amount (minimum 250 mL) is obtained through liposuction. Sixty milliliter of extracted autologous adipose tissue-derived stem cells is the amount, depending on the area to be treated, needed, and after washing it, the resulting material (up to 100 mL) is poured into a glass container. Syringes are prepared with 25–30 mL of lactated Ringer’s solution. The procedure used to obtain adipose tissue cells consists of four or five steps performed with normal mixing with a cover of two syringes: one with 60 mL of adipose tissue and an empty one of 60 mL (Fig. 46.8).


Fig. 46.8
Washing and processing adipose tissue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








