Nasal reconstruction remains a significant surgical challenge. The melolabial flap and its multiple variations relies on the robust vascularity and abundant subcutaneous fat of the melolabial fold, to transfer skin and soft tissue to the lower one-third of the nose, the nasal sidewall or as a replacement for nasal lining while hiding the donor scar in the melolabial crease. This content discusses pertinent cutaneous anatomy, patient selection, preparation and education, flap design, surgical techniques and post-operative considerations to enable the surgeon to achieve a reconstruction result that closely approximates the pre-injury state while producing limited donor site deformity.
Nasal defects, particularly those created by Mohs surgery to eradicate locally invasive skin carcinoma, can leave the patient with a deformity of significant magnitude. The challenge for the reconstructive surgeon, as in all cases, is to recreate the patient’s normal anatomy as accurately and naturally as possible with a minimum of additional noticeable scar. Regardless of the circumstance that leads to the nasal deformity, the reconstructive options selected, closely related to the skill and artistry of the surgeon, most often dictate the aesthetic and functional outcome of the reconstructive effort. Due to the critical function of the nose, nasal breathing must be maintained or in some cases improved during reconstruction. This functional challenge, in addition to the importance of nasal appearance to one’s sense of identity and attractiveness, makes nasal reconstruction a particular challenge.
Defects of the nose that are too large to close using local nasal flaps, are not appropriately repaired with a skin graft or are unfavorable for healing by secondary intention, regional flaps present an important, available source of vascularized soft tissue for reconstruction. Although there are several important regional flaps available for nasal reconstruction, the melolabial flap is one of the workhorse flaps used by the nasal reconstructive surgeon. This article reviews the anatomy of the melolabial fold; the various designs, applications, advantages, and disadvantages of the melolabial flap; preoperative considerations, patient education, and photodocumentation; the types and size of nasal defects best addressed with these flaps; the technical aspects of surgical execution; and the postoperative measures required to obtain an optimal, aesthetic, and functional result.
Anatomy of the melolabial crease and fold
The melolabial crease is an important facial landmark, which grossly distinguishes the cheek from the lips. It is also recognized as the nasolabial crease because it provides a distinction between the caudal aspect of the nose and the cheek. However, the preferred terminology is the melolabial crease as it best describes this anatomic feature. Understanding the anatomy of the melolabial crease and corresponding fold is essential not only for fashioning the melolabial flap but also for a comprehensive appreciation of the changes that take place in the aging face. The anatomy of this crease and fold have been described extensively in prior publications; this article delineates the gross anatomy, histology, and pertinent vascular and neural anatomy of the melolabial region as they each are related to the creation of melolabial flaps.
Gross Anatomy
The mimetic muscles of the face are surrounded by a layer of fascia known as the superficial musculoaponeurotic system (SMAS). This fascial layer continues as the platysma in the neck and as the frontalis muscle in the forehead, eventually becoming the galea aponeurotica of the scalp. Overlying the temporal region, this fascia continues as the temporoparietal fascia. The SMAS overlies the parotid gland, superficial to the parotidomasseteric fascia. In this region, studies have shown the SMAS to be thick and fibrous. As the SMAS continues medially toward the melolabial fold, its fibrous connective tissue becomes progressively thinner because it envelops the mimetic muscles, including the zygomaticus major, zygomaticus minor, orbicularis oris, levator labii superioris, depressor labii inferioris, levator anguli oris, and depressor anguli oris. All these muscles surround the melolabial fold and send out vertically oriented fibrous septa to the dermal layer of the skin. This construct allows the face to express a broad spectrum of emotions, based on the relative contractions and actions of these mimetic muscles.
At the junction of the cheek and lip, there is a dense concentration of the fibrous mimetic muscular decussations. This consolidated area of fibrous extensions results in the melolabial crease. There is a thicker layer of subcutaneous fat lateral to the melolabial crease that facilitates a smooth gliding motion of the mimetic muscles in relation to the skin. These fibrous extensions must traverse this fat layer, and thus, movement of the facial muscles moves both the skin and the thick fat layer below it. Medial to the melolabial crease, however, there is virtually no subcutaneous fat, and some studies suggest that the orbicularis oris fibers attach directly to the dermis in this region. The juxtaposition of the thick subcutaneous fat layer lateral to the crease compared with the subcutaneous tissues overlying the orbicularis oris, which is devoid of fat, creates what is clinically recognized as the melolabial fold. This lateral fat layer is clinically important because it provides adequate bulk and vascularity to the melolabial flap.
Histology
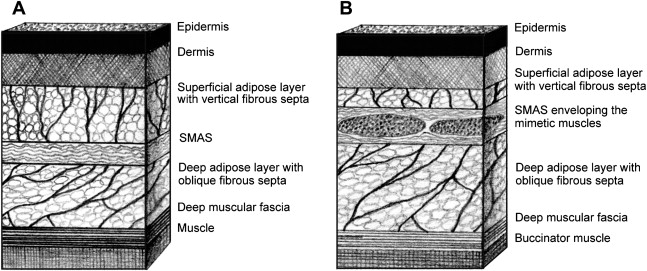
Evaluation of the microscopic anatomy of the melolabial area reinforces the findings of gross dissection. The following structures are encountered in sequence as the analysis moves from superficial to deep layers: epidermis, dermis, superficial adipose layer with vertically oriented fibrous septa, SMAS (a laminar layer of connective tissue), deep adipose layer with obliquely oriented fibrous septa, and deep (muscular) fascia ( Fig. 1 ). While moving from the lateral cheek to the melolabial crease, the superficial adipose layer and SMAS thin, whereas the deep adipose layer thickens. Additionally, the SMAS envelops the mimetic muscle of the medial face. Thus, the vertically oriented fibrous septa found within the superficial adipose layer connect the SMAS to the dermis and transmit muscular movements to the skin. This transmission allows the facial skin to move and express emotions.
Vascular Anatomy
Unlike an axial flap that contains a named artery along its length, the melolabial flap is considered a random flap that is solely dependent on the microvascular anatomy of the melolabial region. Therefore, it is critical to understand the relationship of the blood supply to the superficial subcutaneous fat layer and the overlying skin when raising a melolabial flap.
The medial cheek is perfused primarily from branches of the facial artery and drained by the facial vein, with additional blood supply derived from the infraorbital artery and vein. The facial artery is a primary branch, and the infraorbital artery is a terminal branch of the external carotid system. Melolabial flaps are random flaps that take advantage of this rich vasculature via unnamed musculocutaneous arterial perforators that supply blood flow to the skin. Therefore, survival of this flap is contingent on perfusion pressure rather than being solely dependent on the flap’s length to width ratio.
Perfusion of the facial skin is facilitated by a horizontal arrangement of several vascular plexuses that lie in a parallel fashion and are distributed at different depths within the skin and its related soft tissue structures. The most superficial of these plexuses is the dermal plexus and the closely related subepidermal plexus. The dermal plexus is important for thermoregulation, whereas the function of the subepidermal plexus is to supply the skin with nutrients.
The subdermal plexus is the vascular circuit encountered immediately deep to the subepidermal plexus. The integrity of this plexus is absolutely critical to flap survival because it is these vessels that are primarily responsible for the cutaneous blood supply. The abundance of the subdermal plexus is indicated by the bleeding encounterd along the skin edge after an incision is made. Histologically, this plexus is found between the reticular dermis and the SMAS, within the superficial adipose layer.
The subcutaneous plexus and fascial plexus are then encountered sequentially, deep to the subdermal plexus. The fascial plexus is important when designing fasciocutaneous flaps, which are beyond the scope of this discussion.
Neural Anatomy
The infraorbital nerve, the second division of the trigeminal nerve, exits the infraorbital foramen approximately 2.5 cm from the midline and 1 cm below the inferior orbital rim and provides cutaneous sensation in the part of the face that involves the melolabial fold. This nerve has 3 main terminal branches: the lower palpebral, external nasal, and upper labial. These terminal branches have an average of 5.3, 7.0, and 7.3 end branches, respectively. The external nasal and upper labial branches are most relevant to the melolabial fold. Most of the cutaneous endings of these branches are located medial to the melolabial fold. However, studies have demonstrated a tremendous redundancy and cross-innervation in this region, which explains why hypoesthesia and/or anesthesia is an infrequently encountered consequence of melolabial flaps.
Advantages and disadvantages of melolabial flaps
The melolabial flap is a cutaneous facial flap adjacent to the nose and lip, which takes advantage of the abundant, mobile, well-vascularized soft tissue mound of the medial cheek, and is commonly referred to as the melolabial fold. The skin of this region is appealing for nasal reconstruction because it provides reasonable skin color match, thickness, and texture. Because of the robust vascularity of the medial cheek skin, melolabial flaps lend themselves to several different designs. In each case, the flap takes advantage of the mobile and redundant skin of the medial cheek to correct a deformity of the lateral nasal sidewall or the lower one-third of the nose, depending on the flap’s design. The nomenclature defining the different types of melolabial flaps is based on the mechanisms of movement of skin and soft tissue harvested from the melolabial fold region.
The base of the melolabial transposition flap must be contiguous with the defect being reconstructed, and the donor scar hidden within the melolabial crease. This flap permits the recruitment of lax tissue from the cheek to repair nasal sidewall defects in a single stage. Because the skin of the medial cheek remains attached, blood supply and lymphatic drainage remain intact. Unlike a skin graft, a circumferential scar is avoided, which can lead to a trapdoor deformity. Although defects involving the nasal sidewall can be closed with this flap, the transferred skin matches best for defects of the lower one-third of the nose, which tends to have thicker and more sebaceous skin than the upper two-thirds of the nose. The most significant potential shortcoming of this flap design is that it can distort the alar facial sulcus because the flap must traverse this anatomic junction, which is critical to a normal appearance and is nearly impossible to completely correct once obliterated.
The second category of melolabial flaps avoids obliteration or distortion of the alar facial groove by crossing over the alar facial sulcus rather than going through it. The second category includes the interpolated subcutaneous tissue pedicle melolabial flap and the interpolated cutaneous pedicle melolabial flap. In each case, the flap is transferred across the alar facial sulcus with a pedicle of soft tissue that is removed in a second surgical stage several weeks after the initial flap transfer. Both types of interpolated flaps can be designed to reach, without tension, the lower half of the nose when rotated about their axis of attachment while providing full-thickness external soft tissue replacement. However, as with any interpolated flap, the need for at least 2 procedures is perhaps the most significant shortcoming. The initial procedure transfers the flap and closes the defect, followed by a second procedure after several weeks to sever the flap’s pedicle and complete the inset. The theoretic advantage of the interpolated subcutaneous tissue pedicle melolabial flap is that the flap’s nourishment is supplied by an attached mobilized subcutaneous fat pedicle, which may have improved vascular and lymphatic supply relative to the cutaneous pedicle flap. In addition, during pedicle division and flap inset, simply dividing and trimming the fat pedicle is often all that is needed, which create less distortion of the superior aspect of the melolabial crease and fold than the interpolated cutaneous pedicle melolabial flap. However, a significant shortcoming to the interpolated subcutaneous tissue pedicle melolabial flap design is that mobilizing the fat pedicle needs a wide dissection, placing the facial nerve branches to the zygomaticus major and minor muscles at risk. The interpolated cutaneous pedicle melolabial flap does not carry this risk, is better suited to thin faces with minimum subcutaneous fat, and reaches to the nasal supratip more easily. However, to optimize the flap’s blood supply, at least 3 mm of fat should be preserved on its undersurface. An additional benefit of this flap is that if the distal aspect of the flap becomes necrotic and fails, because it is the most distal aspect of the flap and thus the most vulnerable, then the repair can sometimes be salvaged because vascularized skin is in abundance. If the pedicle is of sufficient length, the necrotic tissue can be debrided and the proximal aspect of the flap advanced distally into the wound bed, giving the reconstruction a second chance to heal. Lastly, in either interpolated melolabial flap design, a relatively thick subcutaneous fat layer may necessitate a future contouring procedure several months after the flap pedicle detachment.
Another flap design uses the superiorly based interpolated cutaneous pedicle melolabial flap as a hinge flap. When flipped 180° about its point of attachment, the skin of the melolabial fold can be used to replace nasal lining along the ipsilateral nasal sidewall. This staged flap design is helpful when other lining tissues are unavailable.
For most patients, regardless of the melolabial flap design used, the donor site scar can be well camouflaged in their existing melolabial crease. With time, the donor scar is often difficult to identify. An additional advantage of melolabial flap reconstruction is that it may be performed comfortably under local anesthesia. An infraorbital nerve block using lidocaine with epinephrine supplemented with a local anesthetic infiltration of the operative sites provides both anesthesia and hemostatic assistance. This method is particularly useful in the older ill patient in whom a general anesthetic may pose an unacceptable medical risk, possibly by delaying or preventing reconstruction.
Regardless of flap design, the most significant disadvantage is the random vascularity of the melolabial flap, which makes it less reliable than the similar axially based soft tissue flaps. The random blood supply, which relies on the subepidermal and subdermal vascular plexuses for flap viability, is at a particular risk in patients who smoke tobacco or have a disease that compromises the skin microvasculature. Additionally, for younger patients with good skin tone and a minimal melolabial crease, hiding the donor scar may be more challenging. However, with proper wound healing, sun protection, and time, these scars often do well even in this group of patients. Of course, the skin quality, which is less sebaceous than the lower one-third of the nose, is not a perfect replacement for nasal skin, and a line of demarcation between the flap and the native nasal skin is always discernable. However, no other skin is similar to that of the lower nose, and thus, this limitation is not unique to the melolabial flap. In addition, if the patient has abundant facial hair follicles, designing a flap for external nasal coverage may be challenging. If this flap is determined to be the best reconstructive option in spite of the issue of facial hair, depilatory techniques should be used postoperatively. However, this limitation is also seen in other regional flaps such as the forehead flap.
Advantages and disadvantages of melolabial flaps
The melolabial flap is a cutaneous facial flap adjacent to the nose and lip, which takes advantage of the abundant, mobile, well-vascularized soft tissue mound of the medial cheek, and is commonly referred to as the melolabial fold. The skin of this region is appealing for nasal reconstruction because it provides reasonable skin color match, thickness, and texture. Because of the robust vascularity of the medial cheek skin, melolabial flaps lend themselves to several different designs. In each case, the flap takes advantage of the mobile and redundant skin of the medial cheek to correct a deformity of the lateral nasal sidewall or the lower one-third of the nose, depending on the flap’s design. The nomenclature defining the different types of melolabial flaps is based on the mechanisms of movement of skin and soft tissue harvested from the melolabial fold region.
The base of the melolabial transposition flap must be contiguous with the defect being reconstructed, and the donor scar hidden within the melolabial crease. This flap permits the recruitment of lax tissue from the cheek to repair nasal sidewall defects in a single stage. Because the skin of the medial cheek remains attached, blood supply and lymphatic drainage remain intact. Unlike a skin graft, a circumferential scar is avoided, which can lead to a trapdoor deformity. Although defects involving the nasal sidewall can be closed with this flap, the transferred skin matches best for defects of the lower one-third of the nose, which tends to have thicker and more sebaceous skin than the upper two-thirds of the nose. The most significant potential shortcoming of this flap design is that it can distort the alar facial sulcus because the flap must traverse this anatomic junction, which is critical to a normal appearance and is nearly impossible to completely correct once obliterated.
The second category of melolabial flaps avoids obliteration or distortion of the alar facial groove by crossing over the alar facial sulcus rather than going through it. The second category includes the interpolated subcutaneous tissue pedicle melolabial flap and the interpolated cutaneous pedicle melolabial flap. In each case, the flap is transferred across the alar facial sulcus with a pedicle of soft tissue that is removed in a second surgical stage several weeks after the initial flap transfer. Both types of interpolated flaps can be designed to reach, without tension, the lower half of the nose when rotated about their axis of attachment while providing full-thickness external soft tissue replacement. However, as with any interpolated flap, the need for at least 2 procedures is perhaps the most significant shortcoming. The initial procedure transfers the flap and closes the defect, followed by a second procedure after several weeks to sever the flap’s pedicle and complete the inset. The theoretic advantage of the interpolated subcutaneous tissue pedicle melolabial flap is that the flap’s nourishment is supplied by an attached mobilized subcutaneous fat pedicle, which may have improved vascular and lymphatic supply relative to the cutaneous pedicle flap. In addition, during pedicle division and flap inset, simply dividing and trimming the fat pedicle is often all that is needed, which create less distortion of the superior aspect of the melolabial crease and fold than the interpolated cutaneous pedicle melolabial flap. However, a significant shortcoming to the interpolated subcutaneous tissue pedicle melolabial flap design is that mobilizing the fat pedicle needs a wide dissection, placing the facial nerve branches to the zygomaticus major and minor muscles at risk. The interpolated cutaneous pedicle melolabial flap does not carry this risk, is better suited to thin faces with minimum subcutaneous fat, and reaches to the nasal supratip more easily. However, to optimize the flap’s blood supply, at least 3 mm of fat should be preserved on its undersurface. An additional benefit of this flap is that if the distal aspect of the flap becomes necrotic and fails, because it is the most distal aspect of the flap and thus the most vulnerable, then the repair can sometimes be salvaged because vascularized skin is in abundance. If the pedicle is of sufficient length, the necrotic tissue can be debrided and the proximal aspect of the flap advanced distally into the wound bed, giving the reconstruction a second chance to heal. Lastly, in either interpolated melolabial flap design, a relatively thick subcutaneous fat layer may necessitate a future contouring procedure several months after the flap pedicle detachment.
Another flap design uses the superiorly based interpolated cutaneous pedicle melolabial flap as a hinge flap. When flipped 180° about its point of attachment, the skin of the melolabial fold can be used to replace nasal lining along the ipsilateral nasal sidewall. This staged flap design is helpful when other lining tissues are unavailable.
For most patients, regardless of the melolabial flap design used, the donor site scar can be well camouflaged in their existing melolabial crease. With time, the donor scar is often difficult to identify. An additional advantage of melolabial flap reconstruction is that it may be performed comfortably under local anesthesia. An infraorbital nerve block using lidocaine with epinephrine supplemented with a local anesthetic infiltration of the operative sites provides both anesthesia and hemostatic assistance. This method is particularly useful in the older ill patient in whom a general anesthetic may pose an unacceptable medical risk, possibly by delaying or preventing reconstruction.
Regardless of flap design, the most significant disadvantage is the random vascularity of the melolabial flap, which makes it less reliable than the similar axially based soft tissue flaps. The random blood supply, which relies on the subepidermal and subdermal vascular plexuses for flap viability, is at a particular risk in patients who smoke tobacco or have a disease that compromises the skin microvasculature. Additionally, for younger patients with good skin tone and a minimal melolabial crease, hiding the donor scar may be more challenging. However, with proper wound healing, sun protection, and time, these scars often do well even in this group of patients. Of course, the skin quality, which is less sebaceous than the lower one-third of the nose, is not a perfect replacement for nasal skin, and a line of demarcation between the flap and the native nasal skin is always discernable. However, no other skin is similar to that of the lower nose, and thus, this limitation is not unique to the melolabial flap. In addition, if the patient has abundant facial hair follicles, designing a flap for external nasal coverage may be challenging. If this flap is determined to be the best reconstructive option in spite of the issue of facial hair, depilatory techniques should be used postoperatively. However, this limitation is also seen in other regional flaps such as the forehead flap.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






