CHAPTER 53 Breast augmentation
Physical evaluation
Anatomy
These structures receive their blood supply via the lateral thoracic and internal thoracic arteries by means of the intercostal perforators. These vessels, in turn, converge to form a dense subdermal vascular plexus, which supplies the skin. The nipple and areola are innervated predominately by the 4th intercostal nerve, as well as the 3rd and 5th, to some extent, by way of the anterolateral and anteromedial cutaneous branches.
Technical steps
Placement
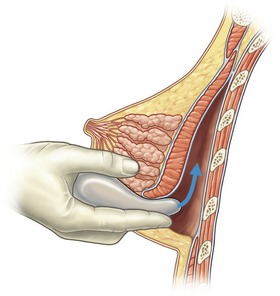
The breast pocket may be created in either the subglandular or subpectoral space (Fig. 53.1). The subglandular technique is usually reserved for patients who have substantial breast tissue or a mild degree of ptosis, since greater projection may be obtained. Also, women who are avid bodybuilders may prefer subglandular implants for the reason that placing them submuscularly, in some instances, may produce breast animation and distortion when the pectoral muscles are flexed. Increased risks of capsular contracture, rippling and implant palpability are typically issues discouraging the routine use of the subglandular plane.
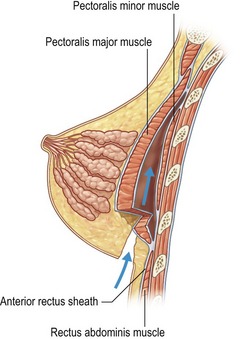
In patients with a paucity of breast tissue and little to no ptosis, the subpectoral technique, in our opinion, produces optimum results. The pectoralis major drapes the superomedial aspect of the prosthesis, softening the transition, and thus creating a more anatomically shaped breast mound (Fig. 53.2). This method also achieves a natural feel, which is especially desirable when using saline implants. The submuscular plane additionally tends to be less vascular, and is associated with fewer sensory alterations of the nipple areolar complex. Also, rates of fibrous capsular contracture are demonstrably lowered with submuscular placement versus subglandular. In addition to improved aesthetic outcomes, there are moreover prospective functional advantages in regard to breast-feeding as well as cancer screening.
Surgical approach
Although numerous methods have been described in the literature, there are three preferred approaches for breast augmentation: inframammary, periareolar and transaxillary (Fig. 53.3). Dissections may be performed in either plane, with or without the aid of an endoscope.
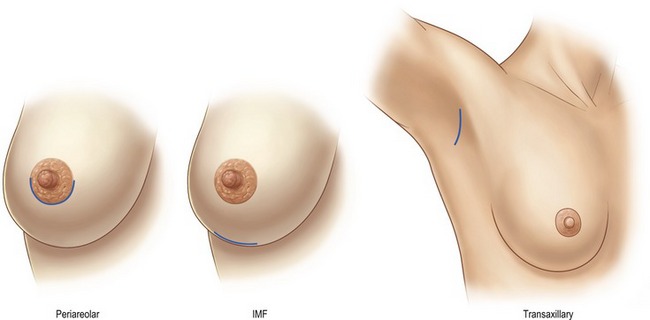
Fig. 53.3 Incision sites: Examples of periareolar, inframammary crease, and transaxillary incision sites are shown. Note how all heal well with proper placement and patient selection given individual breast anatomy. (This figure incorporates images from Figs 53.5, 53.7 and 53.10.)
The inframammary fold incision (Fig. 53.4) provides excellent results in terms of inconspicuous scars, accessibility for both implant types, and fold modifications (Fig. 53.5). This incision allows for optimal view of the pectoral muscle and breast parenchyma, which permits the surgeon to perform an accurate dissection in either, the submuscular or subglandular plane. The downsides of this approach are the potential increased risk of iatrogenic rupture during wound reapproximation, and implant exposure during the postoperative period given the weight of the implant on the healing incision. Additionally, the access incision must be carefully designed to avoid scar migration to the chest wall or inferior pole of the breast.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


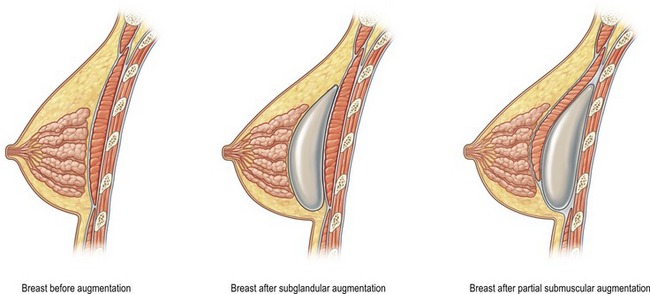
 of the implant is covered by breast gland and fascia, and the top
of the implant is covered by breast gland and fascia, and the top  by pectoralis major muscle.
by pectoralis major muscle.