Androgenetic Alopecia
Donna R. Sadowski
David C. Reid
I. BACKGROUND
Androgenetic alopecia (ADA) is the most common form of hair loss. By age 70, approximately 80% of Caucasian men and 50% of women will have ADA, also referred to as male pattern hair loss (MPHL) and female pattern hair loss (FPHL).1,2 The etiology of ADA is multifactorial, with features such as genetic predisposition and alterations in androgen metabolism playing major roles in its development.2,3 ADA is characterized by shortening of the anagen phase, or active growth phase, of the hair growth cycle. In addition, individual follicles undergo progressive miniaturization, replacing long terminal hairs with vellus-like hairs (Fig. 3-1). This process results in clinically apparent thinning of hair. Overt baldness, however, is only seen after all follicles contained within a follicular unit have undergone miniaturization.4
Androgen hormones, in particular dihydrotestosterone (DHT), play a critical role in the pathogenesis of MPHL. Testosterone is converted to the active metabolite DHT by the enzyme 5α-reductase, which has two isoenzymes (types I and II). Type 1 5α-reductase is largely found in sebaceous glands, while type II 5α-reductase is present in high concentrations in the inner root sheaths of hair follicles and in the prostate gland. Men with androgenetic hair loss have increased amounts of DHT and 5α-reductase in scalp follicles, and men lacking 5α-reductase do not develop MPHL.2,5 Additionally, 5α-reductase inhibitors are efficacious in treating male pattern baldness.5 In contrast, the role of androgens in FPHL is less clear. Although FPHL often occurs in women with hyperandrogenism, the majority of women with FPHL have normal androgen levels.6 Female hair loss patients have less distinct patterns of alopecia and increased frequency of confounding factors, such as anemia, autoimmune disease, pregnancy, and the use of topical hair products. Additionally, treatment with 5α-reductase inhibitors has a less consistent success rate in FPHL than in MPHL.7,8
II. CLINICAL PRESENTATION
Men and women typically present with gradual, symmetric thinning of hair in a distinct pattern. This process begins postpubertally, and the incidence increases with advancing age. The amount of hair shedding and the time course may vary substantially from individual to individual.7 Men typically develop frontoparietal and frontal recession as well as vertex thinning, sometimes referred to as “M” pattern alopecia (Fig. 3-2). Progression of MPHL is commonly classified on the Hamilton-Norwood scale, ranging from stages I to VII based on the extent of alopecia.2 Women usually have diffuse central thinning of the crown and frontal scalp, described as a “Christmas tree” pattern.2 The frontal hairline is variably preserved in women (Fig. 3-3).2,7 The Ludwig (three-point) classification grades the degree of alopecia on frontal and vertex scalp, with relative preservation of the frontal hairline.7 Occasionally, female patients present with “male-type” frontotemporal and vertex thinning.
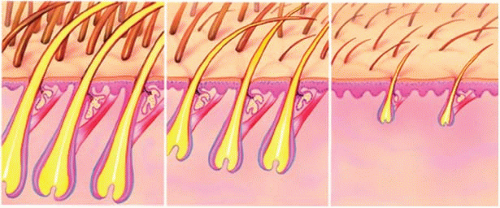 Figure 3-1. Miniaturization of hair follicles in androgenetic alopecia. (With permission from Anatomical Chart Co.) |
III. WORKUP
ADA is predominantly a clinical diagnosis, with typical history and hair loss patterns. Clinical evaluation should include examination of the scalp skin, hair density, and extent of facial and body hair. In female patients, one should also pay particular attention to signs of hyperandrogenism (e.g., acne and hirsutism).7 Laboratory examination is based upon appropriate history and physical findings (Table 3-1). Male patients seldom require laboratory evaluation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree