Category
Definition
Risk of malignancy (%)
Recommendation
0
–
–
Additional imaging required
1
Negative
–
Annual follow-up
2
Benign finding(s)
0
Annual follow-up
3
Probably benign
<2
Term follow-up
4 (A, B, C)
Suggestive of malignancy
3–95
Biopsy recommended
5
Highly suggestive of malignancy
>95
Biopsy required
6
Known neoplasia
–
Conduct according to case
BI-RADS® category 0 must be reserved for cases in which an additional evaluation has to be performed, such as additional mammographic views with local compression or magnification, or even the complementary use of other tests (e.g., ultrasonography or MRI). It can also be used in cases where a comparison with previous tests is important, before a final impression is reached.
Cases classified as negative (category 1) or with benign findings (category 2) are followed up through annual routine tests.
In cases of probably benign lesions (category 3) which show a risk of malignancy lower than 2 %, a semester follow-up is recommended until 2–3 years has elapsed (according to the lesion) with the aim of determining the stability of the lesion. After such a period, if no alteration in the lesion is noticed, it is classified as category 2, and returns to the annual tracking group.
For lesions classified as category 4, the subdivision into categories 4A, 4B, and 4C is optional, but strongly recommended. Category 4A must be used when the risk of malignancy is low and a 6 month control period after biopsy or negative cytological findings is indicated. Category 4B indicates an intermediate risk of malignancy, so a good anatomic–radiological co-relation is needed. Category 4C includes findings of moderate suspicion in which malignancy is expected.
Lesions classified as highly suggestive of malignancy (category 5) have a risk of malignancy higher than 95 %. This group must be reserved for the group of classic tumor lesions such as spiculated masses, pleomorphic calcifications, and ductal calcifications in which a malignant lesion can only be ascertained after surgical evaluation of the region in question.
Category 6 is reserved for the group of lesions that are already diagnosed as being cancerous, and for which neoadjuvant chemotherapy or a second opinion is required. This category is not appropriate in cases of follow-up after breast-conserving surgery.
3.4 Mammography
3.4.1 Normal Mammographic Findings
There is a big variation in the appearance of a normal breast in a mammogram, mainly as to the size, shape, and composition of the parenchyma. The composition of the parenchyma may vary from almost totally substituted to extremely dense, and the sensitivity of mammography is directly related to this composition.
Liposubstituted breasts have excellent background tissue for tumor visualization, whereas high density can obscure tumor visualization.
The BI-RADS® composition of the breast is divided into four categories [6]:
1.
Category 1: breasts with severe adipose substitution (less than 25 % glandular tissue) (Fig. 3.1a)


Fig. 3.1
Mammographic patterns of mammary density according to BI-RADS®: severe adipose substitution (a), sparse fibroglandular densities (b), heterogeneously dense (c), and extremely dense (d)
3.
Category 3: heterogeneously dense breasts, which can obscure the detection of small lesions (approximately 51-72 % glandular tissue) (Fig. 3.1c)
4.
Category 4: extremely dense breasts, which can reduce the sensitivity of mammography (over 75 % fibroglandular tissue) (Fig. 3.1d)
Younger women tend to have a greater amount of fibroglandular tissue, although there is considerable variation within the same age range. As the age range increases or when the woman breastfeeds, the fibroglandular tissue tends to be replaced by fat. The replacement always occurs from the posterior region to the anterior region and from medial to lateral, in a symmetric way. An increase in mammary density can be observed during pregnancy and owing to the use of hormone-replacement therapy (HRT).
3.4.2 Abnormal Mammographic Findings
Masses and calcifications are the commonest abnormal findings in mammography. Other lesions that have been observed are architectural distortion, focal asymmetry, global asymmetry, retraction or cutaneous thickening, mammillary retraction, and axillary lymphadenomegaly.
3.4.2.1 Masses
Masses are described as lesions occupying space that is seen in at least two views. They are described according to shape, margin, and density [6].
The shapes can be round, oval, lobulated, or irregular (Fig. 3.2). Whereas oval and round shapes are usually related to benign lesions, an irregular shape is more associated with malignant lesions.
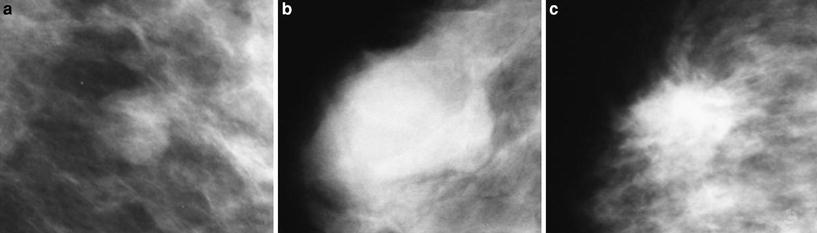
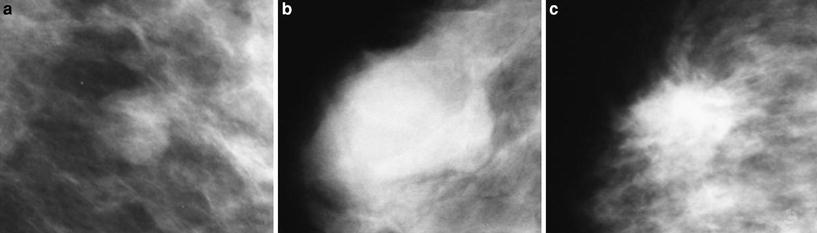
Fig. 3.2
Shapes of masses screened: round (a), oval (b), and irregular (c)
Margins are also an important indicator of malignancy, and they are described as circumscribed, microlobulated, obscured, indistinct, or spiculated (Fig. 3.3). Circumscribed lesions are defined as lesions that show at least 75 % of the margins as well defined, and they are associated with a possibility of malignancy lower than 2 % [32, 33]. These lesions are classified as probably benign (BI-RADS® 3 category) and it is recommended that a semester control is done. Microlobulated lesions and indistinct ones have a higher risk of malignancy, whereas spiculated ones are highly suggestive of malignancy.
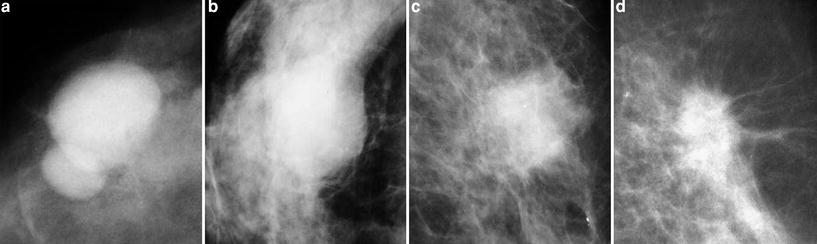
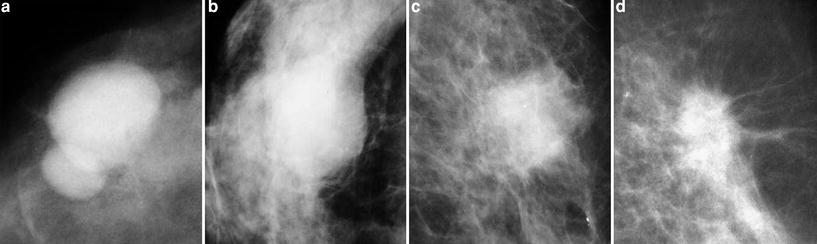
Fig. 3.3
Margins of masses screened: circumscribed (a), obscured (b), indistinct (c), and spiculated (d)
The density of masses may also point to their origin, being described as high density, low density, isodense to parenchyma, and fat density (Fig. 3.4). Generally, benign lesions tend to be less dense than malignant ones, although this is not always true. The existence of fat density inside the mass confirms its benign nature.
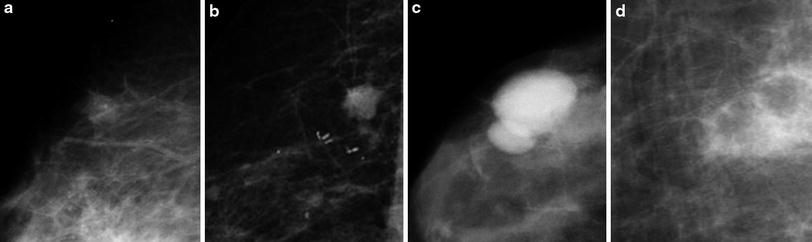
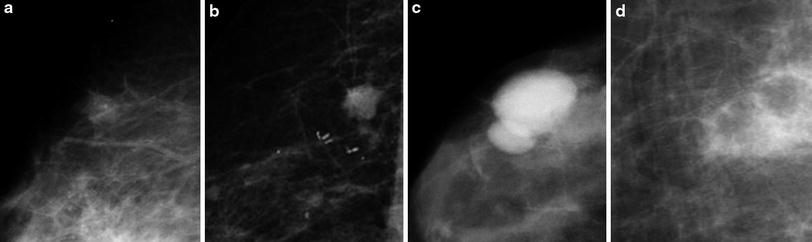
Fig. 3.4
Density of masses screened: low density (a), isodense (b), high density (c), and fat density (d)
Finding associated lesions may help define the nature of lesions, such as gross calcifications (associated with fibroadenoma in involution) and pleomorphic calcifications (related to malignant lesions), cutaneous retraction, and mammillary retraction.
3.4.2.2 Calcifications
Calcifications are described according to their morphology and distribution. Morphology shows a good correlation with the nature of calcifications, and they can be classified as [6]:
1.
Typically benign: skin calcifications (lucent-centered), vascular calcifications (parallel lines associated with vascular structures), “popcorn”-type calcifications (coarse and associated with mass images, corresponding to fibroadenoma in involution), gross tubular calcifications (associated with duct ectasia), round (frequently formed in acini and lobes), rodlike calcifications (lucent-centered), “eggshell” calcifications (calcium deposit on the cyst walls or of fat necrosis), “milk of calcium” calcifications (sediment calcifications inside the cysts), suture calcifications (formation of calcium around the sutures), dystrophic calcifications (in irradiated breasts and those undergoing traumas) (Fig. 3.5).
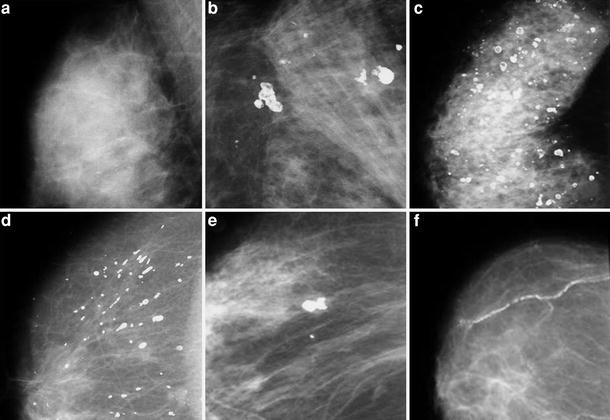
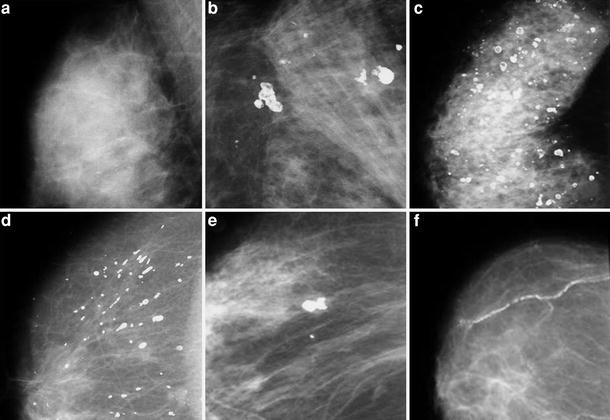
Fig. 3.5
Typically benign calcifications: “milk of calcium” (a); dystrophic (b), round and rodlike (c); gross tubular (d), “popcorn” type (e), and vascular (f)
2.
Of intermediate concern: amorphous or indistinct calcifications (frequently small and with morphology that is difficult to define, commonly mistaken for benign calcifications; when grouped they should be correlated with biopsy findings); heterogeneous calcifications (they are larger and tend to coalesce, so they can be associated with malignancy or with an initial phase of dystrophic calcifications of fibrosis, fibroadenoma or trauma) (Fig. 3.6).
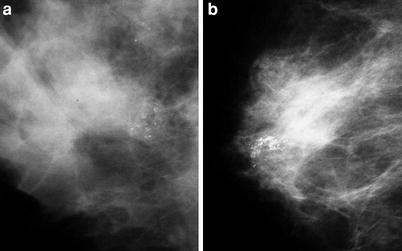
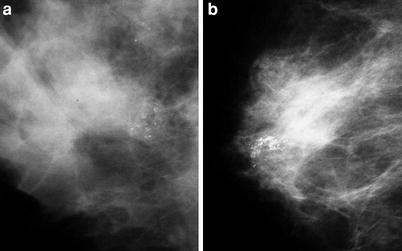
Fig. 3.6
Microcalcifications of intermediate concern: amorphous (a) and heterogeneous (b)
3.
Higher probability of malignancy: fine pleomorphic calcifications (they show a wide variety of shapes and sizes, generally less than 0.5 mm) and ductal calcifications (fine and irregular calcifications on the duct tracks, which suggest that there is participation of the duct through the tumor) (Fig. 3.7).
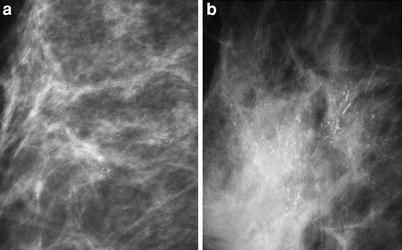
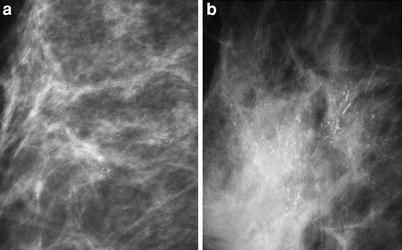
Fig. 3.7
Microcalcifications of higher probability of malignancy: fine pleomorphic (a) and ductal (b)
We can describe the distribution of calcifications as follows:
1.
Diffuse: distributed at random in the breasts, generally found in benign calcifications.
2.
Regional: found in a broad area of the breast, but with no duct track. One or more quadrants may be involved, and the risk of malignancy is associated mainly with calcification morphology.
3.
Clustered: they is used when at least five calcifications occupy a small volume of the breast, and there is high risk of malignancy.
4.
Linear: this points to a ductal distribution, increasing the risk of malignancy.
5.
Segmental: this point to damage to the ducts and their branches in an area of the breast, also increasing the risk of malignancy.
3.4.2.3 Architectural Distortion
Architectural distortion is defined when normal architecture of the breast is altered; however, there is no evident mass (Fig. 3.8). When there are no records of trauma or surgery, distortion leads to a condition highly suspicious of malignancy or a radial scar; therefore, histological evaluation is recommended [6].
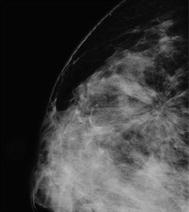
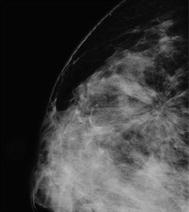
Fig. 3.8
Architectural distortion in mammography
3.4.2.4 Special Cases
Some alterations can be seen through mammography, and they are described as follows [6]:
1.
Isolated duct dilation: If not associated with other relevant clinical suspicious findings, it is not considered important.
2.
Intramammary lymph nodes: They are usually smaller than 10 mm, they have a fatty hilum, and have a reniform shape. They can appear in any breast region, although they are mainly found in lateral quadrants.
3.
Global asymmetry: This generally represents an anatomic variation, which is identified during the comparison with the contralateral breast. It cannot be associated with the palpable mass, the architectural distortion area, masses, or microcalcifications.
4.
Focal asymmetry: This is defined as a lesion that cannot fill the criteria of mass required, and is visualized in both views as similar shapes. It may represent a normal parenchyma island; however, often it has nonspecific characteristics, so it demands additional investigation.
5.
Related findings: Some findings may increase the suspicion of malignancy when identified together with the suspicion of a lesion, represented by skin retraction, nipple retraction, skin thickening, and axillary lymphadenomegaly among others.
3.5 Ultrasonography
Mammary ultrasonography is a diagnostic method that aids in the characterization of alterations detected either in clinical or mammographic examinations [27, 28]. Besides allowing differentiation of solid masses and cystic ones, it supplies additional data to characterize lesions as benign or malignant; it also aids in the analysis of dense breasts through mammograms and it guides percutaneous procedures.
3.5.1 Normal Ultrasonographic Findings
As in mammography, the ultrasonographic aspect of the breast also varies according to its composition. The mammary echotexture results from the combination of the fibroglandular tissue (echogenic), fat (hypoechoic), and connective tissue (ligaments of Cooper, echogenic). These echotexture patterns may affect the sensitivity for lesion detection, therefore reducing the sensitivity for solid mass detection in very liposubstituted breasts, or even simulate alterations in cases of heterogeneous breasts, which must be evaluated and differentiated in real time throughout the examination.
Three echotexture patterns are described according to BI-RADS® [6]:
1.
Homogeneous—fat (Fig. 3.9a)
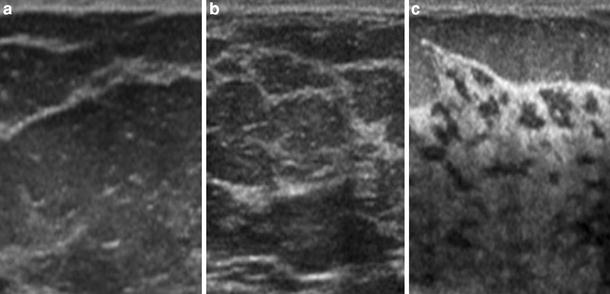
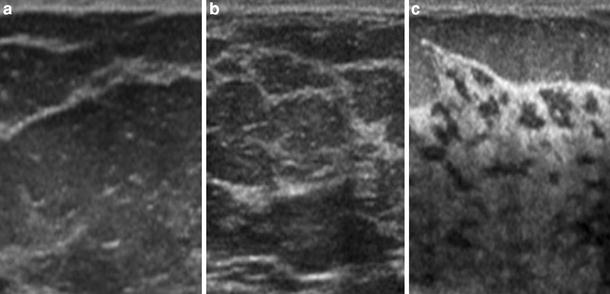
Fig. 3.9
Echotexture patterns in ultrasonography according to BI-RADS®: homogeneous—fat (a), homogeneous—fibroglandular (b), and heterogeneous (c)
3.
Heterogeneous—fibroglandular elements, fat elements, connective tissue and ducts, interspersed; a pattern of younger breasts with little liposubstitution (Fig. 3.9c)
3.5.2 Abnormal Ultrasonographic Findings
The evaluation of masses detected both through mammography and through physical examinations is the most frequent indication for ultrasonography. Calcifications are poorly evaluated through this method, as their detection becomes more difficult, and their morphological evaluation is not possible.
3.5.2.1 Masses
Masses must be detected and analyzed on more than one view to differentiate them from normal anatomic structures. They are echographically described according to shape, orientation, margins, transition with mammary tissue, echogenicity pattern, posterior acoustic aspect, and relations with and effects on the adjacent tissue [6, 28].
The shape can be defined as round, oval, or irregular (Fig. 3.10). When it is oval, it is called macrolobulated if it has up to three lobulations. Interpretation of the examination concerning benignity and malignancy of the mass is similar to that for mammography, and irregular masses are the most suspicious.
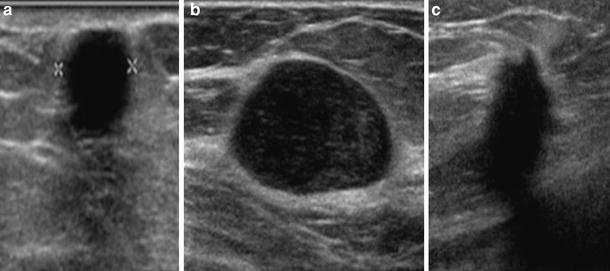
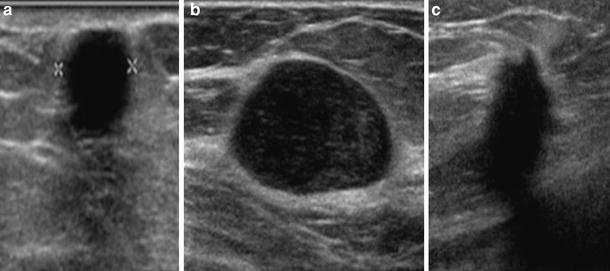
Fig. 3.10
Shape of masses screened through ultrasonography: round (a), oval (b), and irregular (c)
Orientation is a particular aspect of ultrasonography (Fig. 3.11). Masses that are parallel to the skin, that is, wider than higher, are generally benign. When the orientation is vertical, that is, higher than wider, this is more suggestive of malignancy, as it represents a growth through normal tissue planes.
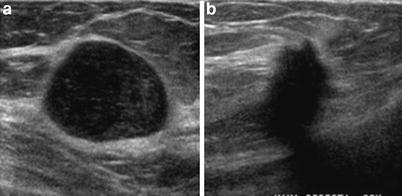
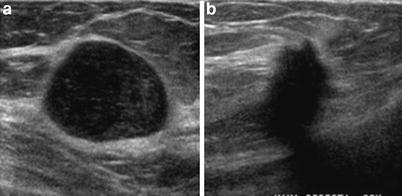
Fig. 3.11
Orientation of masses in ultrasonography: parallel to the skin (a) and perpendicular to the skin (b)
Margins are described as circumscribed, indistinct, spiculated, angular (projections forming acute angles), and microlobulated (various small lobulations of 1–2 mm) (Fig. 3.12). Except for the circumscribed margin, the various aspects are suggestive of malignancy. The spiculated margins and/or microlobulated margins are the ones that have the highest predictive value for malignancy [28, 29].
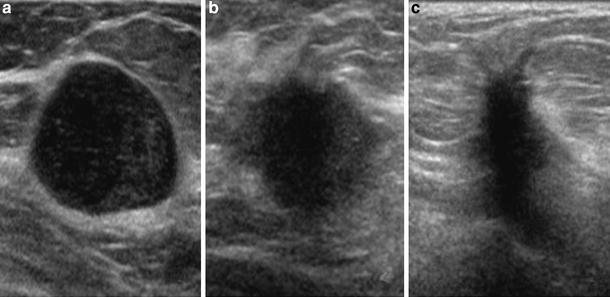
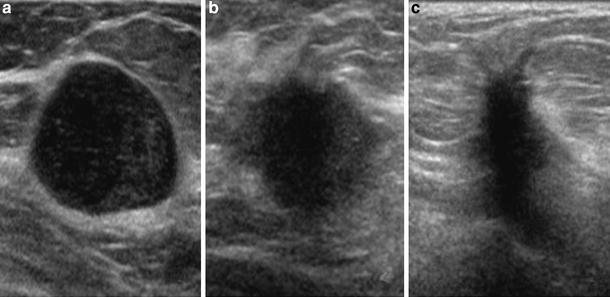
Fig. 3.12
Margins of masses in ultrasonography: circumscribed (a) indistinct (b), and spiculated (c)
The transitional zone with the adjacent mammary parenchyma is described as defined or undefined. The well-defined transition or that with an echogenic halo indicates benignity, as it shows a lesion of slow growth compressing the parenchyma around and not infiltrated. The transition without defined demarcation is associated with some carcinomas and abscesses. The finding of an echogenic pseudo-capsule around the lesion must be interpreted together with the lobe shape (oval or slightly lobulated) to reinforce the sureness of benignity [28].
The echogenicity pattern aids primarily with the differentiation between cystic mass (anechoic) and solid mass (hypoechoic, isoechoic, and hyperechoic), defined in relation to fat (Fig. 3.13). Homogeneously hyperechoic masses are considered of higher predictive value for benignity. Solid hypoechoic and isoechoic masses need other characteristics for evaluation concerning malignancy. Complex masses have mixed echogenicity, with both anechoic and echogenic components [28].
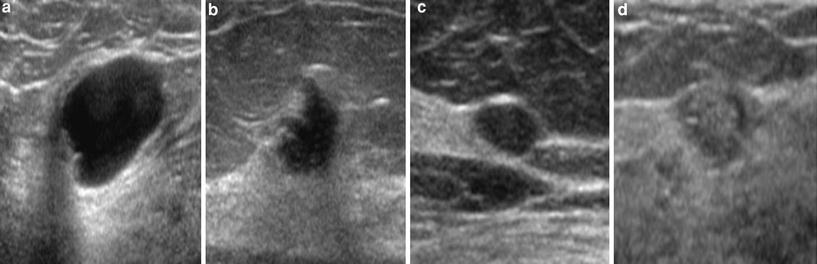
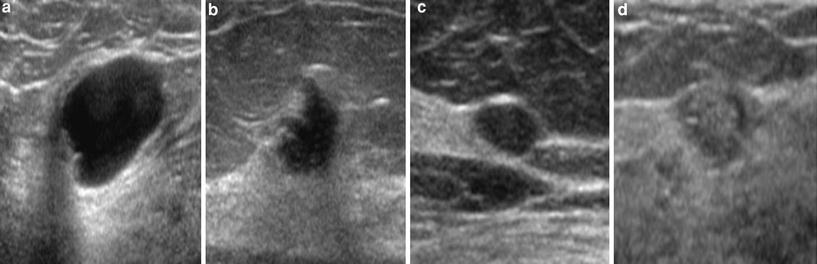
Fig. 3.13
Echogenicity patterns of masses in ultrasonography: anechoic (a), hypoechoic (b), isoechoic (c), and hyperechoic (d)
The posterior acoustic phenomena result from attenuation of the mass (Fig. 3.14), except for posterior peripheral shadow, which occurs as a result of an alteration of the speed of the acoustic beam at the curved edges in either oval or round masses. These phenomena include acoustic reinforcement, that is, more echogenic posterior area, which is found mainly in cysts. Also, an acoustic shadow has been observed, that is, a darker central posterior area, which is associated with calcifications, fibrosis, or neoplasia with high desmoplastic reaction. Some masses do not cause an alteration of the acoustic beam through the mass. These aspects are not reliable for the definition of benignity or malignancy and they must be considered in co-relation with other aspects [28, 29].
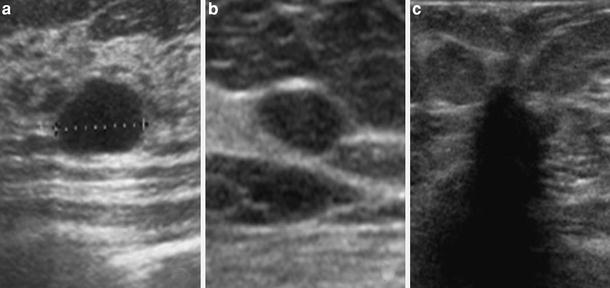
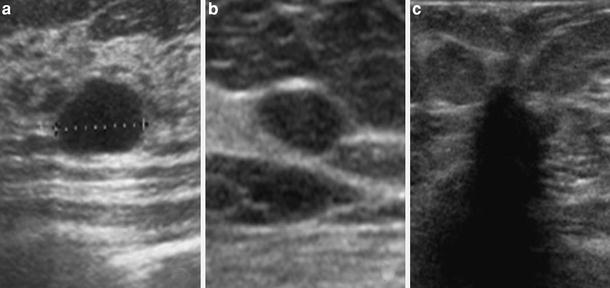
Fig. 3.14
Acoustic phenomena of masses in ultrasonography: acoustic reinforcement (a), no alteration of the acoustic beam (b), and acoustic shadow (c)
Masses may have some effects on adjacent mammary parenchyma. Benign lesions tend to produce fewer alterations, such as compression. More aggressive and infiltrating lesions may obliterate the adjacent tissue planes, pull or thicken Cooper’s ligaments, and cause edema or architectural distortion of the parenchyma, as well as rupture of the regular anatomic planes. The ducts may be pulled and dilated, and the skin may have focal or diffuse thickening (normal is 2 mm or less), retraction, and irregularity.
3.5.2.2 Calcifications
Ultrasonography has very low sensitivity for the detection of calcifications, especially microcalcifications. It also does not allow their morphological analysis, which is important for characterization of malignancy. Among other factors, the low sensitivity results from heterogeneous breast echotexture and from the small size of the microcalcifications (less than 0.5 mm), with no typical posterior acoustic shadow [6, 28].
3.5.2.3 Special Cases
Some alterations exhibit characteristic findings [6]:
1.
Clustered microcysts: These are defined as small anechoic clustered images (less than 2-3 mm) with thin septations inside (less than 0.5 mm), with no associated solid component. When not palpable, they are considered as probably benign lesions (category 3). This finding occurs mainly with fibrocystic alterations and in the apocrine metaplasia (Fig. 3.15a).
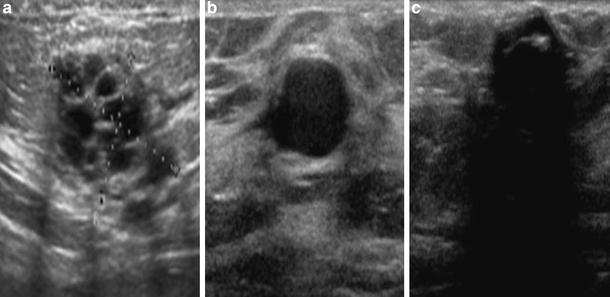
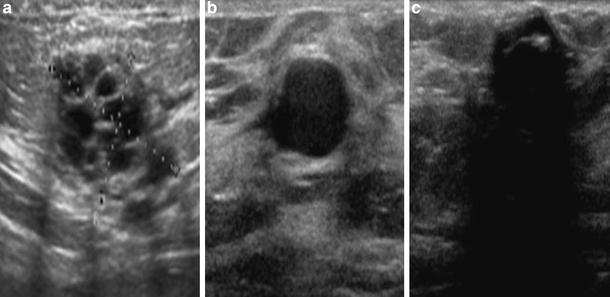
Fig. 3.15
Special cases observed through ultrasonography: clustered microcysts (a), complicated cysts (b), and foreign body related to draining (c)
2.
Complicated cysts: These are cysts that have thin echoes inside the fluid level or even mobile debris, with no solid component attached to the wall. These are also considered as probably benign lesions (category 3) (Fig. 3.15b).
3.
Skin masses: These are the so-called epidermal and sebaceous inclusion cysts, keloids, neurofibromas, and accessory nipples. They are classified as benign lesions (category 2).
4.
Foreign bodies: These may correspond to surgery marking clips, threads, catheters, silicone, metal, or glass from trauma. Clinical history is very important for differentiation. Free silicone in the parenchyma has a typical aspect of a “snowstorm,” that is, an echogenic area that causes a marked acoustic shadow, obscuring the deep structures (Fig. 3.15c).
5.
Intramammary lymph nodes: These are described as oval masses, circumscribed, with an echogenic center and a hypoechoic periphery. They are located mainly in the upper quadrants and sides of the breast, and their size ranges from 0.3 to 1 cm.
6.
Axillary lymph nodes: The aspects are similar to those of the intramammary lymph nodes, and they can measure more than 2 cm. When they are too big (above 4 cm) or with a hypoechoic center, they must be evaluated so the possibility of a metastatic disease is not ignored.
3.5.2.4 Vascularity
This is an additional piece of data for the evaluation of masses or suspicion areas, although with limited value. The complete absence of vascularity is usually observed in cysts. A rather increased vascularity may be suggestive of neovascularity and it is usually observed not only inside the mass but also in the peripheral area of a lesion, or diffusely in the surrounding tissue [6].
3.6 Magnetic Resonance Imaging
MRI is the most accurate method for the detection of breast cancer and it is indicated in selected cases to increase the sensitivity that results from traditional methods (mammography and ultrasonography). The method has the advantage of showing a three-dimensional view of the breast, with high sensitivity and no use of ionizing radiation. Among the disadvantages are the high cost of the procedure and its low specificity [30].
MRI analysis must be made through images obtained from the dynamic technique during the endovenous injection of paramagnetic contrast material (gadolinium), associated with enhancement kinetics. Then, images are obtained with spatial high resolution for a detailed morphological evaluation of the lesion with the aim of detecting characteristics of suggestive malignancy. Interpretation of MRI findings must consider the clinical history data (including physical examinations—palpation of the masses, skin appearance, scars; surgical antecedents of those of biopsies; menstrual cycles; HRT; radiotherapy) and comparison with the findings of previous examinations (mammography and ultrasonography—identification of areas with suggestive lesions, mainly microcalcifications, evaluation of temporal stability, or the appearance of new lesions, among others).
3.6.1 Normal Magnetic Resonance Imaging Findings
Breast anatomy is thoroughly demonstrated through MRI, by which not only the parenchyma can be evaluated, but also vessels, lymph nodes (intramammary and those from axillary prolongations), the retromammary area, and the thoracic wall; these latter are difficult to access through other imaging methods.
The parenchyma is characterized and described according to BI-RADS® criteria [6]:
1.
Severe adipose substitution
2.
Disperse fibroglandular density
3.
Heterogeneously dense
4.
Extremely dense
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








