The Short Scar Periareolar Inferior Pedicle Reduction Mammaplasty
Dennis C. Hammond
Introduction
Since the mid-1960s, the Wise pattern inferior pedicle reduction technique has been, in one variation or another, the preferred technique for breast reduction for most surgeons across North America and around the world. However, more recent interest in reduced or “short” scar techniques has prompted plastic surgeons to more carefully evaluate other approaches. This interest stems not so much from dissatisfaction with the standard inferior pedicle approach, but rather from a desire to reduce the complications associated with the procedure. In particular, techniques to reduce the amount of cutaneous scar and provide for more aesthetic and long-lasting shapes have been actively investigated. This chapter describes one such approach called the short scar periareolar inferior pedicle reduction (SPAIR) mammaplasty (1,2,3,4).
Operative Strategy
In designing this approach, every effort was made to geometrically design a pattern for skin envelope reduction that would limit the scar to the central portion of the breast using a circumvertical strategy to eliminate the wide inframammary scar. Because of the general familiarity with the inferior pedicle approach, this type of pedicle is used to preserve the neurovascular supply to the breast parenchyma and nipple-areola complex (NAC). Finally, internal shaping sutures are used to more effectively reposition the remaining breast tissue to create aesthetic breast shapes that can be evaluated directly at the time of surgery, rather than waiting for time to result in breast shape change with settling. By combining these operative steps, a versatile, consistent, and reliable technique for breast reduction is developed that is applicable to a wide variety of patients.
Patient Marking
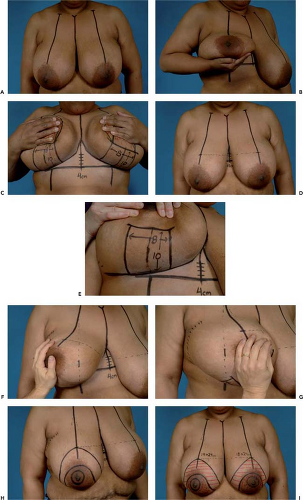
The goal of the marking procedure is to estimate how much of the skin envelope must be retained around the periphery of the breast to comfortably wrap around the inferior pedicle once the excess parenchyma has been resected. With this in mind, four cardinal points are identified using existing breast landmarks. The patient is marked in the upright position. The midsternal line and the inframammary fold are identified, and the breast meridian is then drawn on each side (Figs. 92.1A and 92.1B). This meridian line bisects the breast into two equal volumetric halves and extends from the anterior portion of the breast over and around onto the chest wall. It is important to note that, in some instances, this line will not run through the nipple if the nipple is displaced off the midline of the breast either medially or laterally. The inframammary fold under each breast is joined with a line that extends across the front of the patient (Fig. 92.1C). This allows the location of the fold to be identified with the breasts in their natural orientation. The first cardinal point represents the proposed position of the superior portion of the areola. This point is based on the position of the existing fold. By measuring up from the inframammary fold in the midline 3 to 5 cm, the top portion of the pattern on each side is identified. A line parallel to the inframammary fold line is drawn across the breast (Fig. 92.1D). Where the breast meridian crosses this line represents the topmost portion of the periareolar pattern. The second cardinal point identifies the inferior portion of the pattern. This is a measured landmark based on the breast meridian. The meridian is identified at the level of the inframammary fold, and an 8-cm wide pedicle is drawn and centered on the breast meridian. On either side of the pedicle, a line is drawn up onto the breast parallel with the breast meridian. The length of this line measures 8 cm in smaller breasts, with proposed reduction amounts of 500 g or less, and 10 cm in larger breasts with proposed reduction amounts of 1,000 g or more. The tops of these two lines are then joined in a curvilinear line that parallels the inframammary fold (Fig. 92.1E). This represents the inferior segment of skin that will be preserved after parenchymal resection. The third and fourth cardinal points represent the medial and lateral portions of the periareolar pattern, respectively. These two points are identified by using the hand to elevate and slightly rotate the breast first up and out (Fig. 92.1F), then up and in (Fig. 92.1G), and then transposing visually the breast meridian onto the breast at a point level with the nipple. The goal inherent in manipulating the breast in this way is to try to mold the breast into the desired postoperative shape, and then use the breast meridian to identify the proper position of the medial and lateral resection margin to allow easy redraping of the medial and lateral skin segments around the inferior pedicle. Once these four cardinal points have been identified, they are joined in a curvilinear pattern that assumes the shape of an elongated oval (Fig. 92.1H). A proposed areolar diameter of approximately 5 cm is diagrammed and the pedicle is drawn in, skirting the top of the areolar margin by a distance of 2 to 3 cm. The segment of skin to be removed with the parenchyma is marked with horizontal lines, and the skin of the inferior pedicle that will be de-epithelialized is marked with dots (Fig. 92.1I). It is helpful to measure the dimensions of the proposed periareolar pattern at this point, both in the transverse and longitudinal dimensions. Experience has shown that when either of these measurements is less than 15 cm, there is little difficulty in managing the skin envelope during the skin redraping portion of the procedure. For measurements of 15 to 20 cm, some experience in using the circumvertical concept is helpful. For
measurements of more than 20 cm, experience with the technique is recommended to achieve the best result.
measurements of more than 20 cm, experience with the technique is recommended to achieve the best result.
Operative Technique
At surgery, the patient must be prepared for being elevated to the sitting position during the procedure. This maneuver is mandatory to allow assessment of breast shape during skin redraping. Therefore, the arms must be secured to arm boards and the head supported on a foam headrest. Anesthesia must be informed of the need to sit the patient up during surgery to allow for adequate hydration and avoidance of postural hypotension.
All proposed incisions are infiltrated with a dilute solution of lidocaine with epinephrine. A breast tourniquet is applied, and the areola is placed under maximal stretch. A 52-mm diameter areolar mark is made with a circular template (Figs. 92.2A and 92.2B). Ultimately, the periareolar purse-string suture will be tied down to approximately 40 mm in diameter; thus, the larger areola will eventually be allowed to simply rest in the areolar opening without tension. This strategy allows a more natural-looking and tension-free areola to be created. All incisions are scored, and the inferior pedicle within the periareolar pattern is de-epithelialized, along with a rim of dermis around the periphery (Figs. 92.2C and 92.2D). This rim is de-epithelialized for a width of approximately 1 cm, and the dermis divided with Bovie cautery in such a way that a 5-mm dermal rim is created around the periareolar pattern except for the 8 cm width of the inferior pedicle. This rim of dermis will ultimately serve as a sturdy architectural dermal framework into which the periareolar purse-string suture will be placed. The dermis around the inferior pedicle is likewise divided and the tourniquet released. Medial, superior, and lateral flaps are then developed with three-dimensional sculpting of the breast in mind. The medial and superior flaps are initially dissected directly at the dermal level, with dissection then curving gently downward to create a flap that becomes progressively thicker until the chest wall is reached. At the base of the flap, the thickness of fat and parenchyma measures 4 to 6 cm. Laterally, there is a tendency for the breast to assume a “boxy” appearance if the flap is kept too thick; therefore, initial flap dissection again begins just under the dermis and then angles toward the capsule of the breast. The remainder of the lateral flap is dissected at this level down to the lateral border of the breast. Where the lateral and superior flaps merge, a smooth transition is made from the thicker base of the superior flap to the thinner base of the lateral flap. It is important to emphasize that dissection of the flaps does not violate the
inframammary fold. In the medial and lateral corners of the breast flap dissection, the attachments of Scarpa’s fascia to the underside of the breast are preserved. By keeping these relationships intact, the postoperative phenomenon of “bottoming out” or migration of breast parenchyma below the inframammary fold is prevented. The result is a stable breast shape postoperatively and greater control over the operative result. After the flaps have been created, the bulk of the remaining breast can be delivered from the wound, and the general contours created by the flaps can be seen (Figs. 92.3A and 92.3B). Specifically, the superior and medial contours of the breast should be smooth and full to avoid any sharp step-offs in breast shape. The pedicle is now skeletonized, making sure to avoid any undermining of the NAC (Figs. 92.3C and 92.3D). The longitudinal septum of the breast can usually be identified in the lower half of the breast during this dissection. This septum carries important perforators and should not be incised during pedicle dissection (5,6). The specimen that is removed comes off in the shape of a horseshoe with the lateral limb slightly longer than the medial limb (Fig. 92.3E). It is important to carefully create the flaps and pedicle such that, after pedicle skeletonization, the flaps and pedicle wrap around each other smoothly. This creates a pleasing breast shape and avoids any sharp or unaesthetic contours. In patients with a naturally full upper pole to the breast, no further shaping maneuvers are required, and the procedure simply continues. If, however, there is hollowness in the upper pole of the breast, reshaping with internal sutures is required. This simply involves undermining the remaining breast parenchyma in the superior pole of the breast and advancing this flap superiorly until the desired upper pole fullness is created (Figs. 92.4A–C). At this point, the underside of the flap is sutured down to the pectoralis fascia with one or two absorbable sutures to perform what is essentially an “autoaugmentation” of the upper pole of the breast (Fig. 92.4D). Usually, the leading edge of the undermined superior breast flap is relocated superiorly 4 to 6 cm. This maneuver is made possible by making the superior flap thick enough at the base during the initial flap dissection. When necessary, medial reshaping is also performed by undermining the base of the medial flap up to the level of the intercostal perforators (Fig. 92.4E) and then simply plicating the leading edge of this flap to itself to gather the medial tissues together to create a more rounded contour (Figs. 92.4F–H). Finally, the tendency for the inferior pedicle to fall off laterally into the axilla is counteracted by suturing the base of the
pedicle down to the pectoralis fascia in the central portion of the breast (Fig. 92.4I). This centralizes the bulk of the breast tissue and assists in shaping the breast. After the breast shape has been controlled, the vertical skin incision is determined. By placing traction on the inferior pedicle, the medial and lateral breast flaps will buckle. These two buckle points are joined together with a skin stapler to position the “key staple” (Figs. 92.5A–D). This then sets the rest of the pattern. Two hemostats are used to grasp the previously de-epithelialized dermal shelf right at the key staple point, and upward traction is placed on the inferior skin envelope (Fig. 92.5E). This maneuver allows the redundant inferior skin envelope of the breast to be plicated together with staples until a smooth, rounded contour is created (Figs. 92.5F–J). The NAC is also inset with staples to complete the proposed closure (Fig. 92.5K). Adjustments are often required at this point to either tighten the skin further or loosen
the plication in selected areas to create the desired shape. It is sometimes helpful to perform this plication with the patient upright as an aid to effective shaping. After the desired shape has been created, the edges of the staple line are marked with a skin marker, and all the staples are removed (Fig. 92.5L). The area of the inferior pedicle is identified, and a small medial wedge and a larger lateral wedge of redundant skin and parenchyma are noted (Fig. 92.5M). The inferior pedicle is de-epithelialized, and the medial and lateral wedges of tissue are removed (Fig. 92.5N). In this fashion, the lateral breast flap, because it is completely incised, can be brought over to the medial breast flap on top of the de-epthelialized pedicle without tension or kinking (Fig. 92.5O). This aids in the creation of a smooth rounded inferior breast contour. Drains are placed in larger reductions of more than 700 to 800 g and are brought out laterally along the inframammary fold. The vertical incision is then closed with 4–0 absorbable monofilament, using both interrupted inverted dermal sutures and finally a running subcuticular suture (Fig. 92.5P). The dimension of the periareolar opening will be noted to be much smaller as a result of adding the vertical component to the skin pattern; however, there will still be a discrepancy between the larger diameter of the periareolar incision and the smaller diameter of the areolar incision. This discrepancy is managed by placing a purse-string suture in the periareolar dermal shelf created during the initial incision pattern (Figs. 92.6A and 92.6B). It is highly recommended that a CV-3 Gortex suture is used for this purpose. The handling characteristics of this material are ideal in that this suture material is strong, permanent, and, most important, slides easily through the dermis. This allows the purse-string suture to be closed with a great deal of control and to any desired dimension. The knot for the suture is placed so as to bury it under the edge of the dermal shelf to avoid postoperative erosion through the suture line. The suture is drawn down to create an opening of approximately 40 mm (Figs. 92.6C and 92.6D). After being secured, the patient is placed upright, and the opening is often observed to be irregular and oval shaped along an axis running from superomedial to inferolateral. By drawing a circular pattern centered on this opening and then de-epithelializing this additional skin, a perfectly circular areolar defect can be created (Figs. 92.6E–G). Care must be taken to avoid inadvertently cutting the Gortex purse string suture during this process. The areola is then inset
into the defect again with 4–0 absorbable monofilament suture (Figs. 92.6H and 92.6I). To prevent postoperative asymmetry, it is advised to perform the various steps of the operation sequentially from side to side. This gives maximum control over the volume and shape of each breast and allows proper adjustments to be made as needed. If one breast is completed first, it may become difficult to obtain absolute symmetry in the other, particularly if the second breast then ends up lacking volume compared with the first. After the procedure is fully completed, our preference is to cover the incisions with Dermabond and Opsite. A support garment is then applied.
inframammary fold. In the medial and lateral corners of the breast flap dissection, the attachments of Scarpa’s fascia to the underside of the breast are preserved. By keeping these relationships intact, the postoperative phenomenon of “bottoming out” or migration of breast parenchyma below the inframammary fold is prevented. The result is a stable breast shape postoperatively and greater control over the operative result. After the flaps have been created, the bulk of the remaining breast can be delivered from the wound, and the general contours created by the flaps can be seen (Figs. 92.3A and 92.3B). Specifically, the superior and medial contours of the breast should be smooth and full to avoid any sharp step-offs in breast shape. The pedicle is now skeletonized, making sure to avoid any undermining of the NAC (Figs. 92.3C and 92.3D). The longitudinal septum of the breast can usually be identified in the lower half of the breast during this dissection. This septum carries important perforators and should not be incised during pedicle dissection (5,6). The specimen that is removed comes off in the shape of a horseshoe with the lateral limb slightly longer than the medial limb (Fig. 92.3E). It is important to carefully create the flaps and pedicle such that, after pedicle skeletonization, the flaps and pedicle wrap around each other smoothly. This creates a pleasing breast shape and avoids any sharp or unaesthetic contours. In patients with a naturally full upper pole to the breast, no further shaping maneuvers are required, and the procedure simply continues. If, however, there is hollowness in the upper pole of the breast, reshaping with internal sutures is required. This simply involves undermining the remaining breast parenchyma in the superior pole of the breast and advancing this flap superiorly until the desired upper pole fullness is created (Figs. 92.4A–C). At this point, the underside of the flap is sutured down to the pectoralis fascia with one or two absorbable sutures to perform what is essentially an “autoaugmentation” of the upper pole of the breast (Fig. 92.4D). Usually, the leading edge of the undermined superior breast flap is relocated superiorly 4 to 6 cm. This maneuver is made possible by making the superior flap thick enough at the base during the initial flap dissection. When necessary, medial reshaping is also performed by undermining the base of the medial flap up to the level of the intercostal perforators (Fig. 92.4E) and then simply plicating the leading edge of this flap to itself to gather the medial tissues together to create a more rounded contour (Figs. 92.4F–H). Finally, the tendency for the inferior pedicle to fall off laterally into the axilla is counteracted by suturing the base of the
pedicle down to the pectoralis fascia in the central portion of the breast (Fig. 92.4I). This centralizes the bulk of the breast tissue and assists in shaping the breast. After the breast shape has been controlled, the vertical skin incision is determined. By placing traction on the inferior pedicle, the medial and lateral breast flaps will buckle. These two buckle points are joined together with a skin stapler to position the “key staple” (Figs. 92.5A–D). This then sets the rest of the pattern. Two hemostats are used to grasp the previously de-epithelialized dermal shelf right at the key staple point, and upward traction is placed on the inferior skin envelope (Fig. 92.5E). This maneuver allows the redundant inferior skin envelope of the breast to be plicated together with staples until a smooth, rounded contour is created (Figs. 92.5F–J). The NAC is also inset with staples to complete the proposed closure (Fig. 92.5K). Adjustments are often required at this point to either tighten the skin further or loosen
the plication in selected areas to create the desired shape. It is sometimes helpful to perform this plication with the patient upright as an aid to effective shaping. After the desired shape has been created, the edges of the staple line are marked with a skin marker, and all the staples are removed (Fig. 92.5L). The area of the inferior pedicle is identified, and a small medial wedge and a larger lateral wedge of redundant skin and parenchyma are noted (Fig. 92.5M). The inferior pedicle is de-epithelialized, and the medial and lateral wedges of tissue are removed (Fig. 92.5N). In this fashion, the lateral breast flap, because it is completely incised, can be brought over to the medial breast flap on top of the de-epthelialized pedicle without tension or kinking (Fig. 92.5O). This aids in the creation of a smooth rounded inferior breast contour. Drains are placed in larger reductions of more than 700 to 800 g and are brought out laterally along the inframammary fold. The vertical incision is then closed with 4–0 absorbable monofilament, using both interrupted inverted dermal sutures and finally a running subcuticular suture (Fig. 92.5P). The dimension of the periareolar opening will be noted to be much smaller as a result of adding the vertical component to the skin pattern; however, there will still be a discrepancy between the larger diameter of the periareolar incision and the smaller diameter of the areolar incision. This discrepancy is managed by placing a purse-string suture in the periareolar dermal shelf created during the initial incision pattern (Figs. 92.6A and 92.6B). It is highly recommended that a CV-3 Gortex suture is used for this purpose. The handling characteristics of this material are ideal in that this suture material is strong, permanent, and, most important, slides easily through the dermis. This allows the purse-string suture to be closed with a great deal of control and to any desired dimension. The knot for the suture is placed so as to bury it under the edge of the dermal shelf to avoid postoperative erosion through the suture line. The suture is drawn down to create an opening of approximately 40 mm (Figs. 92.6C and 92.6D). After being secured, the patient is placed upright, and the opening is often observed to be irregular and oval shaped along an axis running from superomedial to inferolateral. By drawing a circular pattern centered on this opening and then de-epithelializing this additional skin, a perfectly circular areolar defect can be created (Figs. 92.6E–G). Care must be taken to avoid inadvertently cutting the Gortex purse string suture during this process. The areola is then inset
into the defect again with 4–0 absorbable monofilament suture (Figs. 92.6H and 92.6I). To prevent postoperative asymmetry, it is advised to perform the various steps of the operation sequentially from side to side. This gives maximum control over the volume and shape of each breast and allows proper adjustments to be made as needed. If one breast is completed first, it may become difficult to obtain absolute symmetry in the other, particularly if the second breast then ends up lacking volume compared with the first. After the procedure is fully completed, our preference is to cover the incisions with Dermabond and Opsite. A support garment is then applied.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree