Back-Table Preparation of the Pancreas for Transplantation
Zoe A. Stewart
TECHNIQUES
INSPECTION OF PANCREAS ALLOGRAFT
Back-table preparation of a pancreas allograft is one of the critical determinants of a successful transplant outcome.1 The transplanting surgeon must evaluate the appearance and consistency of the gland to confirm its suitability for transplantation. Pancreata with parenchymal fatty infiltration, calcification, fibrosis, trauma, or discoloration should be discarded.
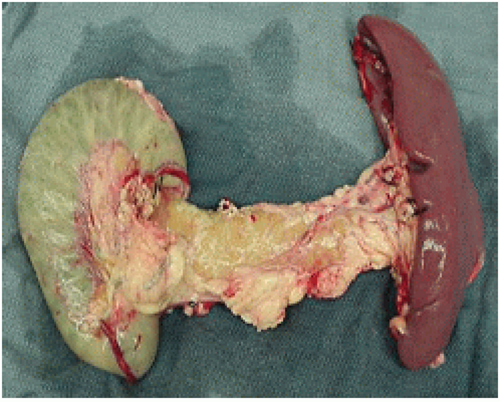
The duodenal segment is inspected for procurement injury. The pancreas allograft arteries and donor iliac arteries are evaluated to ensure suitability for reconstruction. A pancreas allograft appropriate for transplant is shown (FIG 1).
SPLENECTOMY
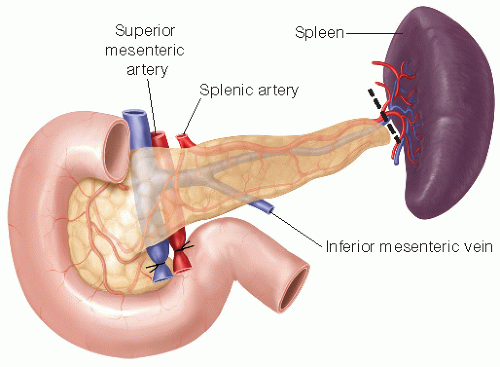
Splenectomy is performed by dividing the splenic artery and vein in the splenic hilum with ties placed on the allograft side (FIG 2). The tail of the pancreas may extend into the splenic hilum and caution must be taken to avoid injury to the allograft parenchyma during this dissection.
REMOVAL OF EXCESS TISSUE FROM THE PANCREAS BODY
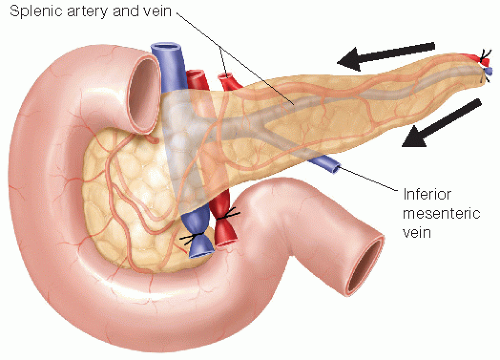
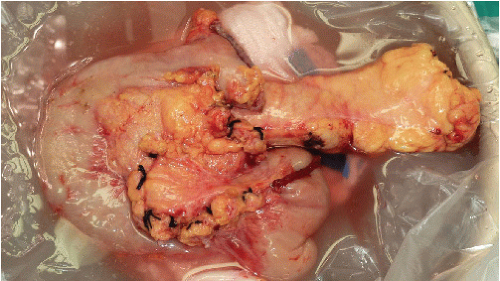
Depending on the procurement technique, it may be necessary to remove excess fat and tissue from the superior and inferior borders of the body of the pancreas (FIGS 3 and 4). On the superior pancreatic border, caution is taken to avoid injury to the splenic artery. The splenic artery orifice should have been marked with a stitch during procurement to aid in identification. Along the inferior border, the inferior mesenteric vein must be ligated if not previously ligated by the procuring surgeon.
PREPARATION OF THE PANCREAS DUODENUM
The pancreas allograft may have excess duodenum from procurement. It is important to keep the duodenal cuff short if bladder drainage is planned for the exocrine secretions in order to minimize metabolic losses. Additionally, if the duodenal cuff is left too long, it may have inadequate blood supply to the ends (FIG 5).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree