Bilateral Sagittal Split Osteotomy for Mandibular Deficiency
Stephen B. Baker
DEFINITION
The mandible supports the lower 16 teeth, and its position is important for occlusion, airway function, jawline aesthetics, and facial form.
It is a U-shaped bone that has three points of contact: two condylar heads, which rest in the glenoid fossa of the skull base, and the mandibular teeth, which are in occlusion with the maxillary teeth.
Mandibular growth abnormalities can result in malocclusion as well as other functional problems such as airway obstruction, articulation difficulty, masticatory problems, and temporomandibular joint (TMJ) problems.1,2
The bilateral sagittal split osteotomy (BSSO) is a procedure that allows movement of the mandible in an anterior or posterior direction while maintaining overlap of the osteotomized bone segments.
The fact that the proximal and distal osteotomized bone segments overlap facilitates return to normal jaw strength and function as healing occurs.
Dal Pont modification
The anterior vertical portion of the sagittal split osteotomy should be made in the region of the mandibular first molar or slightly anterior.
The reason for this recommendation is that the inferior alveolar nerve (IAN) is more medially positioned within the mandible in this region and therefore is less at risk of injury during the osteotomy.1
Hunsuck modification
Hunsuck proposed that the horizontal portion of the BSSO on the medial ramus did not need to extend through and posterior to the lingula.
He proposed correctly that this portion of the osteotomy would split naturally if the posterior cut did not go posteriorly to the lingula.2
ANATOMY
The mandible is divided into several regions: the condyle, ramus, angle, body, parasymphysis, and the symphysis.
The lingula is a triangular bony projection on the medial surface of the mandible, immediately in front of the mandibular foramen. It provides attachment for the sphenomandibular ligament.
The genial tubercle is on the lingual side of the symphysis and is attached to the genioglossus and the geniohyoid.
In a mandibular advancement, the genial tubercle will bring these two muscles forward, which may improve the airway as well as tighten submental laxity.
In contrast, posterior positioning may impair the airway and cause submental fullness.
The IAN is a continuation of the third branch of the trigeminal nerve and enters the mandibular foramen, located on the medial aspect of the ramus. This nerve travels through the mandible in the inferior alveolar canal before exiting the mental foramen to become the mental nerve.
The mental nerve supplies sensation to the soft tissue of the ipsilateral chin with a varying degree of cross innervation to the contralateral side.
Of note is that the IAN is 4 to 5 mm below the mental foramen before it ascends to exit the foramen.
Angle Occlusal Classification
Class I: Neutro-occlusion
Molar relationship: The mesiobuccal cusp of the maxillary first permanent molar occludes with the mesiobuccal groove of the mandibular first permanent molar.
Canine relationship: The mesial incline of the maxillary canine occludes with the distal incline of the mandibular canine. The distal incline of the maxillary canine occludes with the mesial incline of the mandibular first premolar.
Mesognathic: normal, straight face profile with flat facial appearance
Class II: Disto-occlusion (overjet)
Molar relationship: The molar relationship shows the mesiobuccal groove of the mandibular first molar is distally (posteriorly) positioned when in occlusion with the mesiobuccal cusp of the maxillary first molar. Usually, the mesiobuccal cusp of maxillary first molar rests in between the first mandibular molar and second premolar.
Canine relationship: The mesial incline of the maxillary canine occludes anteriorly with the distal incline of the mandibular canine. The distal surface of the mandibular canine is posterior to the mesial surface of the maxillary canine by at least the width of a premolar.
Retrognathic: convex facial profile resulting from a mandible that is too small or maxilla that is too large
Class II malocclusion has two subtypes to describe the position of the anterior teeth:
Division 1: The molar relationships are like that of class II, and the maxillary anterior teeth are protruded. Teeth are proclined and a large overjet is present.
Division 2: The molar relationships are class II where the maxillary central incisors are retroclined. The maxillary lateral incisors may be proclined or normally inclined. Retroclined and a deep overbite exist.
Class III: Mesio-occlusion (negative overjet)
Molar relationship: The mesiobuccal cusp of the maxillary first permanent molar occludes distally (posteriorly) to the mesiobuccal groove of the mandibular first molar.
Canine relationship: Distal surfaces of the mandibular canines are mesial to the mesial surface of the maxillary canines by at least the width of a premolar. Mandibular incisors are in complete crossbite.
Prognathic: concave facial profile with prominent mandible is associated with class III malocclusion.
PATHOGENESIS
Variation in mandibular projection, either prognathia or retrognathia, has a multitude of etiologies:
Heredity
Congenital syndromes
Endocrine abnormalities
Neoplasms
Autoimmune disease
Trauma
It is important to identify the etiology and ensure mandibular growth is stable prior to performing a surgical correction.
PATIENT HISTORY AND PHYSICAL FINDINGS
Dental compensation is the term used to refer to the tendency of teeth to tilt to decrease occlusal discrepancies. For instance, in a class II occlusion, dental compensation refers to the tendency of the maxillary anterior teeth to become retroclined (moving posteriorly) while the mandibular teeth become proclined (moving anteriorly).
The degree of dental compensation is assessed with a lateral cephalometric radiograph; the degree of dental compensation must be accounted for when treatment planning for surgery.
Surgical procedures are usually planned based on the teeth in an uncompensated position. In compensated occlusion, the degree of potential mandibular movement may be underappreciated given the relationship of the compensated occlusion.
Mastication difficulties should be assessed. Dentally uncompensated retrognathic patients typically have an increased overjet, which compromises the ability of the incisors to cut and shear foods during mastication.
Airway obstruction, primarily in retrognathic patients, should be assessed. It is important to inquire about any history of snoring or sleep apnea.
If sleep apnea has not been diagnosed but is suspected based on the patient’s history, a sleep study should be obtained. Results should be incorporated into the treatment plan.
If sleep apnea is present, a two-jaw procedure may be indicated in order to open the airway while correcting the occlusion.
Aesthetic considerations of orthognathic surgery are important to consider. In particular, when treatment planning the correction of a prognathic patient, it is important to be aware of the soft tissue redundancy and submental fullness that may result with posterior positioning of the lower jaw.
Occasionally, even though the SNB is increased and the SNA is normal, the aesthetic result may be optimized by correcting the occlusion with upper jaw advancement to optimize soft tissue draping over the underlying skeletal relationship.3
Many syndromes are associated with mandibular deficiency and should be identified prior to treatment. Although the treatment may not require technical modifications, it is important to be aware of any associated syndromes prior to treatment.
Lower third facial asymmetry is not an uncommon finding in patients with dentofacial deformities.
It is important to note whether the asymmetry is due to mandibular deviation, mandibular asymmetry, or any asymmetry of the chin relative to the mandible.
Additionally, there may be maxillary asymmetry associated with mandibular asymmetry, which requires movement of the upper jaw as well.
In patients who are concerned about the aesthetic impact of insufficient mandibular projection but demonstrate a mild or minimal occlusal abnormality, advancement of the chin is a treatment option that frequently achieves the patient’s aesthetic goals without subjecting them to a sagittal split osteotomy.
IMAGING
A panoramic radiograph is a two-dimensional representation of the mandible from condyle to condyle. It is a useful screening tool for any pathology of the mandible as well as the presence of impacted third molars.
A lateral cephalometric radiograph can be used to identify soft tissue and skeletal cephalometric landmarks to perform cephalometric analyses.
Imaging of wrist growth plates is a useful tool to determine whether skeletal growth is complete or ongoing. Growth plate closure is an indication that skeletal growth is complete.
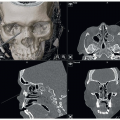
The cone-beam CT (CBCT) produces three-dimensional radiographic images of the patient’s face that can be used for computerized treatment planning and splint fabrication. The technology used in a CBCT allows the image to be obtained with a far lower dose of radiation compared with traditional CT scan.
This image is invaluable in treatment planning for the surgical approach to correct dentofacial deformities. It also aids in the fabrication of surgical splints.
Nuclear imaging is indicated to assess bone activity. It is nonspecific but is indicative of bone activity. This allows the clinician to assess the degree of bone metabolism in the condyles.
DIFFERENTIAL DIAGNOSIS
Neoplasm: Infrequently, a neoplasm may be the source of excessive mandibular growth. A neoplastic etiology typically presents as an asymmetric mandible with the teeth out of occlusion. The rapidity of tumor growth will produce a mandibular shift that exceeds the ability of the maxillary teeth to remain in occlusion. Mandibular asymmetries without a crossbite are typically associated with more chronic processes such as hemifacial microsomia or an early history of condylar trauma.
Trauma: Injury to a condyle before skeletal maturity may stunt growth, leading to mandibular asymmetry and a crossbite.
Autoimmune: Rheumatoid arthritis can cause condylar resorption resulting in an anterior open bite or mandibular retrognathia. It is important to ensure good medical control of the disease prior to undertaking surgical correction.
Developmental anomalies: Anomalies such as Pierre Robin sequence, hemifacial microsomia, or congenital syndromes may result in hypoplastic mandibles. By the time these patients are old enough to be considered for surgery, the underlying etiology has typically been elucidated and should be considered when developing the final surgical plan.
Endocrine: Acromegaly and other hormone abnormalities can lead to anomalies of mandibular size and position.
NONOPERATIVE MANAGEMENT
In mild cases of mandibular prognathia or retrognathia, it may be possible for the orthodontist to dentally compensate for the skeletal abnormality and produce a dental class I occlusion.
Occasionally, extraction of premolars may be necessary to create the space necessary to move the teeth and allow for appropriate dental compensation.
A nonsurgical approach to mandibular retrognathia frequently results in the appearance of a large nose and a weak chin. This occurs because the orthodontist has to retrocline the maxillary incisors to normalize the dental overjet. Since the incisors support the upper lip, the lip moves posteriorly as well as giving the nose an overprojected appearance.
If these patients are unhappy with their facial appearance, rhinoplasty and a genioplasty or chin implant are methods to camouflage the underlying skeletal discrepancy of the jaws and improve facial proportions.
SURGICAL MANAGEMENT
The author performs sagittal split osteotomies after the completion of facial growth.
The goal of this procedure is to anteriorly or posteriorly position the lower jaw. Additionally, this procedure may be performed to improve mandibular asymmetry.
The main steps of the procedure are as follows:
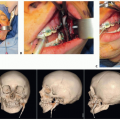
Make incisions in the mandibular mucosa.
Perform the osteotomy from the medial ramus down the ascending ramus along the external oblique bridge to the inferior mandibular cortex.
Perform the sagittal split by ensuring the IAN stays within the distal segment.
Position the patient’s teeth in a class I occlusion.
Verify condylar seating and align the proximal and distal segments with a bone clamp.
Apply rigid fixation with use of the transbuccal trocar.
Release the intermaxillary fixation and verify that the patient’s occlusion is in the desired class I position.
Close the mucosa with chromic sutures and the trocar incision with a layered subcutaneous closure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree