Nasal reconstruction provides a challenging task for any facial plastic surgeon. In performing reconstructive surgery on the nose, one must balance both the functional aspects of the nasal airway with the aesthetic responsibilities of being the central fixture of the face. Before performing surgery, the surgeon must grasp the importance of the anatomic nasal relationships and subunits, the physiology of the skin, the flaps or grafts used to reconstruct these areas, and the basic steps in wound healing. Accurate preoperative planning and analysis of the nasal defect are also vital to producing both an aesthetic and functional nose.
Anatomy, physiology, and general concepts in nasal reconstruction
Nasal reconstruction has made great strides in the last 50 years. Nasal reconstructive surgeons have gotten away from the idea of “filling the hole” and now have multiple options, which enable them to achieve an aesthetically pleasing nose and good functional results. As the central and often the most noticeable feature of the face, the nose is also one of the most difficult to reconstruct. Nasal reconstruction requires a thorough understanding of this complex, 3-dimensional structural and topographic anatomy. Also, key to this type of surgery is the relationship of the nose to the surrounding tissues of the face and how these tissues can be used for a reconstruction that is cosmetically normal for the patient and enables them to breathe properly.
The first step in nasal reconstructive surgery is an understanding of the nasal anatomy. The facial plastic surgeon must understand the intimate relationships between the underlying nasal support structures, the cover of the external skin, the function of the nasal lining, and the unique aspects of the location and contours of the nose.
Nasal Anatomy
Skin
The skin thickness varies depending on the different locations of the nose. In fact, this variation is what originally determined the nasal subunits when described by Gonzalez-Ulloa and colleagues. The thickest area is the caudal portion of the nose, on the nasal tip and ala, with its skin rich in sebaceous glands. This nasal skin progressively gets thinner until it reaches the rhinion, where it is the thinnest, and again as it transitions from the tip to the columella and the alar rim.
Soft-tissue envelope
The soft-tissue envelope is composed of 4 layers: the superficial fatty layer, the fibromuscular layer, the deep fatty layer, and the perichondrial/periosteal layer. The superficial fatty layer is intimately connected to the dermis. Immediately deep to this layer is the fibromuscular layer. This construction is called the nasal superficial musculoaponeurotic system (SMAS) and is in continuity with the rest of the SMAS overlying the face. The mimetic muscles of the nose are within this layer. The next layer is the deep fatty layer, which encases the neurovascular system, supplying the skin-soft-tissue envelope. Between this layer and the perichondrium/periosteum lies the avascular plane that is used to deglove the nose during rhinoplasty.
As mentioned previously, part of the soft-tissue envelope is composed of a muscular layer. The mimetic muscles of the nose are usually divided into 4 groups. The elevator muscles shorten the nose and dilate the nostrils. They are the procerus, levator labii superioris alaeque nasi and anomalous nasi. The depressor muscles, which lengthen the nose and dilate the nostrils, consist of the alar nasalis and depressor septi nasi. The compressor muscles lengthen the nose and narrow the nostrils. They are the transverse nasalis and compressor narium minor. Finally, the minor dilator muscle, the dilator naris anterior, widens the nostrils.
Lining
The nasal vestibule is lined by a strip of thin skin (stratified squamous keratinized epithelium). This epithelium loses its keratinizing nature and transitions into the nasal mucosa (pseudostratified columnar ciliated epithelium) as it moves further into the nose. This epithelium, called the respiratory epithelium, lines the sinonasal cavity with the exception of the area covered by the olfactory epithelium. The nasal mucosa has a rich vascular supply, which makes it an attractive option for flaps in reconstructing the inner lining of full-thickness nasal defects.
Blood supply
The blood supply to the nose comes from branches of both the external carotid artery (through the facial artery and the infraorbital artery) and internal carotid artery (through the ophthalmic and anterior ethmoidal artery) ( Fig. 1 ).

In the external carotid artery system, the facial artery has 2 terminal branches, the angular artery and the superior labial artery. The former passes in a deep groove between the nasal alae and the cheek, deep to the levator labii-superioris alaeque nasi muscle, and gives off the lateral nasal branch, which provides the blood supply to the lateral portion of the caudal nose. The angular artery then continues, following the rim of the pyriform aperture, giving off about 7 to 14 branches that perforate through the soft-tissue envelope to supply the nasal skin. The superior labial artery courses medially to the columella, where it gives off septal branches to supply the anterior portion of the nasal septal mucosa, and it terminates as the columellar artery, which runs between the medial crus of the lower lateral cartilage (LLC) and is frequently transected during the transcolumellar approach for an open rhinoplasty. The infraorbital artery arises from the infraorbital foramen with the infraorbital nerve and supplements the blood supply with branches that give rise to the lateral nasal artery and the dorsal nasal artery.
The internal carotid system also gives rise to an extensive vascular network that supplies the nose. The ophthalmic artery has both ocular and orbital branches. One of the orbital branches is the anterior ethmoidal artery, which provides the blood supply for the anterosuperior portion of the nasal cavity. After running in the skull base between the frontal sinus and the anterior ethmoid sinuses, it emerges between the cephalic edge of the upper lateral cartilage (ULC) and the caudal edge of the nasal bone, providing part of the blood supply to the nasal tip, along with the lateral nasal artery. The ophthalmic artery finally gives rise to 2 terminal branches: the frontal artery and the dorsal nasal artery. The latter pierces the orbital septum and exits the orbit just superiorly to the medial canthal ligament and runs down to anastomose with the lateral nasal artery, creating a rich, axial arterial network.
Sensory nerve supply
The skin overlying the nose is innervated by the ophthalmic (V 1 ) and maxillary (V 2 ) branches of the trigeminal nerve ( Fig. 2 ). The cutaneous branches of the ophthalmic nerve are the supratrochlear, the infratrochlear, and the external nasal nerves. The supratrochlear branch exits at the supraorbital foramen, and the infratrochlear branch exits the orbit just superior to the medial canthus. They provide sensory supply to the skin of the nasion, radix, and rhinion and the cephalic portion of the lateral nasal sidewall. The external nasal branch comes from the anterior ethmoid nerve and emerges between the ULC and the nasal bone, accompanied by the anterior ethmoidal artery. This branch innervates the skin of the caudal nasal dorsum and nasal tip.
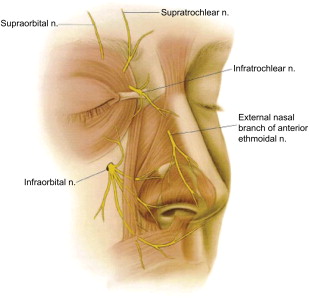
The branches of the maxillary nerve are the infraorbital nerve and the nasopalatine nerve. The infraorbital branch courses on the roof of the maxillary sinus and exits the cranium at the infraorbital foramen. It innervates the skin of the caudal portion of the lateral nasal sidewall, ala, and nasal vestibule. The nasopalatine branch enters the nose through the incisive foramen and innervates the nasal septal mucosa.
Bone and cartilaginous framework
The bony framework is a pyramidal structure that consists of the paired nasal bones and the ascending process of the maxilla on either side. The cephalic portion articulates with the frontal bone superiorly and caudally, forming the cranial portion of the pyriform aperture ( Fig. 3 ). The nasal bones are thicker superiorly and progressively become thinner until their free edge inferiorly. The nasal bones are, on average, 25 mm, but their length can vary significantly. They fuse at the midline and give an internal projection that supports the perpendicular plate of the ethmoid bone. Inferiorly, the nasal bones articulate with the overlapped cephalic portion of the ULC, which are fused medially with the cartilage of the nasal septum. This area of confluence between the nasal bones, perpendicular plate of the ethmoid bone, ULCs, and cartilage of the nasal septum is connected by a dense fibrous tissue and is called the “keystone area.” This region provides critical support to the midvault of the nose.
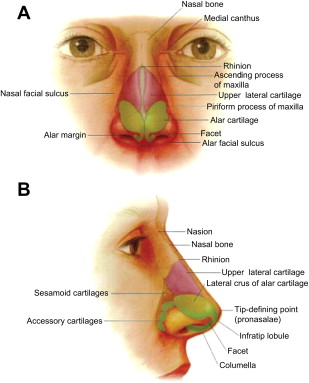
The upper cartilaginous vault is made by the ULCs and the fused cartilaginous nasal septum. The cephalic two-thirds of the ULCs are fused with the nasal septum, and as they extend inferiorly, the ULC gradually separates and flares laterally from the septum. The lateral portion of the ULC does not have any skeletal support because it does not articulate with the pyriform aperture but ends in an area called the external lateral triangle. This area is bordered by the pyriform aperture, the ULC, and the cephalic border of the lateral aspect of the LLC. It is covered by the transverse nasalis muscle and may contain one or more sesamoid cartilages. The most caudal aspect of the LLC ideally forms an angle with the nasal septum at the area of the internal nasal valve, which is described in more detail later in the article.
The lower cartilaginous framework is formed by the LLC. This paired cartilage morphology is made of 3 portions: the medial, middle, and lateral crura. The medial crus has 2 components: the footplate and the columellar portion. These segments rotate in 2 angles: the angle of cephalic rotation and the angle of footplate diversion. The medial crus has its configuration in 3 anatomic variations: the asymmetric parallel, flared symmetric, and straight symmetric. Anteriorly, the medial crus transitions to the middle crus in the columellar breakpoint. The middle crus is made up of the lobular and the domal segments. The lobular segment is usually camouflaged by the overlying soft-tissue envelope. On the other hand, the domal segment is often visible and is critical in determining the tip-defining points. Its external expression depends on its angulation, the divergence of the 2 defining points, and the thickness of the overlying soft tissue. The middle crus is connected to the opposite side by the interdomal ligament. Superiorly, the LLC curves and transitions into the lateral crus. This portion of the LLC plays a major role in determining the shape of the alar region. It articulates superiorly with the caudal edge of the ULC in the “scroll area” where there is usually some degree of overlap, most commonly with the LLC coming externally to the ULC. The LLC varies in shape and size, and the longitudinal axis of the lateral crus approaches 45°. This angle turns the LLC to a more cephalic position as it projects laterally, away from the alar rim, and that is the reason why the LLC provides support only to the medial half of the nasal ala.
Nasal valves
The nasal valves are the portion of the nose that regulates airflow, because they have the narrowest cross-sectional area of the entire airway. They are usually described individually as the external and internal nasal valves. The resistance in the nasal airway can be divided between the nasal vestibule, internal nasal valve, and the turbinated cavity of the nasal passage. Whereas the nasal vestibule contributes only about one-third of the nasal resistance and the nasal passage with its turbinates contribute only minimally, the nasal valves comprise the major areas of resistance in the nasal cavity.
The internal nasal valve corresponds to the area between the head of the inferior turbinate, the nasal septum, and the ULC. A key portion of this valve is the angle between the nasal septum and the ULC, the normal range of which is 10° to 15°. The internal nasal valve area is the flow-limiting segment of the nasal airway and comprises about 50% of the total airway resistance from the nasal vestibule to the alveoli. Nasal resistance functions according to Poiseuille’s law; it is inversely proportional to the fourth power of the radius of the nasal passages (resistance = [viscosity × length]/radius 4 ). This means that small changes in the size of the nasal valve can have exponential effects on the airflow resistance. As mentioned earlier, Bernoulli principle plays a key role in the physiology of the nasal valve. As the air flows across the narrowed nasal valve, the velocity increases and pressure decreases. This negative pressure in the valve area causes further nasal valve collapse. Not only the internal nasal valve but also the external nasal valve or nasal ala may collapse from the increased negative pressures developed from inspiration.
The external nasal valve is formed by the nasal ala and its supporting structures. It consists of the columella (fixed portion) medially and the lateral crura of the LLC (mobile portion). This mobile portion tends to collapse with inspiratory flow by the Bernoulli effect, but this collapse is resisted by the action of the dilator nares and the levator labii alaeque muscles along with the intrinsic strength of the LLC. The flow in the external nasal valve is primarily determined by the position of the cartilage and is minimally influenced by the degree of mucosal engorgement.
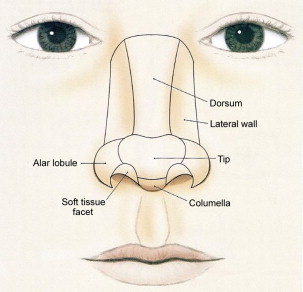
Subunit Approach to Cutaneous Anatomy
In the early days of facial reconstruction, the main goal was to provide tissue coverage to the defect without significant concern with the cosmetic appearance. This concept started to change in the 1950s when surgeons started to advocate the use of “like tissue” to replace “like tissue.” They noted that, by giving the reconstructed defect an appropriate contour and color match, the viewing eye would more likely perceive the area as normal. As described earlier, the initial work for improving facial reconstruction was made by Gonzalez-Ulloa and colleagues, when they observed that the face had distinct units with transition lines between them. They postulated that these units would be determined by differences in the underlying histologic characteristics between the adjacent areas. The skin characteristics include thickness, amount of subcutaneous fat, color, texture, and presence of hair. The transition lines, or aesthetic borders, include the anterior hairline, mental crease, melolabial crease, orbital rim, preauricular crease, and nasofacial groove. The investigators determined that the main aesthetic units of the face are the forehead, eyelids, cheeks, lips, mentum, auricles, and nose. Placing incisions along those transition lines would camouflage the reconstruction. Millard expanded the concept, advocating that not only the incisions should be transition lines but also the entire unit should be reconstructed.
Building on those previous concepts, Burget and Menick further developed this philosophy, dividing the nose into subunits ( Fig. 4 ). In a landmark article, they identified the specific topographic subunits as the dorsum, tip, columella and the paired ala, sidewalls, and soft triangles. They suggested that when reconstructing nasal defects, replacing entire subunits generally provided better aesthetic results. Their results were supported by data from perceptive psychology. They also described the “50% rule,” advocating that, in patients in whom more than 50% of the involved subunit was removed, the reconstruction should encompass the entire subunit, which would include removing healthy skin from the surrounding area. For defects that were less than 50% of the subunit, the reconstruction should provide adequate contour and color match, without removing healthy tissue.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








