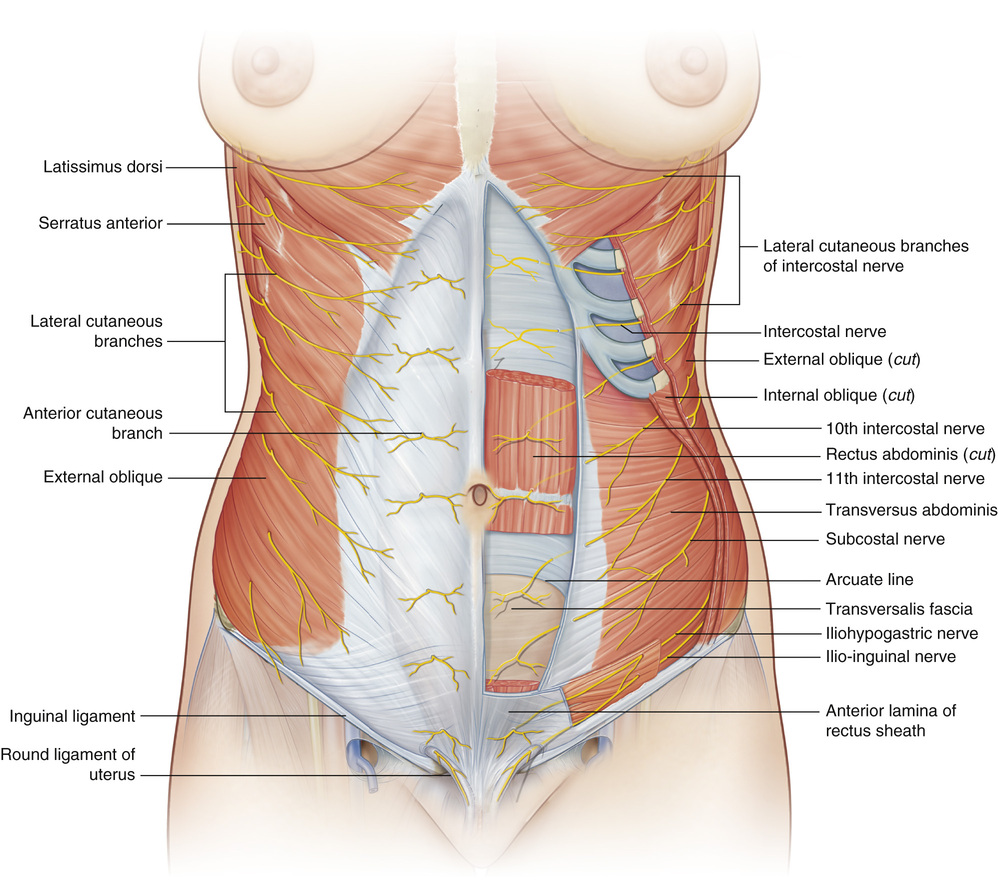
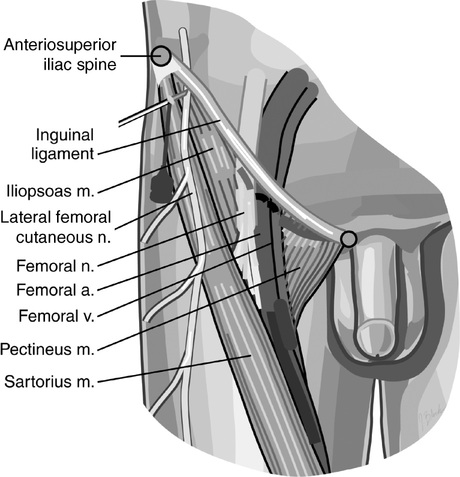
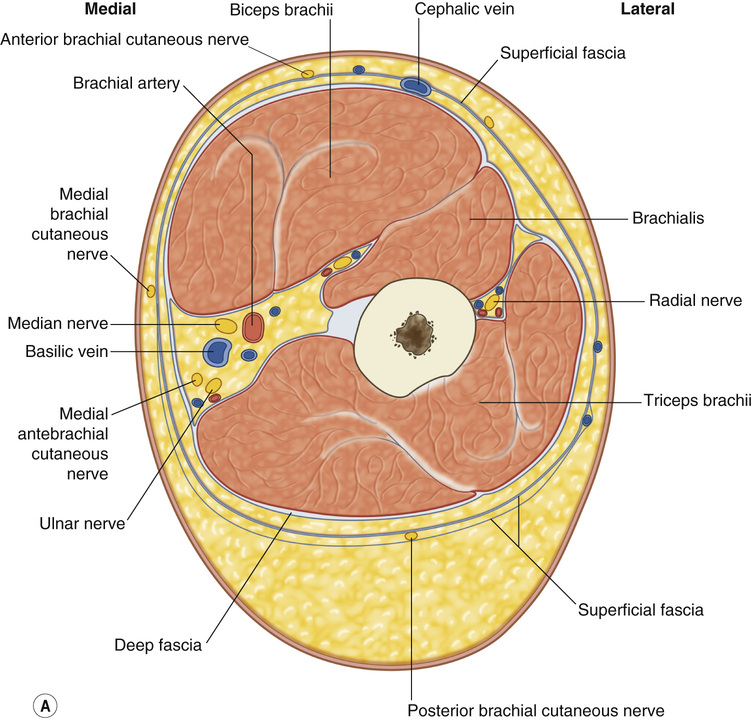
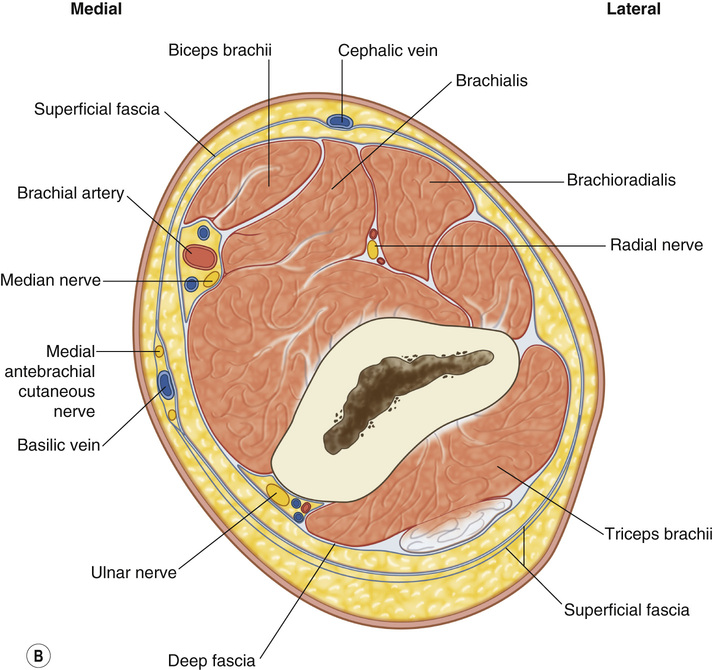
• Trunk: Removal of excess skin and subcutaneous tissue, often after massive weight loss ▪ Degree of skin excess, fatty excess, and muscular diastasis assists with selection of appropriate procedure. ○ Suction-assisted lipectomy: Minimal skin excess, moderate subcutaneous adiposity, no diastasis ○ Abdominoplasty: Excess anterior abdominal skin and subcutaneous tissue, with appreciable diastasis. Lower incision placed at least 5 to 7 cm superior to vulvar commissure ◆ Miniabdominoplasty: Short scar, often no transposition of umbilicus, minimal diastasis ◆ Fleur-de-lis: Excess skin in both transverse and vertical dimensions. By adding vertical excision, can improve vertical excess ➔ In general, perform the vertical excision first. ◆ Lipoabdominoplasty: Combination of full abdominoplasty and liposuction ○ Circumferential body lift/lower body lift: Excess skin and subcutaneous tissue circumferentially with ptosis of gluteal soft tissues ◆ Can perform gluteal lift/autoaugmentation with gluteal artery flaps ▪ Complications: Reportedly occur in 15% to 25% of patients (50% for active smokers) ○ Skin necrosis: Most commonly occurs in supraumbilical region ○ Skin dehiscence: Most common complication when combining skin resection procedures ○ Bulge: Most commonly occurs superior to umbilicus because of failure to plicate supraumbilical rectus fascia during diastasis repair ○ Encephalopathy: Most commonly associated with thiamine deficiency (Wernicke-Korsakoff encephalopathy) in the massive-weight-loss patient ○ Pain/numbness (see Figure 29.1) ◆ Lateral femoral cutaneous n.: Numbness/pain along anterolateral thigh (see Figure 29.2) ◆ Iliohypogastric n.: Numbness/pain along the inguinal crease and lateral gluteal region ➔ Danger zone: Lateral lower abdominal transverse incisions near inguinal ligament ◆ Ilioinguinal n.: Numbness along the medial thigh and scrotum/labia ➔ Danger zone: Lateral lower abdominal transverse incisions near inguinal ligament ◆ Intercostal n.: Numbness along abdominal/flank dermatomes T5 to L1 • Upper extremity/brachioplasty: Removal of excess skin and adipose tissue of the upper arm (see Figure 29.3) ○ Re-anchoring the posteromedial upper arm soft tissue to axillary fascia with nonabsorbable suture ▪ Complications: Reportedly occur in 25% to 50% of patients ○ Hypertrophic scarring (occurs in up to 40%): Most frequent complication of brachioplasty; often caused by tension, tissue mismatch, poor nutrition ◆ Treatment: Conservative including compression, silicone sheeting, steroid injection ○ Wound healing complications: Seroma, wound dehiscence ◆ Can be exacerbated by further weight loss ○ Nerve injury (occurs in up to 5%) ◆ Medial antebrachial cutaneous n. ➔ Runs in close proximity to the intramuscular septum and penetrates fascia at 14 cm proximal to the medial epicondyle; especially at risk of injury here ➔ Leads to paresthesia of upper arm and anterior proximal forearm ➔ Treat with hand therapy and local massage, gabapentin; improves with time ◆ Medial brachial cutaneous n. ➔ Runs with basilic vein, sends out branches at 7 cm and 15 cm proximal to the medial epicondyle ➔ Injury leads to numbness and paresthesias of the medial upper arm.
Body Contouring and Suction-Assisted Lipectomy
![]() Therefore, always identify nerve at this level and leave fat on deep fascia in this area.
Therefore, always identify nerve at this level and leave fat on deep fascia in this area.
Body Contouring and Suction-Assisted Lipectomy
Chapter 29