Arterial Reconstruction with Replaced Hepatic Arteries
Arterial Reconstruction with Replaced Hepatic Arteries
Paolo R. Salvalaggio
Jefferson A. Alves
Roberto F. Meirelles Jr
Sergio P. Meira Filho
Marcelo B. Rezende
PATIENT HISTORY AND PHYSICAL FINDINGS
A detailed history of the recipient must be obtained. In particular, a history of diabetes, hypercoagulability, hypertension, obesity, portal vein thrombosis, hepatocellular carcinoma, cardiovascular disease, previous abdominal and/or vascular surgeries, and smoking might be relevant.
Perform a full physical exam, with particular attention for signs of portal hypertension, ascites, abdominal diameter, previous scars, and pulses at the extremities.
In most cases, different surgical teams perform the donor and the recipient operation. Close communication between the teams is critical for the selection of the best technique to reconstruct the replaced and/or accessory arteries.
1
IMAGING AND OTHER DIAGNOSTIC STUDIES
Most transplant centers include an ultrasound during the workup of the recipient. This test will describe portal and arterial flow at the level of the hilum.
If available, a computed tomography (CT) scan or magnetic resonance imaging (MRI) can further detail portal and arterial anatomy of the recipient, including the presence of flow, size (diameter or caliber) of the vessels, and presence of replaced and/or accessory anatomy.
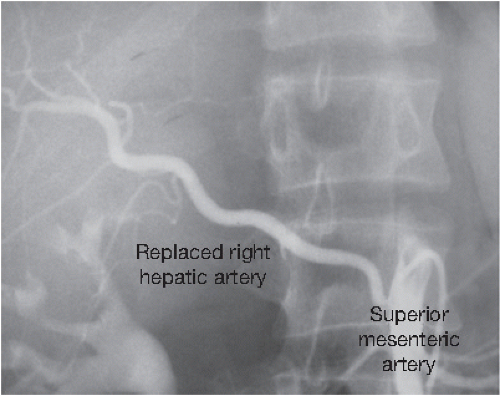
For recipients who have hepatocellular carcinoma and underwent transcatheter arterial chemoembolization (TACE) and/or radiofrequency ablation (RFA), a review of the current arteriogram may depict inconsistent flow, thrombosis, or aberrant anatomy that can alter surgical planning (
FIG 1).
SURGICAL MANAGEMENT
Preoperative Planning
Arterial reconstruction with replaced and/or accessory hepatic artery should take in consideration all data from history, physical examination, laboratory, and imaging tests of the recipients as well as the report of the surgical team that have procured the liver allograft.
There are many variations in hepatic arterial anatomy. These are classified in
Table 1.
2
Avoid the terms accessory or replaced, because it is often difficult to determine which the appropriate designation is. “Accessory” infers redundant arterial supply, but it is rarely possible to know if the supply is truly redundant and thus can be ligated. Use the terms aberrant left or right artery, not aiming to identify whether the vessel is accessory or replaced.
Record the donor and recipient arterial anatomy in the operative record.
Get Clinical Tree app for offline access