Introduction
Breast augmentation, according to the most recent procedural statistics data from the American Society for Aesthetic Plastic Surgery, continues to have increased popularity as the most common surgical procedure in the United States and was performed in more than 330,000 women in 2017. The most common incision access used is the inframammary approach worldwide, based largely a long-existing bias that this approach is most simple to perform with the best ability to accomplish consistent results.
There is an evolving body of literature, however, that suggests that the transaxillary approach can be performed with results that are comparable in terms of consistent and predictable outcomes, with the advantage of the avoidance of an incision on the breast for primary breast implant placement. In their recent literature review for outcomes-based analysis for breast augmentation, Lista and Ahmad suggest that the transaxillary approach is preferred equally to the inframammary approach for breast implant placement. Numerous additional studies have reported excellent and predictable outcomes using the transaxillary approach with several variations of technique.
This chapter discusses the author’s preferred technique for transaxillary breast augmentation with the aid of endoscopic assistance. , This includes a discussion of rationale for this approach and an emphasis on specific aspects of technique that allow for consistent technical control and outcomes that equal the more universally popular inframammary approach.
Indications and Contraindications
The author views any patient who is a candidate for breast augmentation as a candidate for the transaxillary approach. The deciding factor on whether this approach is used becomes an issue of patient choice. An important aspect of this choice by the patient comes down to correct information relative to the transaxillary approach, because many surgeons claim to offer the approach and then criticize it, often based on a lack of experience or just because they do not prefer the approach, to then offer only the inframammary approach with which they may be more comfortable.
After an explanation of the technique, how it works, and that the addition of the endoscope allows for precise technical control in the author’s hands that makes the procedure identical to the inframammary approach in terms of the internal cuts made, the patient can then select her preferred approach. The only difference between the axillary approach, in the technique of the author, is the set of instruments used to create the partial subpectoral pocket. The patient selects the transaxillary approach if she prefers that her breast implants be placed with no incisions on the breast.
An issue that can be confusing is whether certain tissue types represent contraindications to the transaxillary approach. The author uses the approach in any patient who is otherwise an appropriate candidate for breast augmentation. This applies to patients with all tissue types and who request any type of breast implant device used by the author in his clinical practice. This also applies to patients who have minimal ptosis, after a detailed explanation and distinction from patients who have significant ptosis and require a breast augmentation with mastopexy.
Preoperative Evaluation and Special Considerations
The main issues for preoperative evaluation include the preference of incision location, accurate education relative to the choice of incision relative to the technique for pocket creation, and an assessment of tissue type with the resultant discussion of whether the patient can achieve the outcome desired should her tissue position be low as a result of mammary ptosis. This issue is emphasized because of the large subgroup of patients in the author’s revision practice from outside who had ptosis addressed by breast augmentation with subsequent dissatisfaction with the position and appearance of the augmented breast because a mastopexy was not pursued.
There are several important issues relative to incision location that should be understood. The transaxillary incision, when properly placed within the hair-bearing skin, will almost always heal in a way that is difficult to see postoperatively. The timing of the incision becoming difficult to see may vary to some degree based on the ethnicity of the patient, with the longest maturation time frames noted in Asian, Hispanic, and red-haired Caucasian patients. The author informs his patients that the incisions usually are difficult to see by 1 year, with distinct improvement seen at 4 months.
The author has performed the transaxillary approach routinely in patients who are avid tennis players, entertainers, and cheerleaders for major conference sporting events who usually have no issues as long as there have been appropriate expectations created through patient education. These patients can elect the inframammary approach or the axillary approach, then, if they prefer to have their implants placed with no incisions on their breasts. The periareolar approach is not currently offered on a routine basis by the author unless requested by a patient.
Surgical Technique
Preoperative Markings
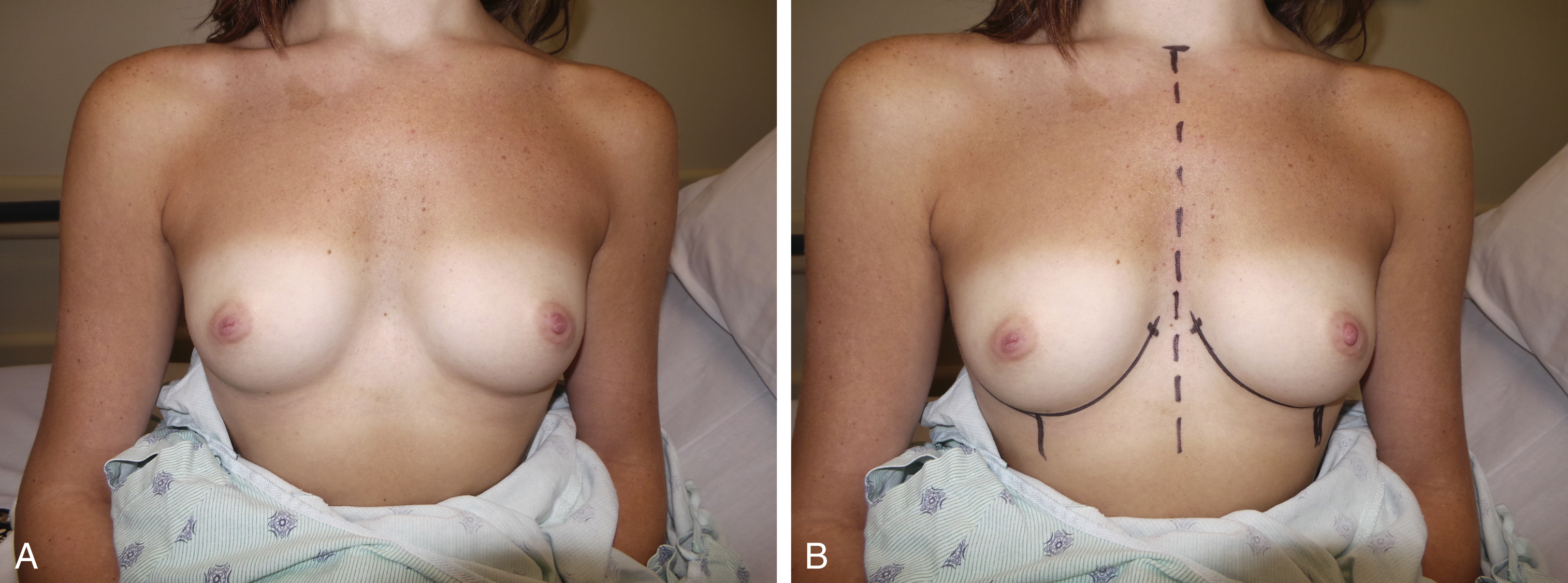
The author has a preferred sequence of preoperative markings. The markings begin with an interrupted line to show the midline of the chest, from the sternal notch to the xiphoid process. It is important that any issues relative to minor or significant asymmetries in ribcage shape are noted. This is important in both preoperative patient education and preoperative markings. The preoperative inframammary fold (IMF) is then marked, along with the mid-breast meridian on each side. The preoperative breast width, desired breast width, and lateral tissue thickness measurements are checked and marked just below the clavicle for reference and documentation ( Fig. 3.1A, B ).
The proposed changes in IMF location and shape are then marked on each side, based on a combination of the tissue type present and the type of implant used. This process for these determinations are based on the nipple-to-IMF distance on strong stretch, which must equal the sum of the height of the implant planned (equal to the diameter of a round implant) and the implant projection divided by 2, plus 0.5–1 cm if the tissue is fairly thick, as described by Caplin as the St. Louis Formula ( Fig. 3.2A ). This approach is used regardless of incision location in the practice of the author.
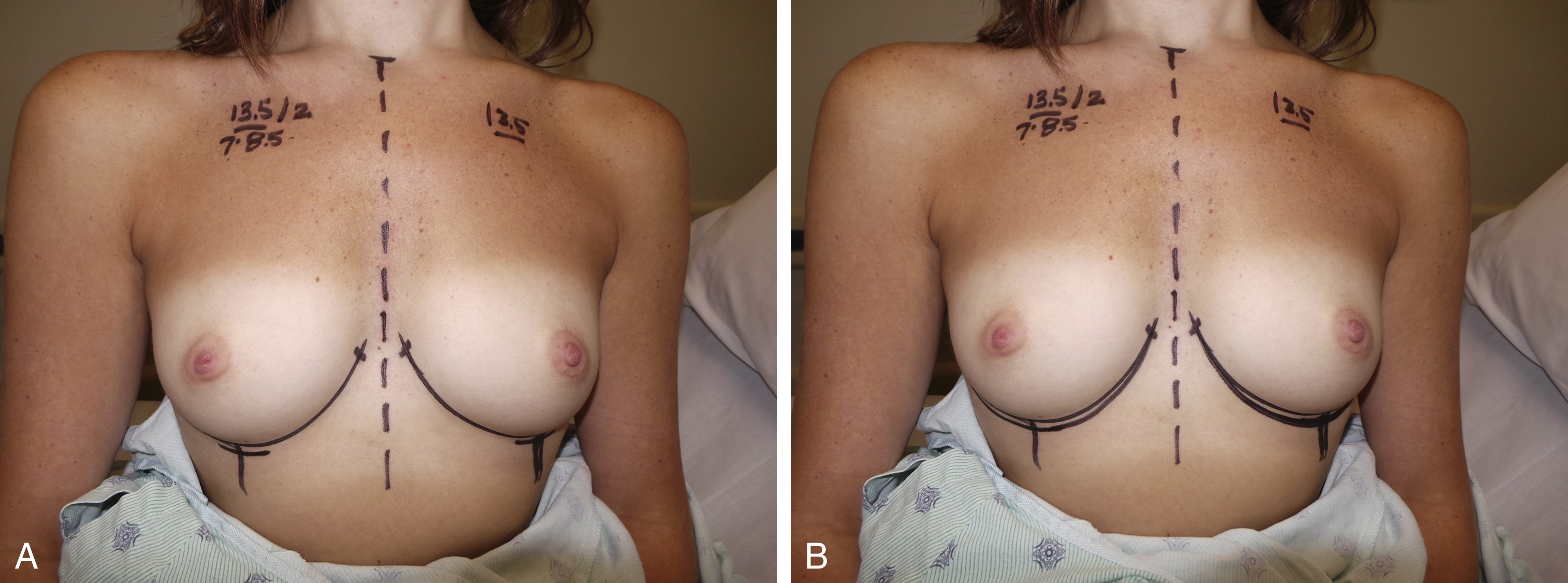
The central level markings are checked by a sternal notch to mid-breast meridian at IMF measurement, with confirmation of equal distances present. Allowances are made for meaningful differences of ribcage shape from side to side. The IMF markings are then extended medially and laterally as indicated. The superior aspect of the medial IMF is marked and used as a reference for the superior-most division of the pectoralis major muscle release ( Fig. 3.2B ).
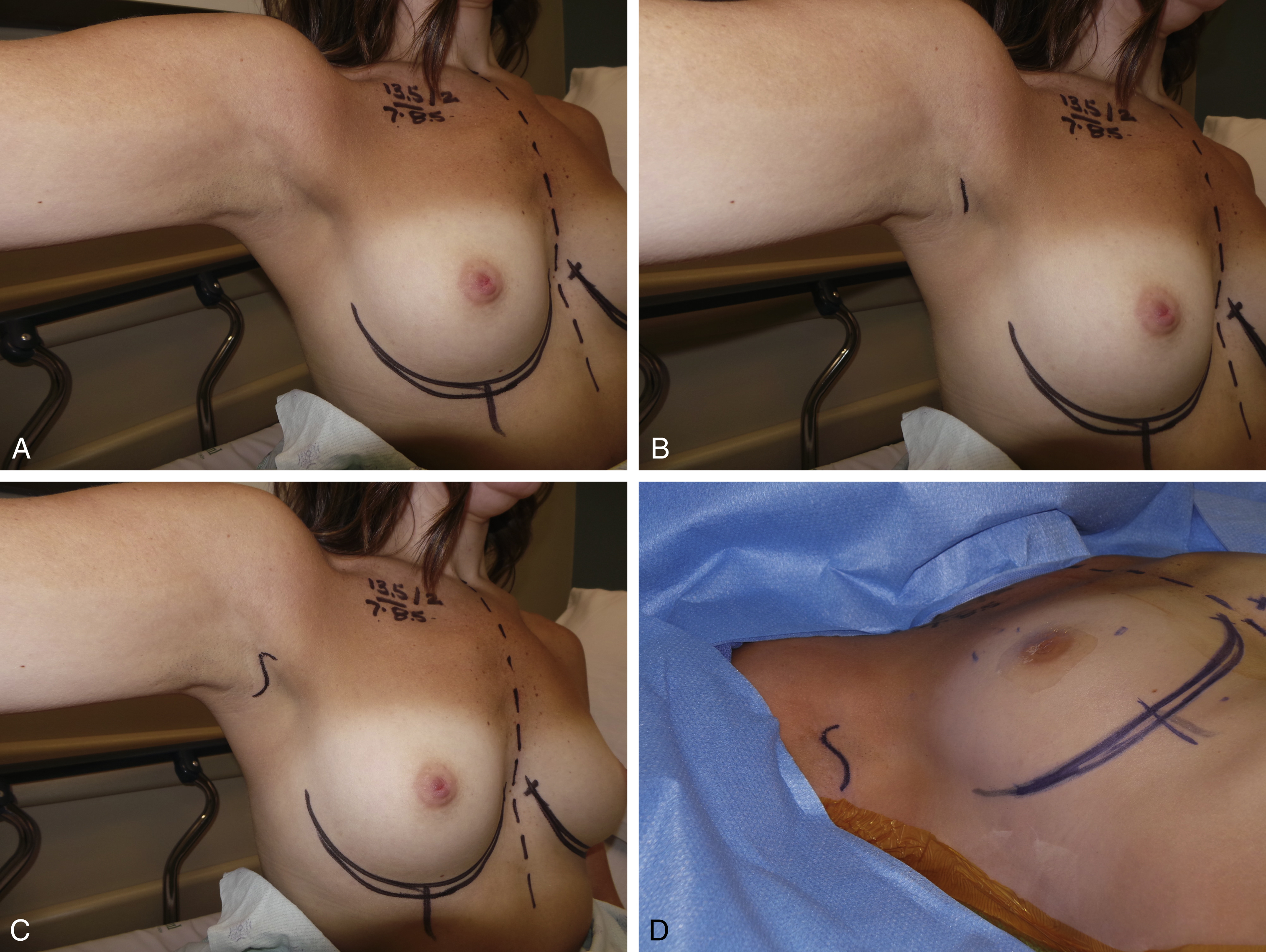
The next issue for markings is the incision. Regardless of the type of implant to be used, the first mark is in the axillary apex. A dominant skin crease is used for the incision location if present, but mainly for the incision anterior to the axillary apex marking. The posterior aspect of the incision may be directed slightly superiorly to keep the incision within the hair-bearing skin ( Fig. 3.3A–D ). The key concept is that the incision must be kept within the hair-bearing skin in all aspects. The incision designs used routinely by the author in his practice include open V, boomerang, and open S shapes. Photos of markings are then taken in the preoperative holding area that are used for reference as needed during the procedure.
Intraoperative Markings
The preoperative markings are then routinely rechecked at the start of the procedure, with the patient prepped and draped and the arms extended and out 90 degrees from the chest. Special attention is given to the nipple-to-IMF distances both at rest and on stretch. The reason for this is because the author then conducts the procedure to release the tissue and create a tissue pocket to the markings in all areas. This is the reason that the preoperative markings are performed with great attention to detail.
Details of the Procedure
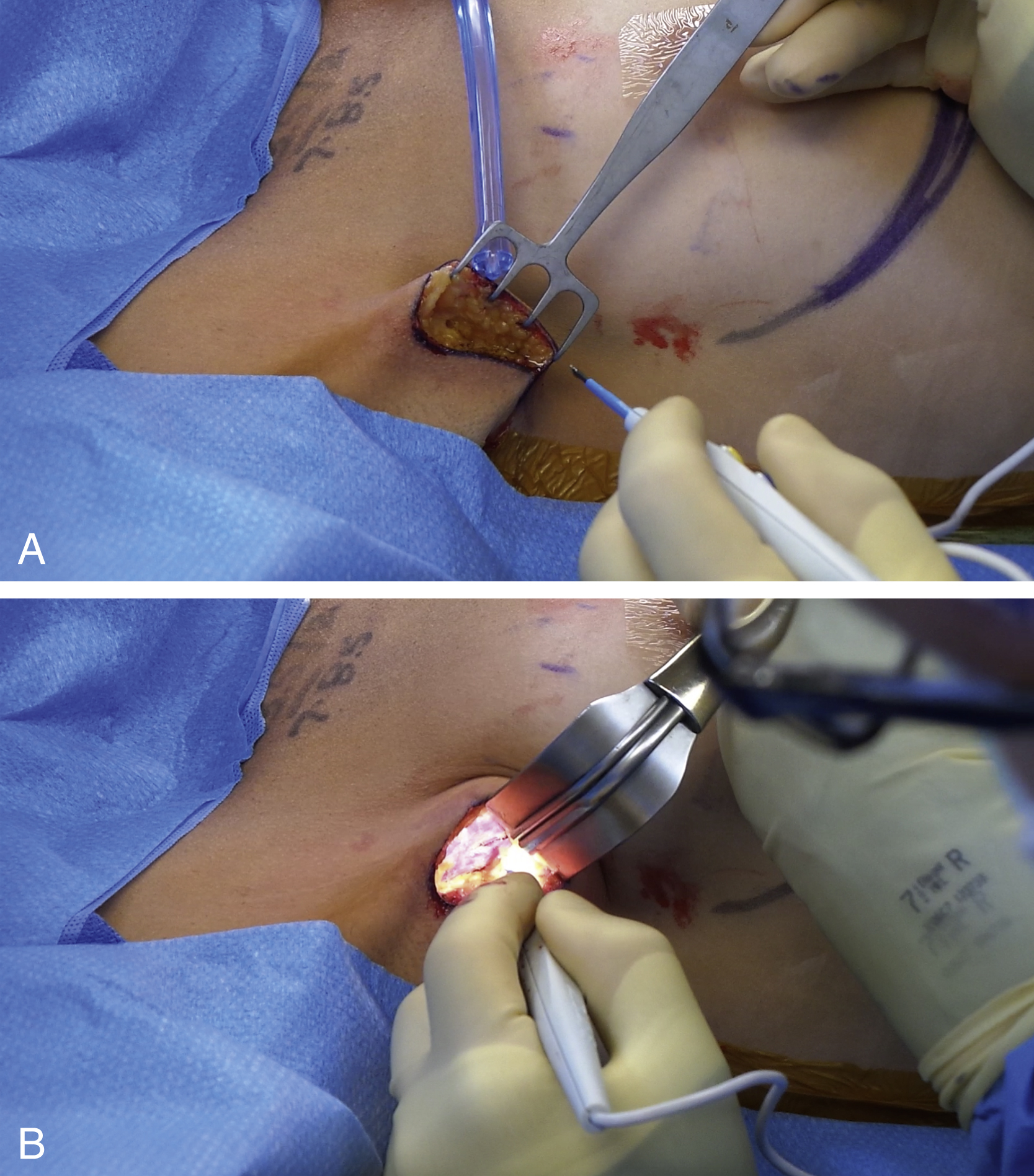
Incision and Tissue Tunnel
A 4-cm incision is placed in the axilla as described earlier. A cross-hatch marking is made in the axillary apex to serve as a reference for alignment during closure. A thin skin flap is then created in an anterior direction, toward the lateral border of the pectoralis major muscle. It is important to note that this dissection avoids entry into the axillary contents and minimizes damage to the intercostobrachial nerve. A four-prong skin flap is helpful to create this flap, with repeated checks to ensure correct thinness of the flap ( Fig. 3.4A ). A fiber-optic retractor is then used to expose the lateral border of the pectoralis major muscle ( Fig. 3.4B ). Once identified, the fascia is entered and the lateral border of the muscle is exposed. Using a finger moved right along the undersurface of the pectoralis major muscle, a plane is created between the pectoralis major and pectoralis minor muscle below. A finger-sweep type maneuver is used to develop this tissue plane. This can be developed using the cautery, but the author has not found this approach to be helpful. This is the one area that the author prefers gentle blunt dissection in the transaxillary approach. The tissue tunnel for entry of the implant has been preliminarily created with the technique described to this point.