I. BACKGROUND
The most serious reactions to insects are caused by acquired hypersensitivity. Over 80% of deaths from insect bites and stings result from anaphylactic reactions and occur within 1 hour of the event. Anaphylaxis occurs in 3% of adults and 1% of children after an insect sting. Many patients who develop generalized reactions to insect bites or stings have no history of previous systemic of local reactions to the insect. Patients with a large local reaction incur only a 5% to 10% chance of developing a systemic reaction.
The most venomous insects belong to the order Hymenoptera, which includes bees, wasps, and ants. Hymenoptera venom contains serotonin, kinins, acetylcholine, lecithinase, hyaluronidase, phospholipase, and melittin. Exposure to venom in allergic individuals causes histamine release from leukocytes.
The order Diptera includes mosquitoes and flies. Mosquitoes inject salivary fluid into the victim, causing an immediate allergic reaction. Flies pierce through the skin, directly inserting saliva that causes both allergic and toxic reactions.
The order Hemiptera includes the bed bug (Cimex lenticularis) and the Reduviid bug. Historically, bed bugs were found in poor living conditions and unkempt hotels. In recent years, infestations have increased at a rapid rate and now include suburban and higher income populations as well. Bed bugs hidden in mattresses and upholstery come out at night to feed. The Reduviid bug of Mexico, Central America, and South America lives in cracks of mud hut walls and spreads disease-depositing stool on the skin as it bites.
The Meloidae and Staphylinidae families of the order Coleoptera include blister beetles. Blister beetle species of varying colors and patterns are found worldwide, with approximately 300 species residing in the United States. When blister beetles are pressed or rubbed, pederin- or cantharidin-containing hemolymph blisters the skin. Cantharidin is a toxin of medical interest, and it is used for treatment of warts and molluscum in dermatology.
II. CLINICAL PRESENTATION
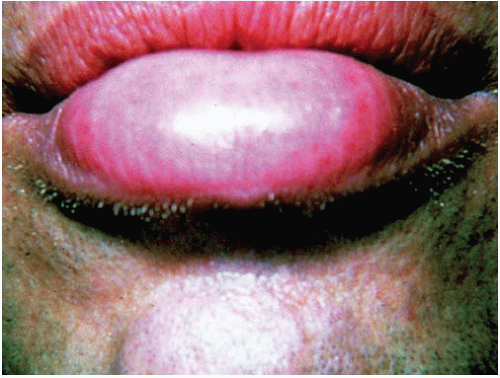
A. Hymenoptera. Hymenoptera stings usually result in instantaneous pain followed by a localized wheal and flare reaction with associated pruritus. Edema is variable (
Fig. 6-1). Multiple bee, wasp, yellow jacket, or hornet
stings can result in systemic reactions, including vomiting, diarrhea, generalized edema, dyspnea, hypotension, and collapse. Life-threatening allergic sting reactions are characterized by the usual manifestations of anaphylaxis: urticaria, laryngeal edema, bronchospasm, abdominal cramps, and shock. Harvester and fire ants are known for the intense burning and pain associated with their stings. Localized necrosis secondary to phospholipase and hyaluronidase in the venom may be present at the sting site.
B. Diptera
1. Mosquitoes. Mosquito bites result in immediate allergic reaction to injected salivary fluids. Several hours later, a pruritic papule develops. Mosquitoes can also serve as the host for diseases, including Eastern and Western Equine Encephalitis, West Nile Virus, filariasis, malaria, and yellow fever.
2. Flies. Flies bites cause immediate pruritic wheals followed by itchy, red papules. The black fly is renowned for inducing extremely painful and long-lasting reactions. Flies associated with disease are listed in
Table 6-5.
C. Siphonaptera (Fleas). Bites usually appear as grouped urticaria papules, often with a central punctum. They are commonly located on the distal extremities. Fleas are vectors for the bubonic plague, brucellosis, melioidosis, erysipeloid, and endemic typhus.
D. Hemiptera (True Bugs). Bed bugs leave linearly arranged pruritic papules in groups of two or three on the face and extremities, known as the “breakfast, lunch, and dinner” sign. The Reduviid bug acts as a vector for
Trypanosoma cruzi, causing American trypanosomiasis or Chagas disease. Known as the “kissing bug,” the Reduviid often bites the victim’s face. Local reactions include a unilateral periorbital conjunctivitis and periorbital edema, known as the “Roma-a sign,” and regional lymphadenopathy
known as the “Chagoma.” Systemic reactions include myocardial damage, megacolon, and megaesophagus.