31 Aesthetic genital surgery
Synopsis
 Male and female aesthetic genital surgery can greatly enhance confidence if a real or perceived deformity exists.
Male and female aesthetic genital surgery can greatly enhance confidence if a real or perceived deformity exists.
 Many new genital surgeries have been developed.
Many new genital surgeries have been developed.
 In the male, penile enlargement surgery can result in severe deformities, which can often be reconstructed.
In the male, penile enlargement surgery can result in severe deformities, which can often be reconstructed.
 Hidden penis, penoscrotal web, and scrotum reduction surgeries are very successful with a low complication rate.
Hidden penis, penoscrotal web, and scrotum reduction surgeries are very successful with a low complication rate.
 Labia minora and clitoral hood reduction performed by the “extended central wedge” excision gives a natural appearance with very high patient satisfaction.
Labia minora and clitoral hood reduction performed by the “extended central wedge” excision gives a natural appearance with very high patient satisfaction.
 Mons pubic lifting and labia majora reduction, with or without fat excision, increase self-esteem.
Mons pubic lifting and labia majora reduction, with or without fat excision, increase self-esteem.
 As with all aesthetic surgeries, genital surgery requires the same meticulous attention to detail.
As with all aesthetic surgeries, genital surgery requires the same meticulous attention to detail.
Male genital aesthetic surgery
Measurements
Schonfeld and Beebe1 determined that the length of the fully stretched flaccid penis correlated closely with the erect penis. The dorsal length from the junction of the penopubic skin to the tip of the glans in the fully stretched flaccid penis correlated closely to the erect penis. Erect girth or circumference correlated with girth measurements of the flaccid penis according to a more complicated ratio.
Da Ros and Teloken et al.2 performed artificial erections on 150 Caucasian men, measuring penis length from the center of the pubic bone to the tip of the glans and penis circumference at the corona and base. Average penis length was 5.7 inches; 18 were shorter than 4.7 inches and 18 longer than 6.3 inches. Circumference at the base of the penis ranged from 3.5 to 5.9 inches (average 4.7) and at the coronal groove from 3.2–5.5 inches (average 4.4).
Wessells et al.3 compared the relationship between penile length in the flaccid stretched and in erect states and also concluded that there was a positive relationship. The average flaccid stretched penile length was 11 cm, while the average erect penile length was 12.5 cm. The correlation between stretched length and erect length was r2 = 0.769. Average flaccid circumference was 10 cm with an average erect circumference of 12.5 cm, and, therefore, correlation was not favorable for circumference. They also state that a thick pubic fat pad decreases visible flaccid penile length but not functional penile length during intercourse.
Anatomy
The suspensory ligament of the penis is a thick, triangular band extending from the linea alba and the upper portion of the symphysis pubis and arcuate ligament to the dorsal midline of the penis.4 It derives from the outer investing fascia of the abdomen and divides into a sling at the junction of the fixed and mobile portions of the penis. In addition, thickened bands of Scarpa’s fascia, called the fundiform ligaments, firmly attach to the rectus fascia above the pubic symphysis and extend onto the dorsal and lateral penis, possibly restricting penile excursion.5
The skin of the penis is thin, hairless (more distal), and has loose connections with the deeper structures of the penis. No adipose tissue is present under the skin. The superficial or subcutaneous fascia of the penis (dartos fascia) is continuous with the Scarpa’s and Camper’s fascias of the lower abdomen and extends to the corona of the penis. The dartos fascia contains scattered smooth muscle cells. Branches of the superficial external pudendal vessels provide the blood supply to the dartos fascia and skin. The internal pudendal system, which includes the deep dorsal arteries and veins and the cavernosal and urethral vessels, usually communicates with the external pudendal system only at the glans and corona.6 Because the dartos fascia is highly vascular, it provides an excellent tissue bed for grafts. Buck’s fascia invests the shaft of the penis deep to the dartos fascia. The dorsal nerves of the penis supply erogenous sensation to the glans penis. The deep dorsal vessels and the dorsal nerve travel in the pudendal canal along the ischial ramus and then pass ventrally along the margin of the inferior ramus of the pubis in the deep perineal pouch. The neurovascular bundles pierce the perineal membrane  inch from the symphysis pubis and continue within Buck’s fascia of the penis. Each of the two deep dorsal arteries lies between the deep dorsal vein in the midline and the dorsal nerves of the penis laterally.
inch from the symphysis pubis and continue within Buck’s fascia of the penis. Each of the two deep dorsal arteries lies between the deep dorsal vein in the midline and the dorsal nerves of the penis laterally.
Penile enlargement
Penile lengthening
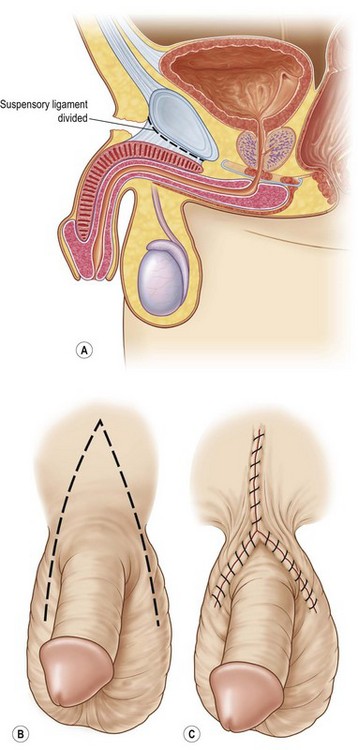
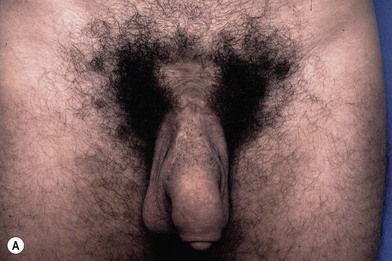
Penile lengthening is achieved by releasing the suspensory ligament of the penis and the postoperative use of penile weights or stretching devices (Fig. 31.1A).7–10 The ligament is released only one fingerbreadth by cutting directly on the periosteum throughout the length of the midline pubic symphysis. The release is usually performed through a 3–4 cm lower transverse incision just above the penopubic junction, but many surgeons advance infrapubic skin onto the penis using a VY advancement flap (Fig. 31.1B,C).11,12 This VY flap theoretically increases penile length or gives the penis the appearance of increased flaccid length, which may occur if the patient has a shortage of penile skin. Penile length gain is disputed in most cases, and the VY flap can actually cause the penis to appear either longer or shorter in the flaccid state. The VY flap is based distally at the penopubic junction varying from a small (2–3 cm) to a large base. The larger flap encompasses the entire dorsal base of the penis and part of the scrotum, which causes interruption of a significant portion of the proximal penile dartos fascia and skin. The blood supply and lymphatic drainage of the penis is thus partially interrupted which can cause healing complications such as flap tip loss, poor wound healing with wound dehiscence, and postoperative swelling. Healing problems predispose to hypertrophic or wide scars, which create hairless pubic scars and depressions (Figs 31.2A, 31.3A). The large VY flap also advances thick, hair-bearing tissue onto the penis, which frequently creates an unnatural hump at the penile base and the appearance of a low-hanging penis.13–16 The penis can appear surrounded by the scrotum (scrotalization) with an overhanging large pubic fat pad, which makes the penis look shorter and hidden. A VY flap can also create ‘dog-ears’ at the distal scrotal flap incision. Smaller VY advancement flaps cause less frequent problems, but wound and aesthetic complications also occur.
Outcomes
An occasional patient may complain of penile shortening after release of the suspensory ligament. Since there is a dead space between the pubic symphysis and the corpora, it is possible for the corpora to reattach in a shortened position. This dead space can be filled by a proximal or distal based fat flap transposed from the medial spermatic cord (Fig. 31.4). However, most doctors tell the patients to stretch the penis after the release without filling the space.
Girth increase treatment
Fat injections
Autologous fat injections into the dartos fascia are still used by some physicians to increase penile thickness. The fat is moveable and gives a somewhat spongy texture to the penis. Less than 50% of injected fat normally survives in other parts of the body. Ideally, small amounts of fat (10–20 cc) are injected in multiple tunnels. Small amounts of total injected fat produce only minimal girth gain but do not have much risk of complications. Complications include asymmetry of the sides of the penis, nodules with bulging and concavities, and loss of penile rigidity due to an overabundance of fat (Figs 31.3, 31.5A).
Dermal and dermal fat grafts
Girth enlargement is also performed by inserting either dermal or dermal fat strips into the dartos fascia or by wrapping dermal fat sheets circumferentially between the dartos and Buck’s fascias.7–10 The strips can be placed through either a partial circumcision incision or a transverse pubic incision. The sheet graft, which is not commonly performed, is usually placed through a hemi-circumcision incision and wrapped about 80% of the circumference of the penis with the urethra left uncovered. The grafts are sutured proximally and distally to prevent migration. Usually, the dermal fat grafts ‘take’ well and provide circumference girth increase from 2–4 cm. However, difficulties with penile immobilization and the thickness of the grafts increase the risk of poor ‘take’ and subsequent severe complications such as restriction of erection with penile shortening or penile curvature. The procedure is far more invasive than fat injections and requires several hours of surgery. Donor site scars from the buttock crease, suprapubic region, or flanks can be very unsightly. Nodules and fat reabsorption are less common with dermal fat grafts than fat injections. Significant penile edema and induration exist for 6 weeks postoperation, and relatively normal texture returns in 4–6 months. Wrapping a sheet of dermal-fat grafts, rather than inserting strips, provides smooth texture with less risk of ridges and displacement. Penile skin loss has been seen with dermal fat grafts.
Allograft dermal matrix grafts
True corporal girth increase can be obtained by making lengthwise incisions through the tunica albuginea at the 3 and 9 o’clock locations and then patching these defects with Alloderm or long saphenous vein grafts.17 This procedure was derived from penile straightening operations for Peyronie’s disease. However, most of the results are anecdotal with no large series. The risk of erectile dysfunction is theoretically possible if infection or poor healing occurs, since the erectile chamber is violated.
Other techniques are being tried to increase girth by using tissue engineering with biodegradable scaffolds.18
Reconstruction of penile enlargements
Patients present with a diverse array of deformities and reconstructive issues.15,16 They may have a combination of penile lengthening with VY flaps and/or fat injections, or penile lengthening with Alloderm, etc. The patient must prioritize his reconstructive goals, because complete correction of all the deformities may not be possible at one operation, if at all. He may want only limited fat or Alloderm removal, partial or no VY flap reversal, or minimal scar revisions. Realistic expectations must be emphasized.
Reversal of VY advancement flap
The most common repair is partial or complete reversal of the VY advancement flap with excision of the wide scars (Figs 31.2, 31.3).14–16 Reversal and scar revision eradicates the unsightly dorsal penile hump and proximal penile hair-bearing tissue by re-draping the penis with the normal shaft skin. The penile skin is elevated to its normal position by aligning the hair on the ‘V’ flap with the pubic hair. The suprapubic concavity and unsightly scars are usually also corrected by partially or completely reversing the VY flap, excising scar tissue, mobilizing Scarpa’s fascia and skin from both sides of the vertical scar, and approximating the wound. Complete VY reversal resulting in a semicircular incision is ideal, but it is often impossible or undesirable. Part of the flap tip may have necrosed after the first procedure or must be excised on this revision to prevent tip flap loss. The patient may have had multiple circumcisions after fat injections stretched the penile skin. Therefore, the adequacy of shaft skin needs to be determined intraoperatively to insure that complete reversal of the flap does not shorten the penis (either real or illusory) and restrict an erection. A pharmacologic erection achieved by intracavernosal injection of Prostaglandin E1 helps to determine skin adequacy. No restriction of erection should occur by pulling on the erect penis. If there is inadequate penile skin for complete reversal, partial reversal is performed which results in an inverted Y-shaped scar with a shorter vertical limb (Figs 31.3B, 31.6). The resulting ‘Y’ scar is more noticeable than the scar from complete reversal.
Reversing the VY flap can cause scrotal ‘dog-ears’, which are usually followed along the lateral scrotum. The method of closure and ‘dog-ear’ excision is determined by judging the tightness of the penile skin, taking care not to restrict an erection. Do not eliminate skin discrepancy or ‘dog-ears’ by making a circular incision through the skin and dartos fascia at the penile base, since prolonged lymphedema or skin loss can occur. Alternatively, the ‘dog-ear’ is excised from the mid-portion on the lateral side of the incision, creating a lateral dart instead of following the ‘dog-ear’ medially around the penile base (Fig. 31.6).
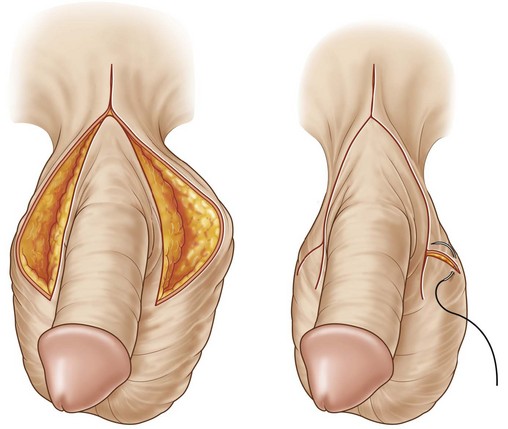
Re-release of the suspensory ligament is performed only if the patient complains of penile shortening, since the risk of injury to the dorsal neurovascular structures is increased. In order to prevent reattachment of the corpora bodies to the symphysis in a shortened position, a fat flap or flaps transposed from spermatic cord lipomatous tissue should be placed between the corpora and the pubic symphysis (Fig. 31.4).
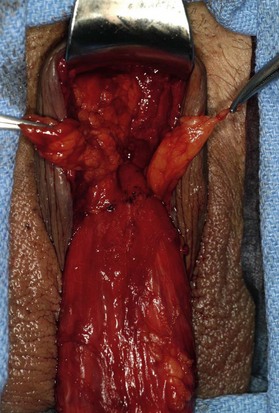
Fat removal
Most patients with fat injections do not want complete removal of the fat. They usually complain of nodules or penile asymmetry with various concavities or convexities. Removal of fat nodules and/or penile contouring is performed through a limited or complete circumcision incision, a medial raphe incision, or part of a previous VY incision (Fig. 31.5). Shaft incisions are cosmetically unacceptable and unnecessary. Deforming or firm fat deposits are removed first followed by contouring of the residual fat. Over-resection of fat creates unsightly concavities, so perform contouring by removing small increments of the deforming fat.
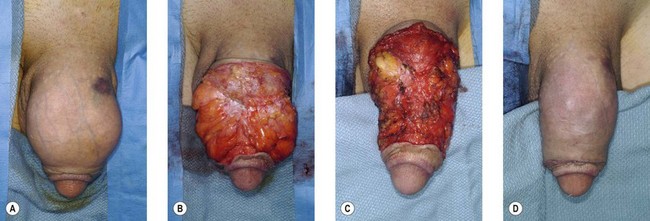
Dermal fat graft and Alloderm removal
Dermis, dermal fat grafts, and Alloderm present with a variety of different problems, including penile shortening, curvature, and areas of induration.3 Removal of the grafts are performed though one or a combination of circumcision, median raphe, or low pubic incisions. An indurated, scarred graft that is not adhered to the Buck’s fascia can be removed without much difficulty, thereby correcting the deformity (Fig. 31.7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree