Breast Reduction
Dennis C. Hammond M.D.
Michael Loffredo M.D.
Grand Rapids, Mich.
From Partners in Plastic Surgery.
Received for publication December 14, 2010; accepted June 29, 2011.
Copyright ©2012 by the American Society of Plastic Surgeons
DOI: 10.1097/PRS.0b013e31824a2efc
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Video content is available for this article. The videos can be found under the “Related Videos” section of the full-text article, or, for Ovid users, using the URL citations printed in the article.
Learning Objectives: After studying this article, the participant should be able to: 1. Understand the preoperative considerations that must be weighed to appropriately assess operative risk of breast reduction. 2. Have a full understanding of the basic techniques that are available to treat the patient with macromastia. 3. Identify which patients are best suited to a particular technique. 4. Identify common complications associated with breast reduction and understand how to treat them.
Summary: Breast reduction remains a basic plastic surgery procedure designed to alleviate upper torso complaints resulting from macromastia. Historically, the inverted-T inferior pedicle procedure was the dominant technique for the treatment of macromastia for 40 years. The past two decades have seen a reexamination of breast reduction technique in an attempt to improve on the results and minimize complications. As a result, a new genre of procedures based on different pedicles and short-scar skin management techniques has been introduced. With these new procedures, the plastic surgeon now has a variety of different techniques that can be offered for reducing the hypertrophic breast. Strategically applying the concepts inherent in these procedures to the correct patient can provide outstanding results with few complications. In this article, the concepts and results of these various procedures are discussed to give the reader a basic understanding of the options available for breast reduction. (Plast. Reconstr. Surg. 129: 829e, 2012.)
Preoperative Assessment
History
For any patient presenting for breast reduction, it must be remembered that a significant number of women will develop breast cancer in their lifetimes. For this reason, one of the most important preoperative issues to be clarified relates to the malignant potential of the breast. Although uncommon, occult breast cancer in the reduction specimen is occasionally detected.1,2 For this reason, a breast history must be obtained, with special emphasis placed on the results of any previous open or percutaneous biopsies, whether any masses have been or are currently present, and when the last mammogram was obtained. A practical rule of thumb regarding mammographic clearance of the breast would involve requiring such clearance for any patient older than 30 years, and lowering this threshold to 25 if there is a family history of breast cancer in any first-degree relative. For patients younger than 25 years, mammographic clearance would likely have such a low yield that its routine use would only rarely affect surgical planning regarding breast reduction. Other important information relates to the reproductive history of the patient and whether
she was able to successfully breast-feed. If not, her desire to breast-feed in the future must be assessed, as breast reduction surgery can impact on this very personal choice.3–5 Also, what effect pregnancy or weight gain had on breast size should be noted, as this can be a predictor of how the patient’s breast may change over time after the procedure if she should lose weight. This is a common concern of many patients, as they feel their breasts are a hindrance to properly exercising, and many plan to lose weight after the procedure. Basic information regarding general health status and medications can identify the need for preoperative physiologic optimization with the help of the patient’s primary care provider. Perhaps most importantly, whether or not the patient is a current or previous smoker must be documented. A smoking history will double the risk for developing a postoperative complication, and strategies designed to reduce this risk may be implemented, including cessation of smoking and alteration of technique, with perhaps a less aggressive dissection being performed.6 Also, the presence of common symptoms related to strain on the upper torso attributable to the weight of the breasts must be documented. These symptoms can include headaches, neck pain, back pain, submammary intertrigo (particularly during the warmer months), painful bra strap marks with grooving and possible associated ulnar paresthesias caused by pressure on the brachial plexus, breast pain, difficulty wearing clothing that fits proportionately, and emotional sequelae (particularly in younger girls). This latter issue is important to identify in an adolescent patient, as peer pressure or even ridicule related to breast size can hinder social development at this very important time in her life. For this reason alone, breast reduction surgery can be justified in affected patients. Finally, the patient should provide some guidance as to what size breast she was hoping to have after the procedure. Inappropriate expectations are best dealt with before surgery, as dealing with them postoperatively can be decidedly unsatisfying and unsuccessful.
she was able to successfully breast-feed. If not, her desire to breast-feed in the future must be assessed, as breast reduction surgery can impact on this very personal choice.3–5 Also, what effect pregnancy or weight gain had on breast size should be noted, as this can be a predictor of how the patient’s breast may change over time after the procedure if she should lose weight. This is a common concern of many patients, as they feel their breasts are a hindrance to properly exercising, and many plan to lose weight after the procedure. Basic information regarding general health status and medications can identify the need for preoperative physiologic optimization with the help of the patient’s primary care provider. Perhaps most importantly, whether or not the patient is a current or previous smoker must be documented. A smoking history will double the risk for developing a postoperative complication, and strategies designed to reduce this risk may be implemented, including cessation of smoking and alteration of technique, with perhaps a less aggressive dissection being performed.6 Also, the presence of common symptoms related to strain on the upper torso attributable to the weight of the breasts must be documented. These symptoms can include headaches, neck pain, back pain, submammary intertrigo (particularly during the warmer months), painful bra strap marks with grooving and possible associated ulnar paresthesias caused by pressure on the brachial plexus, breast pain, difficulty wearing clothing that fits proportionately, and emotional sequelae (particularly in younger girls). This latter issue is important to identify in an adolescent patient, as peer pressure or even ridicule related to breast size can hinder social development at this very important time in her life. For this reason alone, breast reduction surgery can be justified in affected patients. Finally, the patient should provide some guidance as to what size breast she was hoping to have after the procedure. Inappropriate expectations are best dealt with before surgery, as dealing with them postoperatively can be decidedly unsatisfying and unsuccessful.
Physical Examination
The patient is best examined in the standing position, with the arms comfortably at the sides. Any asymmetries in the size of the breasts, the position of the nipple-areola complex, and the level of the inframammary fold are noted. Measurements from the mid clavicle or the sternal notch down to the nipple are obtained, and the distance from the inframammary fold up to the nipple is noted. The latter measurement is important, as it serves as an indicator of the length of the pedicle when an inferior pedicle technique is used. The breast is palpated to assess for any potential masses, and the density of the parenchyma is noted. This is a useful observation to make, as dense fibrous breasts that are often seen in younger women are difficult to dissect, and the tissue remaining after resection often does not mold together as smoothly as a breast with a greater fat content. Finally, an assessment is made as to the estimated amount of breast tissue that will be removed from each side. Accuracy in this determination is helpful in streamlining the insurance preauthorization status. It is also a skill that improves with experience.
Photographic Documentation
Photographic documentation of the patient’s preoperative appearance is a vital part of the preoperative consultation. It is an important part of the patient’s record that can provide perspective if any complications or aesthetic concerns arise postoperatively. Three views of the breast documenting the appearance of the breast from the front and from each side adequately serve to record the patient’s preoperative condition. Supplemental views, including a three-quarters view, a hands-over-head view, and a photograph with the hands lifting the breast to allow the level of the inframammary fold to be seen, can be included for further documentation as needed. Framing the patient from the neck down to just below the level of the breasts with the width extending from just outside each arm will allow the shape, size, and position of the breast to be visualized and yet allow perspective with regard to the rest of the torso to be seen. As with all breast surgery, at no time is it necessary or desirable to include the patient’s face in the photograph.
Insurance Issues
Although breast reduction can occasionally be performed as a self-pay procedure, in the vast majority of instances, some type of insurance is used to pay for or help defray the costs associated with breast reduction. As such, many insurance plans have developed a preauthorization process designed to assess the severity of the patient’s condition and determine whether or not breast reduction would then be indicated. A common thread that applies to many insurance plans relates to documentation of the functional symptoms noted previously. Also, many plans will require what are called “conservative” measures to alleviate the patient’s symptoms, including participation in physical therapy or chiropractic therapy, and a trial of specially fitted support garments. Medical relief
of symptoms with a trial of oral analgesics and/or antiinflammatory drugs is also commonly required. Once these preliminary administrative details have been documented, an estimate as to the weight of tissue to be removed is made based on the surgeon’s previous experience. Typically at this point, a chart is then consulted that references the height and weight of the patient, and either the body surface area or the body mass index is calculated. By adding in the patient’s measurements, a minimum amount of tissue that must be removed to qualify for insurance coverage can then be determined. If the requirements for the symptom complex have been met along with the required (estimated) amount for removal, the procedure can be considered a covered benefit. Some plans offer automatic coverage at this point; others still require a formal letter of preauthorization. Regardless of the details, it is recommended in every circumstance to document the patient’s symptom complex thoroughly and make the best estimate for tissue removal that can be made. This information can prove very useful during the procedure to ensure not only adequate reduction of the breast but also enhanced symmetry in cases of marked breast volume asymmetry.
of symptoms with a trial of oral analgesics and/or antiinflammatory drugs is also commonly required. Once these preliminary administrative details have been documented, an estimate as to the weight of tissue to be removed is made based on the surgeon’s previous experience. Typically at this point, a chart is then consulted that references the height and weight of the patient, and either the body surface area or the body mass index is calculated. By adding in the patient’s measurements, a minimum amount of tissue that must be removed to qualify for insurance coverage can then be determined. If the requirements for the symptom complex have been met along with the required (estimated) amount for removal, the procedure can be considered a covered benefit. Some plans offer automatic coverage at this point; others still require a formal letter of preauthorization. Regardless of the details, it is recommended in every circumstance to document the patient’s symptom complex thoroughly and make the best estimate for tissue removal that can be made. This information can prove very useful during the procedure to ensure not only adequate reduction of the breast but also enhanced symmetry in cases of marked breast volume asymmetry.
Operative Strategy
Any procedure designed to reduce the breast must include four cardinal elements. First, a pedicle must be incorporated into the design that preserves the vascularity and innervation to the nipple-areola complex. Second, and closely related to pedicle choice, selected quadrants of the breast must be removed to accomplish the desired volume reduction. This is commonly accomplished by removing tissue from around the perimeter of the pedicle. Third, the excessive skin envelope must be managed in such a way as to minimize scarring as much as possible and yet allow a proportional relationship to be created between the remaining skin and the reduced breast volume. Fourth, an overall aesthetic breast shape must be created either as a function of the overall operative strategy or secondary to defined maneuvers designed to create a specific contour. Any procedure designed to reduce the breast will include these four elements, and analyzing these various and sometimes diverse procedures in this fashion will facilitate a greater understanding of each.
Inverted-T Inferior Pedicle
Pedicle: inferior
Volume reduction: medial, superior, and lateral
Skin pattern: inverted T
Shape: passive
The inverted-T inferior pedicle has been the preferred method of breast reduction around the world over the past 40 years, and it has clearly stood the test of time.7–10 The blood supply is based on an inferior pedicle, with the redundant tissue being removed from around the upper hemisphere of the pedicle. The excess skin is removed from the lower pole of the breast, including a V-shaped central vertical segment. The resulting scar is that of an inverted T or anchor shape. This has been also commonly referred to as a Wise pattern. Shape is created passively simply as a result of the wrapping of the skin flaps around the inferior pedicle that then settles under the influence of gravity. (See Video, Supplemental Digital Content 1, which highlights the marks and technical features of a standard inferior pedicle inverted-T or Wise pattern breast reduction, available in the “Related Videos” section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com.easyaccess1.lib.cuhk.edu.hk/PRS/A485.)
The main advantage of the inverted-T inferior pedicle technique is that it can be applied in any circumstance, from simple mastopexy to reduction for gigantomastia (Fig. 1). There is no defined upper limit related to volume for this technique. In extreme instances, the pedicle could be of such length that it outstrips the blood supply. In these circumstances, it is a simple matter to remove the nipple-areola complex, trim the pedicle back to a level of viability, and apply the nipple-areola complex as a skin graft. In contrast to this approach of using the nippleareola complex graft technique only when ischemia to the nipple-areola complex is identified intraoperatively,
some surgeons use this free nipple graft technique as a planned procedure for larger breast reductions deemed to be over a specific amount.11–13 Commonly used guidelines for using the free nipple-areola complex graft technique include reductions of over 1500 g from each side.
some surgeons use this free nipple graft technique as a planned procedure for larger breast reductions deemed to be over a specific amount.11–13 Commonly used guidelines for using the free nipple-areola complex graft technique include reductions of over 1500 g from each side.
 Video 1. Supplemental Digital Content 1, which highlights the marks and technical features of a standard inferior pedicle inverted-T or Wise pattern breast reduction, is available in the “Related Videos” section of the full-text article on PRSJournal.com or, for Ovid users, at http://links.lww.com.easyaccess1.lib.cuhk.edu.hk/PRS/A485. |
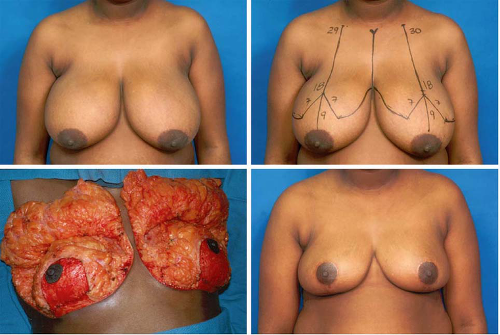 Fig. 1. (Above, left) Preoperative appearance of a 36-year-old woman in preparation for breast reduction using an inverted-T inferior pedicle approach. (Above, right) Preoperative marks. (Below, left) Intraoperative appearance after removal of the excess breast tissue and placement of the inferior/central pedicle into position. (Below, right) Appearance 1 year after removal of 600 g of tissue from the right breast and 650 g of tissue from the left.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|