Acne
Kristy F. Fleming
Murad Alam
I. BACKGROUND
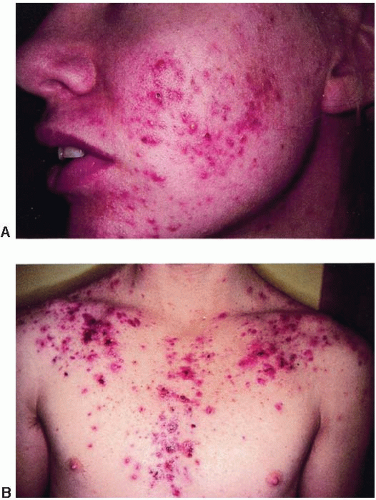
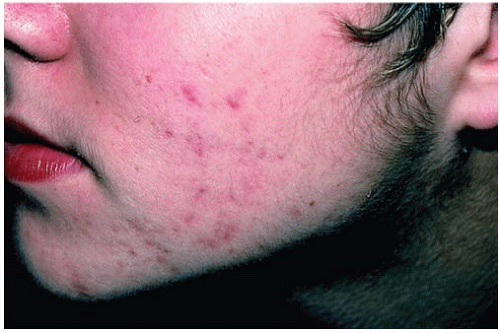
Acne vulgaris is a common, chronic disorder, involving inflammation of the pilosebaceous units that can be varied in presentation and difficult to treat. Acne pathogenesis derives from four main factors: sebaceous gland hyperplasia, abnormal follicular desquamation, Propionibacterium acnes, and inflammation. The primary lesion is the microcomedo, which may evolve into a noninflammatory comedo (open or closed) or become inflamed and form a papule, pustule, or nodule (Figs. 1-1 and 1-2).
Most adolescents (80%) experience some acne; however, it may linger into adulthood. Lesions may begin as early as ages 8 to 10 years at adrenarche, when androgens of adrenal origin begin to stimulate pilosebaceous units. Severe disease affects boys 10 times more frequently than girls, and patients often have a family history of severe cystic acne (Fig. 1-3).
Neonatal acne or cephalic pustulosis is self-limited with an onset around 2 to 3 weeks of age. Nearly one in five newborns is affected by at least mild neonatal acne characterized by erythematous nonscarring papules on the face and neck, most commonly on the cheeks and nasal bridge. This disorder spontaneously resolves within 1 to 3 months. Malassezia spp. have been implicated in the pathogenesis of neonatal acne. Topical 2% ketoconazole cream as well as benzoyl peroxide (BPO) has been shown to be effective treatments, although parental reassurance alone is often sufficient, given the transient and benign nature of the eruption.
Infantile acne usually presents at 3 to 6 months of age and includes persistent comedones and inflammatory lesions with an increased risk of scarring. Immature infantile adrenal glands lead to elevated dehydroepiandrosterone (DHEAS) levels until the age of 12 months. Boys are more often affected than girls because of additional high testosterone levels between the ages of 6 and 12 months. Infantile acne usually resolves within 1 to 2 years; however, individuals with infantile acne may have an increased risk of severe acne as teenager’s acne. Acne in mid-childhood is relatively uncommon and may be a marker for adrenal or gonadal tumors. Further workup of these patients is advised.
Early-onset acne may be the first sign of an underlying hormonal abnormality, especially if there is an associated advanced bone age and early pubic hair development. At puberty, hormonal stimuli lead to increased growth and development of sebaceous follicles. Female patients with severe acne or evidence of virilization often have abnormally high levels of circulating androgens. Several studies have demonstrated that many female patients with milder forms of acne and no evidence of virilization may still have ovarian and/or adrenal overproduction of androgens. In those patients with normal circulating levels of androgens, there is some evidence that suggests a heightened end-organ responsiveness of the sebaceous glands to androgenic stimulation. This heightened end-organ response may result in increased conversion of testosterone to
dihydrotestosterone and other 5-α-reduced metabolites or suppressed follicular testosterone metabolism. Male acne patients tend to have higher levels of androstenedione, testosterone, free androgen index, and 11-deoxycortisol.1
dihydrotestosterone and other 5-α-reduced metabolites or suppressed follicular testosterone metabolism. Male acne patients tend to have higher levels of androstenedione, testosterone, free androgen index, and 11-deoxycortisol.1
As many as one-third of adult women are affected by a low-grade acneiform eruption that may start de novo or merge imperceptibly with preexisting adolescent acne. The eruption may be induced by chronic exposure to
comedogenic substances such as isopropyl myristate, cocoa butter, and fatty acids present in some creams and moisturizers, by androgenic stimuli from progestins present in some oral contraceptives, by recent cessation of oral contraceptives, or by unknown causes.
comedogenic substances such as isopropyl myristate, cocoa butter, and fatty acids present in some creams and moisturizers, by androgenic stimuli from progestins present in some oral contraceptives, by recent cessation of oral contraceptives, or by unknown causes.
Inflammatory acne may yield both scarring and pigmentary changes. Early treatment is essential to prevent and minimize the cosmetic disfigurement associated with acne scarring. Adequate therapy will, in all cases, decrease its severity and may entirely suppress this disease.
II. CLINICAL PRESENTATION
Acne has a significant impact on the patient’s self-image and quality of life, and the psychological toll of acne may be comparable to that of asthma or epilepsy. Even clinically mild acne may
cause considerable social embarrassment to the patient. As with all medical and psychological conditions, the patient’s perception of the severity of the problem is an important factor in choosing treatment.
cause considerable social embarrassment to the patient. As with all medical and psychological conditions, the patient’s perception of the severity of the problem is an important factor in choosing treatment.
A. Noninflammatory Lesions. The initial lesion is the closed comedo; visible as a 1- to 2-mm white bump (whitehead) most easily seen when the skin is stretched. If follicle contents extrude, a 2- to 5-mm, dark-topped, open comedo (blackhead) results. Patients should be advised that this black material is simply oxidized keratin, not dirt.
B. Inflammatory Lesions. Erythematous papules, pustules, cysts, and abscesses may be seen. Patients with cystic acne also tend to show polyporous comedones, which result from prior inflammation during which epithelial scarring caused fistulous links between neighboring sebaceous units. Acne lesions are seen primarily on the face, but the neck, chest, shoulders, and back may be involved. One or more anatomic areas may be involved in any given patient, and the pattern of involvement, once present, tends to remain constant.
III. WORKUP
Several points regarding etiology or therapy should be considered with each patient:
A. Endocrine Factors. Sudden onset of acne, treatment-resistant acne, and acne associated with signs of androgynism should lead one to suspect an endocrine abnormality.
1. Acne Accompanied by Irregular Menstrual Periods or Concomitant Hirsutism. Men and women with mild-to-severe cystic acne, especially those who do not respond to conventional therapy, may have elevated plasma-free testosterone and/or DHEAS levels. Hyperandrogenism is associated with acne, hirsutism, alopecia, and menstrual irregularities; other possible findings include infertility, deepening of the voice, increased libido, acanthosis nigricans, insulin resistance, type 2 diabetes mellitus, and dyslipidemia. DHEAS elevations above 8,000 ng/mL suggest the presence of an adrenal tumor; a range of 4,000 to 8,000 ng/mL is indicative of congenital adrenal hyperplasia. Testosterone elevations point to an ovarian dysfunction, with levels of 150 to 200 ng/dL suggesting an ovarian tumor. Oral contraceptives can mask an underlying endocrine disorder, so testing should be done 1 month after the discontinuation of exogenous hormones. Women may have high normal levels of DHEAS and testosterone and may benefit from hormonal therapy. Postmenopausal acne occurs in some women with previously oily skin, with the development of small closed comedones at the periphery of the face; unopposed adrenal androgens are the presumed cause. See Table 1-1.
2. Premenstrual Flare-Up. Premenstrual flares of acne are associated with a narrowing of the sebaceous duct orifice between days 15 and 20 of the menstrual cycle. This can lead to duct obstruction and resistance to the flow of sebum. Many women tend to do well on anovulatory drugs.
3. Acne Associated with Oral Contraceptives. Acne may be associated with oral contraceptive pills if recently started or discontinued and if composed of an androgenic progesterone. During the first two or three cycles
on oral contraceptives, acne may worsen. Post-pill acne may continue for as long as a year after birth control pills are stopped. Although anovulatory drugs may provide excellent therapy for acne, the various pills differ enormously in their effect on the sebaceous gland. Oral contraceptives that contain the androgenic and antiestrogenic progestogens norgestrel and norethindrone acetate may actually provoke an acneiform eruption.
on oral contraceptives, acne may worsen. Post-pill acne may continue for as long as a year after birth control pills are stopped. Although anovulatory drugs may provide excellent therapy for acne, the various pills differ enormously in their effect on the sebaceous gland. Oral contraceptives that contain the androgenic and antiestrogenic progestogens norgestrel and norethindrone acetate may actually provoke an acneiform eruption.
TABLE 1-1 Endocrinopathies to Consider in Patient with Acne | |
|---|---|
|
B. Acne due to Occupational or Chemical Exposure. Exposure to heavy oils, greases, polyvinyl chloride, chlorinated aromatic hydrocarbons, and tars can cause acne. These occlusive comedogenic agents will initiate lesions, as can some greasy substances used for hair care (pomade acne). Certain oily or greasy cosmetics and creams can also exacerbate acne.
C. Acne due to Occlusive Clothing or Habits. Mechanical trauma (pressure, friction, rubbing, and squeezing) from clothing or athletic wear or from behavioral habits will also cause lesions. For example, football players may develop acne lesions in the distribution of their helmet and chin strap.
D. Medications-Induced Acne. Drug-induced acne often presents as an abrupt, monomorphous eruption of inflammatory papules. The most prominent among these are corticosteroids, adrenocorticotropic hormone, phenytoin, androgens, anabolic steroids (danazol and testosterone), epidermal growth factor receptor inhibitors, and melanoma chemotherapy agents such as Vemurafenib. Other known stimuli include trimethadione, isoniazid, lithium, iodides, bromides, halothane, vitamin B12, cobalt irradiation, and hyperalimentation therapy.
E. Rapid-Onset Acne Associated with Fever and Leukocytosis. Acne fulminans is a destructive arthropathy, resembling rheumatoid arthritis. SAPHO syndrome consists of synovitis, acne, pustulosis (palmar-plantar pustular psoriasis), hyperostoses, and osteitis; this is considered one of the spondyloarthropathies and has been reported with inflammatory bowel disease (IBD) and pyoderma gangrenosum. The PAPA syndrome, an autosomal dominant disorder, consists of pyogenic sterile arthritis, pyoderma gangrenosum, and acne.
F. Antibiotic-Resistant Acne. There is an increased incidence of bacterial resistance of both P. acnes and coagulase-negative Staphylococcus aureus noted after long-term antibiotic use. These resistant bacteria are found in both the patients and their close contacts. Propionibacterium acnes resistance to antibiotics should be considered in treatment failures. This is seen particularly with erythromycin; but cross-resistance can occur with clindamycin. Multiple antibiotics should not be used at the same time and BPOs should be added as a second agent to help minimize this possibility. The highest possible dose of an oral antibiotic should be started for as short a course as possible. Oral minocycline has the lowest risk of bacterial resistance over time. Oral isotretinoin reduces the total number of resistant P. acnes.
An unusual complication of chronic broad-spectrum antibiotic therapy is the development of a gram-negative folliculitis. Such patients will notice a sudden change in their acne, with the appearance of pustules or large inflammatory cysts that, on culture, usually grow Proteus, Pseudomonas, or Klebsiella species. Because acne cysts are sterile on routine bacteriologic culture, a sudden change in morphology warrants Gram stain and culture of cyst/abscess contents. This condition is treated with isotretinoin or the appropriate antibiotic determined from culture and sensitivity testing.
IV. TREATMENT
Acne therapy must take into consideration a multitude of factors. Often multiple therapeutic agents are used simultaneously or on a rotation schedule depending on patient response and side effects. The treatment of acne is a dynamic process and must always include the patient’s subjective evaluation of his or her appearance and symptoms.
A. Topical Retinoids




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree