Breast Augmentation and Reconstruction Using Brava External Breast Expansion and Autologous Fat Grafting
Roger K. Khouri
Daniel Del Vecchio
Introduction
In plastic surgery few topics warrants as much controversy, excitement, and curiosity as fat grafting to the breasts. Although the solution to the “fat puzzle” is far from solved, results from a variety of independent investigators suggest that fat grafting to the breast is a legitimate procedure that warrants careful study. In January 2009 the American Society of Plastic Surgeons (ASPS) reversed their previous position on fat grafting to the breasts, stating, “studies provide consistent evidence for…fat grafting for breast augmentation…as a safe method” but cautioned “results of fat transfer remain dependent on a surgeon’s technique and expertise” (1). This chapter we outline our rationale, collective techniques, and clinical experience in more than 100 cases and describe our current process from initial patient selection to postoperative care.
History
In 1983 Illouz (2) showed that fat can be removed from small port incisions using a cannula connected to vacuum. This offered surgeons an opportunity to use liposuctioned fat as an autologous filler. However, because many of the variables so important to fat grafting were not well understood, early results were disappointing as related to volume maintenance. At the same time, the success of the silicone breast implants reduced the interest in fat grafting for breast augmentation.
In 1987, Bircoll published his experience with the autologous grafting of liposuctioned fat for breast augmentation (3,4). This was followed by a series of opinion letters to the editor that culminated in the American Society of Plastic Surgeons issuing a position statement questioning the safety of fat grafting to the breast (5). This opinion statement suggested that fat grafting would compromise breast cancer detection and should be prohibited. Because of this unprecedented strong ban and because early results were neither impressive nor reproducible, this position statement stood, and the technique was largely abandoned for more than 20 years.
Some Europeans, undeterred by the ASPS position, persisted and continued to push for the technique, although not for cosmetic augmentation. Emmanuel Delay in Lyon, France, presented a series at the French Society of Plastic Surgery in 2001 and Gino Rigotti in Verona, Italy, also had a large series that he presented at the American Association of Plastic Surgeons in 2005.
At the 2006 meeting of the American Society for Aesthetic Plastic Surgery (ASAPS), Baker et al. presented a series of 20 patients augmented with a combination of external expansion and fat grafting (6). Using serial breast magnetic resonance imaging (MRI) and three-dimensional (3D) volumetric analysis, they described a 180-mL augmentation with documented volumetric survival of the grafts. None of the women had difficult-to-interpret findings on the mammogram. At the latest update of this prospective clinical trial, with more than 40 women followed up for at least 6 months and for an average of 30 months, there were still no issues with breast imaging or difficult-to-interpret masses (7).
In 2007, Coleman and Saboeiro published a review of 17 patients who were grafted using autologous fat and were followed up with serial photography (8). The results were overall successful, with maintenance of volume over 7 to 12 years of follow-up. They used serial grafting sessions instead of injecting large volumes in a single session in a preexpanded recipient breast like Baker et al.
With the growing realization that with optimal technique, fat grafts to the breast have potential to survive long term and that the radiographic arguments behind the ASPS-imposed ban were no longer valid (9,10,11,12,13,14,15), many surgeons across the world have started publishing their previously unpublished work (16,17,18,19,20,21).
Large-Volume Fat Grafting
Scientific Variables and Their Relative Importance
Large-volume fat grafting required for effective breast augmentation and reconstruction has to be distinguished from the relatively smaller volume fat grafting needed to improve contour defects or to restore age-related fat atrophy in the face. Because of the large volume of donor necessary, it represents greater technical challenge. The first step in understanding the science and optimizing patient safety and results in fat grafting is to understand the many variables involved. Applying what is known from skin grafting and solid organ transplantation can provide a starting point. A more basic science approach to variables in fat grafting might employ tissue transplantation as a benchmark as suggested in Table 118.1.
A more challenging step is quantifying the relative weights of these variables. Determining the relative importance of each variable helps to guide priorities in patient selection, surgical management, and technique.
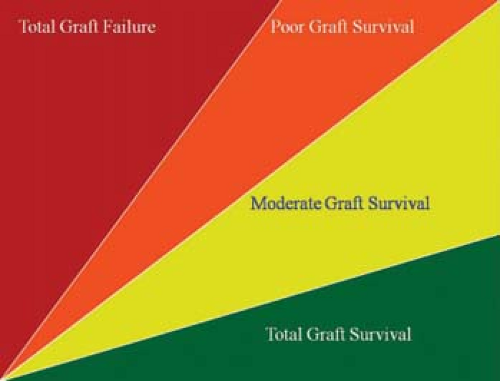
Percentage graft survival is a frequently referred to outcome measure that has to be put in proper perspective. It would be relatively easy to get a 10-mL graft volume to survive completely
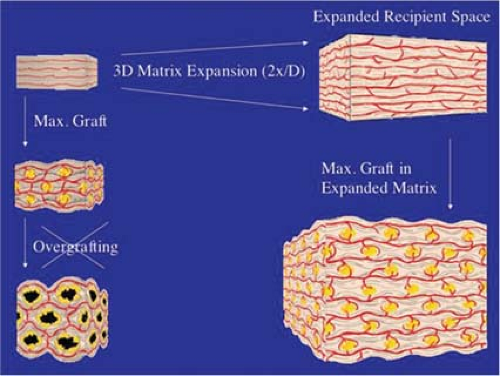
if evenly dispersed, one cell at a time, in a 100-mL recipient, while it would be rather impossible to squeeze 100-mL grafts into a 10-mL recipient site. Therefore percentage graft survival is critically dependent on the ratio of graft to recipient volume. This is illustrated in Figure 118.1.
if evenly dispersed, one cell at a time, in a 100-mL recipient, while it would be rather impossible to squeeze 100-mL grafts into a 10-mL recipient site. Therefore percentage graft survival is critically dependent on the ratio of graft to recipient volume. This is illustrated in Figure 118.1.
Table 118.1 Variables in 3-D Fat Transplantation | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Theoretical Concepts in Large-Volume, Three-Dimensional Fat Grafting
Fat grafting is 3D grafting, a novel concept for surgeons more familiar with the two-dimensional skin grafting. Large-volume fat grafting can be compared to sowing seeds in a 3D field. To harvest the best crop possible, one needs to optimize the following four critical components:
The seeds (e.g., the graft, its quality, viability, stem cell content)
The planting method (e.g., the surgical technique of diffusely, evenly, and atraumatically sowing to avoid clumps)
The field (e.g., the recipient tissue, its size, its vascularity, the presence or absence of growth-promoting factors)
The nurturing postplanting (e.g., postoperative care, immobilization, stimulation of growth)
It does not matter whether three of these components are maximally optimized; if one component is poor, the yield will be poor. It is the least optimized of these four components, the bottleneck factor, that becomes rate limiting and determines the overall result. To illustrate this, consider that poor seeds planted in a large, fertile field will not yield much, and, conversely, excellent seeds squeezed and crowded in a small, rocky soil will not yield much either. Moreover, while the best possible seeds poorly planted in the best fertile soil will yield a poor crop, even the best seeds optimally planted in the best fertile soil will not yield a good crop if after planting the soil is stirred or the field is left to dry out.
Some surgeons have shown acceptable results using a variety of fat harvesting and preparation methods, some often diametrically opposite to each other. This is because methods of fat harvest and preparation are not bottleneck rate-limiting factors in large-volume fat grafting. Our experience points to the fact that the major limiting factor in large-volume fat grafting is the recipient site, not management of the graft material.
Managing Theory and Science in Fat Grafting
As surgeons seeking to optimize the results of autologous fat grafting, we have to manage the technical variables over which we have some degree of control:
Donor material: fat harvesting and fat processing
Fat grafting technique: mapping technique and reverse liposuction technique
Recipient-site management: pregraft and postgraft
Donor Material
Fat Harvesting
Harvesting: Role of the Cannula.
Using smaller cannula sizes during harvesting creates less donor-site trauma and allows for removal of smaller lobules of fat, which may improve flow characteristics during reinjection. However, the smaller the cannula size, the slower is the fat removal process, and for fat-grafting breast augmentation to be a viable technique, one must be conscious of operative time. For the procedure to gain adoption in breast augmentation, for example, it must be performed in 2 hours or less. These opposing incentives—harvesting time and quality of donor graft—represent one pair of several diametrically opposed variables in fat grafting.
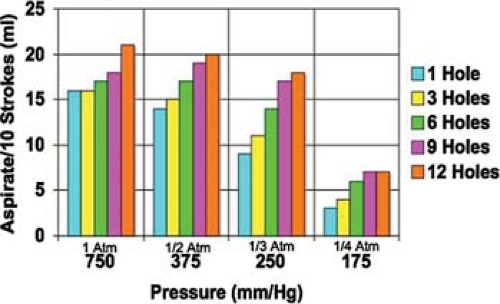
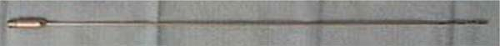
As important as cannula size are cannula hole size and number of holes. We have studied the effect of varying the number of side holes on the efficiency of liposuction and confirmed the intuitive assumption that the larger the number of side holes, the more efficient is the liposuction at less traumatic pressures (Fig. 118.2). A 12-gauge (2.7-mm-diameter) cannula with 9 to 12 side holes of size 2 × 1 mm can extract a significant amount of fat despite its small caliber.
Harvesting: Role of Suction Negative Pressure.
Although it is not well documented, some studies demonstrate that the lower the absolute value of the negative pressure used at harvest, the better is the graft viability (22). However, studies
that use clinical volume maintenance as endpoints may not be as accurate as those using adipocyte integrity immediately postharvest. Until this is studied in a well-controlled setting with quantitative data, it is best to assume that the lower the absolute value of the negative pressure needed to obtain the graft, the less is the trauma to the adipocyte. Figure 118.3 shows that our choice of a 12-hole cannula set at 1/3 atm (250 mm Hg) is a more efficient harvesting instrument than a single-hole cannula operating at 1 atm.
that use clinical volume maintenance as endpoints may not be as accurate as those using adipocyte integrity immediately postharvest. Until this is studied in a well-controlled setting with quantitative data, it is best to assume that the lower the absolute value of the negative pressure needed to obtain the graft, the less is the trauma to the adipocyte. Figure 118.3 shows that our choice of a 12-hole cannula set at 1/3 atm (250 mm Hg) is a more efficient harvesting instrument than a single-hole cannula operating at 1 atm.
Harvesting: Syringe Versus Liposuction Aspirator.
Harvesting the fat for grafting can be accomplished at the recommended low pressures either with a mechanical liposuction aspirator vacuum source or with a handheld syringe. Mechanical aspiration is more efficient, but it presents potential problems. The fat collection reservoir needs to be in series with the vacuum source and has to remain vertical, lest the collected fat continues toward the pump. The reservoir also has to be rigid to stay open and hold the vacuum, and it also has to remain sterile (Fig. 118.4.)
This arrangement requires long connection tubes that generate potential dead space losses. At every instance of vacuum loss, whenever one of the holes of the liposuction cannula comes close to the surface, air can flow through the tubing to desiccate the adipocytes trapped in the long tubing, and the air gush splashes the collection bottle. We found this to be more difficult in patients with low body mass index who only have small amounts of fat.
The concern over air exposure is not well quantified. It has been reported in one communication that greater than 50% of adipocytes undergo cytoplasmic lysis on exposure to air (23). This potential concern led us to develop a two-way tissue routing valve that separates the syringe vacuum source from the collection receptacle and directs the aspirate toward a collection bag when the syringe is full (Fig. 118.5.)
Harvesting: Graft Harvest Site.
Although it has been suggested that there are specific donor areas that allow for a higher survival of fat grafting, we, like others (24), have not found the anatomic location of the donor site to be of significance to outcomes. It may turn out that that adipocyte cellular size, which varies in different body regions and also among different patients, may be the more important variable. Larger cells have a higher likelihood of mechanical cell membrane damage during extraction, and it may be this variable of cell size relative to cannula hole size that is more important than the area on the body used for harvest per se.
Fat Processing
Air Exposure During Processing.
As stated earlier, a variable of unknown weight in fat harvesting and processing remains the negative impact of air exposure (23). Fat concentration techniques range from drying the fat on Telfa rolls (high air exposure, high likelihood of cell damage and contamination), to completely closed systems that keep the fat inside intravenous (IV) tubing, two-way routing valves, and IV bags. Washing harvested graft with saline-buffered solutions and adding growth factors or cell preservatives (25) has been described and may show promise in the future. We believe that there are already many potential factors (stem cells, growth factors) in the lipoaspirate that should be preserved in the graft. This is one of the reasons we do not favor washing or filtration and prefer not to completely remove fluid by high-speed centrifugation.
Role of Stem Cell–Enriched Graft.
Concentrating adipocyte stem cells and remixing them with mature adipocytes to increase cell viability has been described (26). The theoretical benefit of a stem cell–enriched graft is that the smaller stem cells improve volume yield. The smaller graft volumes will differentiate and grow into larger mature adipocytes to yield a larger augmentation. Although this may be an effective strategy in the future, this technique is not proven, nor is it approved by the Food and Drug Administration, and we do not employ it.
The Fallacy of “Percentage Yields”.
One of the most confusing metrics in fat grafting is a lack of standardization regarding “percentage yields.” Once fat is lipoaspirated as donor graft
there is an infinite number of different concentrations of fat relative to crystalloid that can be reached prior to grafting the recipient site. Unless we know this percentage, or “fatocrit,” we can never really know what percentage of fat survived grafting. Another reason is there is no standardization regarding how to measure percentage yields. Are we measuring percentage volume retention? Are we measuring percentage increase in volume of the recipient site? Are we measuring the actual proportion of grafted cells that survived? Recent animal models may help to standardize attempts at cellular percentage survival (27) and may help to describe methods to better quantify volume retention pre and post grafting. We believe that careful documentation of the following should be done in fat-grafting patients, in order to better understand the yield in each case:
there is an infinite number of different concentrations of fat relative to crystalloid that can be reached prior to grafting the recipient site. Unless we know this percentage, or “fatocrit,” we can never really know what percentage of fat survived grafting. Another reason is there is no standardization regarding how to measure percentage yields. Are we measuring percentage volume retention? Are we measuring percentage increase in volume of the recipient site? Are we measuring the actual proportion of grafted cells that survived? Recent animal models may help to standardize attempts at cellular percentage survival (27) and may help to describe methods to better quantify volume retention pre and post grafting. We believe that careful documentation of the following should be done in fat-grafting patients, in order to better understand the yield in each case:
Document the preexpansion volume of the breast (MRI, 3D imaging, or both).
Document the method of crystalloid separation (double decanting, low-speed centrifugation, high-speed centrifugation).
Document the volume of material grafted.
Document the postgraft volume of the breast at 6 months or more (MRI, 3D imaging, or both).
High-Speed Centrifugation.
Centrifuging the lipoaspirate at 1,000 × g for 3 minutes is the method of fat processing that had been popularized as a strategy for effective fat grafting. Historically, the penchant for centrifugation arose from the need to graft as much adipocyte biomass as possible into a limited space. Although centrifugation can yield highly concentrated fat, there are four potential problems with centrifugation (Fig. 118.6):
The cells may be damaged with high g-forces, although studies have shown that the standard centrifugation protocol has no significant deleterious effect on survival.
It is a time- and labor-consuming process and one that exposes the graft to potential contamination.
High fat concentrations may cause clumping and more difficult flow during reinjection.
Clumped cells have less-than-optimal graft-to-recipient interface and thus lower engraftment potential for the individual cells at the center of the clump.
Low–G-Force Centrifugation.
Use of the BRAVA system of preexpansion of the recipient site has emancipated fat grafting from the need for centrifugation and its potential disadvantages. The BRAVA-expanded breast has the advantage of space and thus reduces the deleterious effect of crowding. In the expanded space, a larger amount of loose fat slurry can be more diffusely dispersed and survive better. Through use of an external centrifuge with bags in the closed technique (Fig. 118.7), fat cells are still separated from crystalloid with little trauma at 1.5 to 2 × g.
The “Double-Decanting” Technique: “One G” of Separation.
If effective preexpansion of the recipient site can generate a hyperexpanded recipient parenchymal space, it means that the more expanded the breast is, the less concentrated does the harvested adipocytes need to be. At some expansion volume, there may be no need to centrifuge the fat. Simply decanting the crystalloid off in the collection canister (step 1) and then transferring the decanted fat into a 60-cc syringe (step 2) can process fat at a suitable concentration for grafting (Fig. 118.8) This is called the “double-decanting” technique.
Fat Grafting Technique
There are two popular methods of fat grafting: the “mapping” technique and the “reverse liposuction” technique. There is no
strong data to prove which technique is better or yields better results. As stated earlier, the overall technique must take into consideration the relative time and manpower demands of each variable discussed to render an “optimized” operation, not a “maximized” variable per se.
strong data to prove which technique is better or yields better results. As stated earlier, the overall technique must take into consideration the relative time and manpower demands of each variable discussed to render an “optimized” operation, not a “maximized” variable per se.
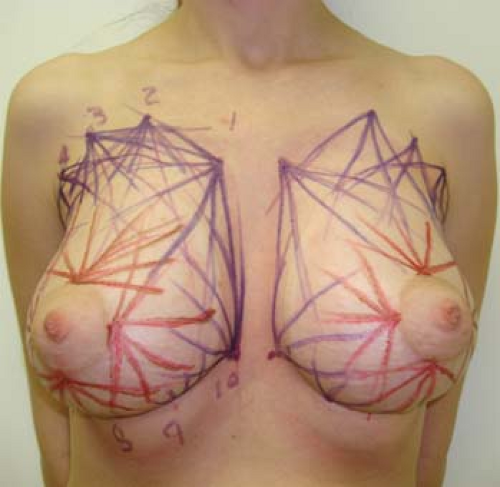
The Mapping Technique.
Donor cells have the highest chance of survival with the technique that best ensures an even, three-dimensional dispersion of the fat. The higher the surface-to-volume contact with the recipient-site tissue for each fat lobule transplanted, the higher is the likelihood of sufficient oxygen diffusion and survival of the graft. The mapping technique involves the use of small (3 to 5 cc) syringes handheld and connected directly to a 14-gauge blunt side-hole cannula. Markings are made in the recipient areas to aid in a systematic, diffuse, and even injection of the entire recipient. From 8 to 10 circummammary and 4 circumareolar entry points are usually made with a 14-gauge hypodermic needle. Through each entry point the 15- to 20-cm-long cannula makes multiple tunnels that fan out radially and inject 2 to 3 cc of fat upon withdrawal. The cannula is then inserted into another adjacent entry point, and the process is repeated to yield a 3D weave that evenly criss-cross covers the recipient space (Fig. 118.9). Multiple levels of graft are deposited, deep from the base of the breast just above the pectoralis fascia, to the subcutaneous space immediately subjacent to the dermis. Direct injection of fat into the dense parenchyma of the breast is never performed. This technique is deliberate and exact but does take time. In addition, it requires the operator to deploy the plunger and withdraw the needle at the same time.
Reverse Liposuction Technique.
The reverse liposuction technique uses three to five insertions on the breast, two or three in the inframammary fold (IMF), and several laterally and toward the axilla. The IMF insertions are made below the native IMF, as this will descend 1 to 2 cm, similar to the effect seen in augmentation with breast prostheses. The “décolletage” or “social” part of the breast is avoided in the event hyperpigmentation of the needle sites occurs. With a 15- to 20-cm side-hole, 14-gauge needle loaded directly onto 60-cc syringes, the fat is injected using a controlled and deliberate liposuction movement of the plunger along a fanning pattern of vectors at
multiple planar levels from the base of the breast. The axillary insertion is also used to place the graft in the submuscular position. The rate of insertion in this technique should be 2 to 4 seconds per cc, which results in a rate of 2 to 3 minutes/60 cc of fat, or a grafting session of 300 cc per breast performed in 10 to 15 minutes on each breast.
multiple planar levels from the base of the breast. The axillary insertion is also used to place the graft in the submuscular position. The rate of insertion in this technique should be 2 to 4 seconds per cc, which results in a rate of 2 to 3 minutes/60 cc of fat, or a grafting session of 300 cc per breast performed in 10 to 15 minutes on each breast.
An example of optimizing a technique versus maximizing a variable, the reverse liposuction technique strives to reduce grafting time and the number of insertion sites. There is a higher potential for less diversified dispersion if this technique is not effectively performed. Another potential benefit of the reverse liposuction technique is that 60-cc syringes used from double decanting can be immediately loaded, decreasing fat handling. The 60-cc syringes generate lower maximum pressures than do 5-cc syringes, which are used in other techniques. Therefore, if there is a blockage of flow along the insertion needle due to clumping, this will occur at a lower pressure level using a 60-cc syringe, with less potential damage to the grafted cells.
A summary of the three commonly used techniques is outlined in Table 118.2.
Recipient-Site Management
No other variable in fat grafting has been less studied or appreciated than the recipient site. To better appreciate the role of the recipient site in fat grafting, consider the history of fat grafting compared to those of skin grafting. Descriptions in Sanskrit indicate that small skin grafts were employed in India by 3000 BC (28). Eventually, improvements in instrumentation afforded more uniform donor thicknesses. Only during the last 60 or so years have more advanced wound care, debridement, antibiotics, and methods of graft immobilization helped to improve graft take. In recent years the introduction of vacuum-assisted closure (VAC) has further revolutionized skin grafting by a variety of postulated effects, including bacterial clearance, neovascularization, and reduction in edema of the wound bed. When we consider the recent introduction of fat grafting relative to skin grafting, it is clear that we have just begun. Recipient-site management has only recently been suggested as an important variable in fat grafting that could be potentially manipulated and improved. The size, vascularity, and pressure compliance of the recipient site are the most prominent components.
Table 118.2 | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Recipient-Site Size.
In the familiar 2D skin grafting of wounds, the surface of the wound determines the upper limit of skin graft that survives, and overgrafting more skin does not help. Similarly, in 3D grafting, the volume of the recipient bed sets the maximal limit to the volume of graft that can survive, and overgrafting with more fat will lead to necrosis and oil cysts.
We devised a geometric model of 3D grafting of tissue droplets that assumes the following:
Evenly diversified 3D dispersion of the grafted droplets
A similar size range for graft droplets and recipient stromal cells
Preservation of the recipient matrix 3D vascular stromal interconnections
Infinite compliance of the recipient stroma as it is stretched to accommodate the graft droplets
This model suggests that even with the most perfect technique and the most even graft distribution, graft volume cannot exceed two thirds of the recipient volume. Filling above this limit will lead to overcrowding, and by worsening the graft-to-recipient contact and the diffusion gradient, drastically decrease cell survival.
Using the previously described “seeds in a field” analogy, the size of the field, not the number of seeds, ultimately sets the upper limit of the crop size. “Overcorrection” or overgrafting is definitely counterproductive; the reasonable approach is to try to match the graft volume to the recipient volume. With the understanding that we can modulate the recipient site in fat grafting, the overcorrection and overgrafting of yesterday become the overexpansion of today.
This opens up an opportunity for positive intervention. For megavolume grafting in a tight space, temporary expansion of the recipient loosens the extracellular matrix and creates many more interstices where many more individual fat droplets can optimize their graft to recipient interface and survive (see Fig. 118.10).
Recipient-Site Vascularity.
It is well established that muscle tissue with its high capillary density is an excellent graft recipient, and that the more vascular the recipient, the better is the graft survival (29,30).
Furthermore, a number of cytokines and growth factors can accelerate the process of graft angiogenesis and improve survival. Future attempts at priming the recipient site by increasing its vascularity and endogenously stimulating angiogenic cytokine production may potentially improve engraftment.
Recipient-Site Filling Pressure.
From the general surgery trauma literature and from consideration of hand and upper extremity trauma, the importance of compartment pressure and the grave consequences of high interstitial pressure are well understood. If it were possible to preexpand the recipient space prior to fat grafting, it would make it more compliant and allow the injection of larger volumes of graft into the recipient site before reaching physiologically excessive interstitial pressures.
Recipient-Site Modulation: Brava External Breast Expansion
The BRAVA bra was initially developed in the 1990s as an external soft tissue expander to enlarge the breast. The device consists of a pair of semirigid domes with silicone gel rim cushion that interfaces with the skin and that are worn around the breasts like a bra. A small battery-operated “sport” pump maintains a low negative pressure inside the domes that does not interrupt capillary flow and imparts on the breast surface a constant gentle isotropic distraction force (Fig. 118.11). Studies have shown that when the device is worn in an uninterrupted fashion for 10 to 12 hours/day, true and long-lasting breast augmentation ensues over a period of weeks to months (31,32,33,34,35).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree