Severe and Life-Threatening Skin Eruptions in the Acutely III Patient 
Epidemiology
Age of Onset. Usually >50 years; in children, EES usually results from atopic dermatitis.
Sex. Males > females.
Etiology
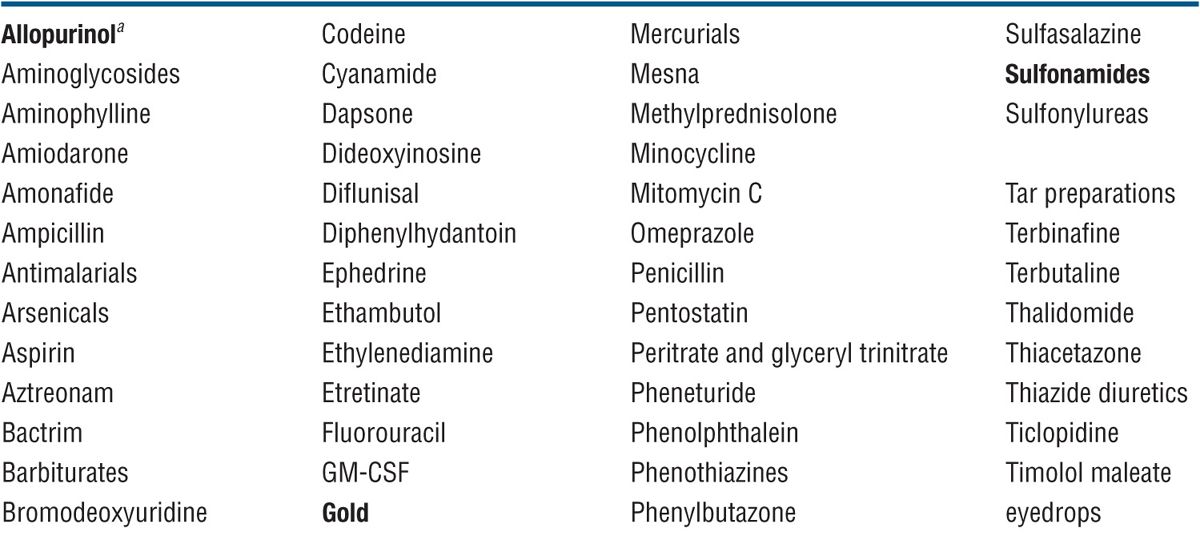
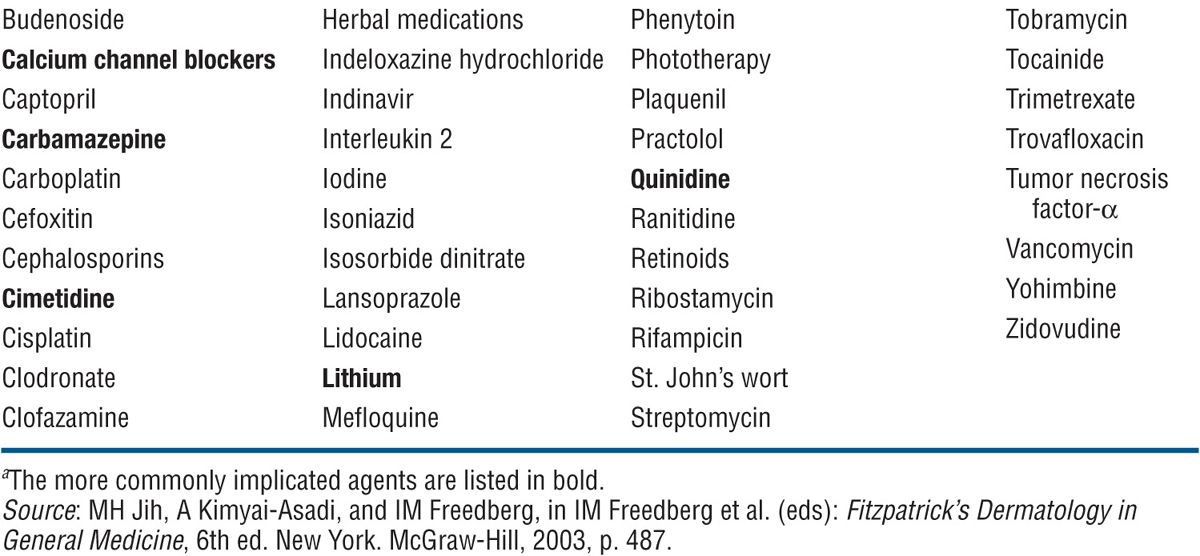
Some 50% of patients have history of preexisting dermatosis. Most frequent are psoriasis, atopic dermatitis, adverse cutaneous drug reactions, cutaneous T-cell lymphoma (CTCL), allergic contact dermatitis, and pityriasis rubra pilaris (Table 8-1). Drugs most commonly implicated in EES are shown in Table 8-2. In 20% of patients, it is not possible to identify the cause.
TABLE 8-1 ETIOLOGY OF EXFOLIATIVE DERMATITIS IN ADULTS
TABLE 8-2 DRUGS THAT CAUSE EXFOLIATIVE DERMATITIS
Pathogenesis
The metabolic response to EES may be profound. Large amounts of warm blood are present in the skin due to the dilatation of capillaries, resulting in considerable heat dissipation. Also, there may be high-output cardiac failure; the loss of scales (and thus proteins) through exfoliation can be considerable, up to 9 g/m2 of body surface per day.
Clinical Manifestation
Depending on the etiology, the acute phase may develop rapidly, usually in a drug reaction, or psoriasis. At this early acute stage, it is still possible to identify the preexisting dermatosis. There is fever, pruritus, fatigue, weakness, anorexia, weight loss, malaise, feeling cold, and shivers.
Appearance of Patient. Frightened, red, “toxic,” may be malodorous.
Skin lesions. Skin is red, thickened, scaly. Dermatitis is uniform involving the entire body surface (Figs. 8-1 to 8-3), except for pityriasis rubra pilaris, where EES spares sharply defined areas of normal skin (see Fig. 3-17). Thickening leads to exaggerated skin folds (Figs. 8-2 and 8-3); scaling may be fine and branny and may be barely perceptible (Fig. 8-2) or large, up to 0.5 cm, and lamellar (Fig. 8-1).
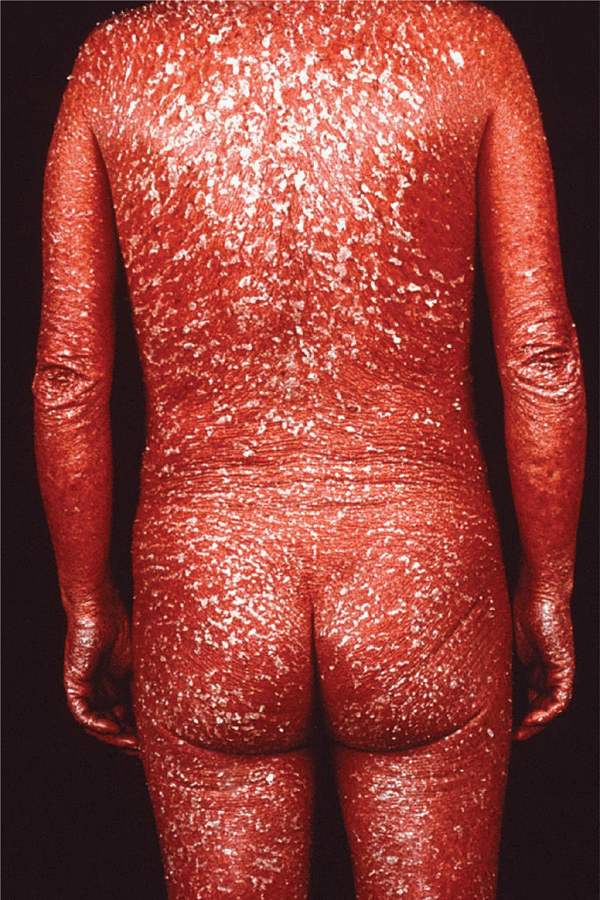
Figure 8-1. Exfoliative dermatitis: psoriasis There is universal erythema, thickening of the skin, and heavy scaling. This patient had psoriasis as suggested by the large silvery white scales and the scalp and nail involvement not seen in this illustration. The patient had fatigue, weakness, malaise, and was shivering. It is quite obvious that such massive scaling can lead to protein loss and the maximal dilatation of skin capillaries to considerable heat dissipation and high-output cardiac failure.
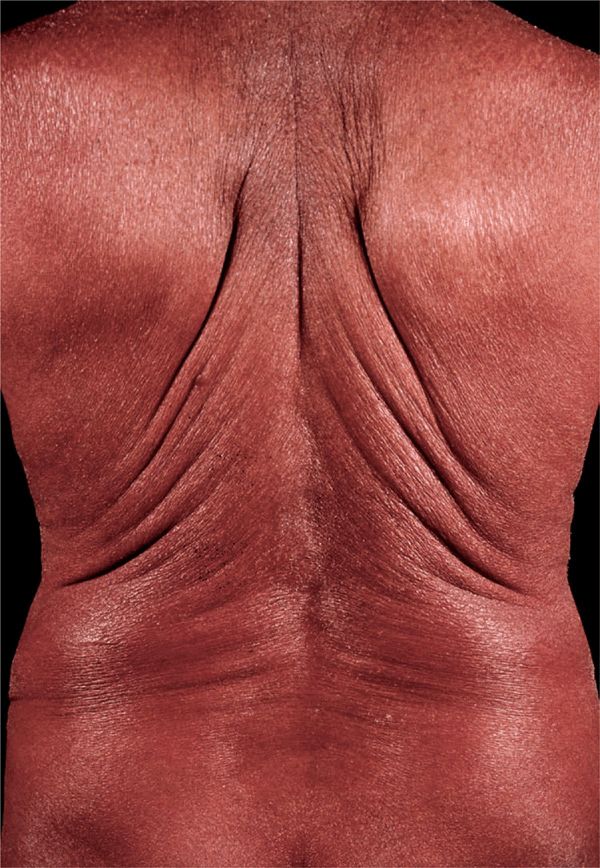
Figure 8-2. Exfoliative dermatitis: drug induced This is generalized erythroderma with thickening of skin resulting in increased skin folds, universal redness, a fine brawny scaling. This patient had developed erythroderma following the injection of gold salts for rheumatoid arthritis.
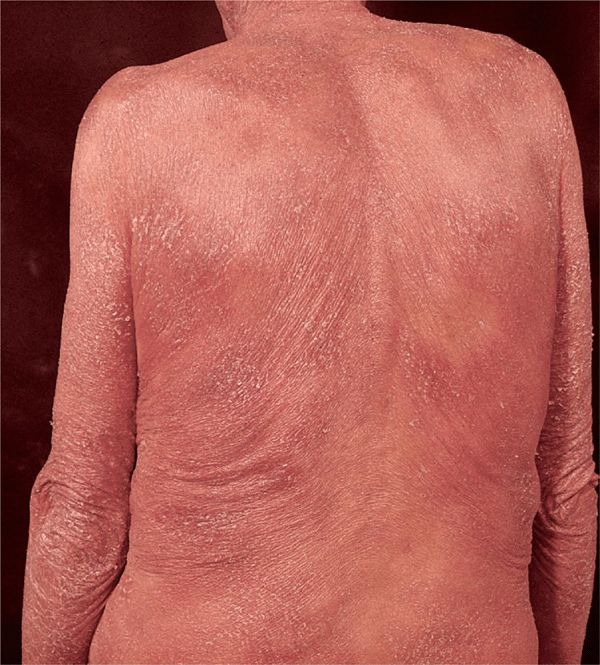
Figure 8-3. Exfoliative dermatitis: cutaneous T-cell lymphoma There is universal erythema, thickening, and scaling. Note that in contrast to erythroderma shown in Figs. 8-1 and 8-2, the degree of erythema and thickness is not uniform and the redness has a brownish hue. In addition, this elderly patient had hair loss, massive involvement of palms and soles with diffuse hyperkeratoses, cracks, and fissures. Generalized lymphadenopathy was also present.
Palms and Soles. Usually involved, with massive hyperkeratosis and deep fissures in pity-riasis rubra pilaris, Sézary syndrome, and psoriasis.
Hair. Telogen effluvium, even alopecia, except for EES arising in eczema or psoriasis.
Nails. Thickening of nail plates, onycholysis, shedding of nails.
Pigmentation. In chronic EES, there may be hyperpigmentation or patchy loss of pigment in patients whose normal skin is brown or black.
General Examination
Lymph nodes generalized, rubbery, and usually small; enlarged in Sézary syndrome. Edema of lower legs and ankles.
Laboratory Examinations
Chemistry. Low serum albumin and increase in gammaglobulins; electrolyte imbalance; acute-phase proteins increased.
Hematology. Leukocytosis.
Bacterial Culture. Skin: rule out secondary Staphylococcus aureus infection. Blood: rule out sepsis.
Dermatopathology. Depends on type of underlying disease. In all there is parakeratosis, inter- and intracellular edema, acanthosis with elongation of the rete ridges, and exocytosis of cells, edema of the dermis, and an inflammatory infiltrate.
Imaging. CT scans or MRI should be used to find evidence of lymphoma.
Lymph Node Biopsy. When there is suspicion of lymphoma.
Diagnosis
The history of the preexisting dermatosis may be the only clue. Also, pathognomonic signs and symptoms of the preexisting dermatosis may help, e.g., dusky-red color in psoriasis (Fig. 8-1) and yellowish red in pityriasis rubra pilaris (see Fig. 3-17); typical nail changes of psoriasis; lichenification, erosions, and excoriations in atopic dermatitis and eczema; diffuse, relatively nonscaling palmar hyperkeratoses with fissures in CTCL and pityriasis rubra pilaris; sharply demarcated patches of noninvolved skin within the erythroderma in pityriasis rubra pilaris; massive hyperkeratotic scale of scalp, usually without hair loss in psoriasis and with hair loss in CTCL and pityriasis rubra pilaris; in the latter and in CTCL, ectropion may occur.
Course and Prognosis
Guarded, depends on underlying etiology. Patients may succumb to infections or, if they have cardiac problems, to cardiac failure (high-output failure) or, as was unfortunately often the case in the past, to the effects of prolonged glucocorticoid therapy.
Management
This important medical problem should be dealt with in a modern inpatient dermatology facility with experienced personnel. The patient should be hospitalized in a single room, at least for the beginning workup and during the development of a therapeutic program. The hospital room conditions (heat and cold) should be adjusted to the patient’s needs; most often, these patients need a warm room with many blankets.
Topical. Water baths with added bath oils, followed by application of bland emollients.
Systemic. Oral glucocorticoids for remission induction but not for maintenance; systemic and topical therapy as required by underlying condition.
Supportive. Supportive cardiac, fluid, electrolyte, protein replacement therapy as required.
 EES is a serious, at times life-threatening, reaction pattern of the skin characterized by a uniform redness, infiltration, and scaling involving practically the entire skin.
EES is a serious, at times life-threatening, reaction pattern of the skin characterized by a uniform redness, infiltration, and scaling involving practically the entire skin. It is associated with fever, malaise, shivers, and generalized lymphadenopathy.
It is associated with fever, malaise, shivers, and generalized lymphadenopathy. Two stages, acute and chronic, merge one into the other. In the acute and subacute phases, there is rapid onset of generalized vivid red erythema and fine branny scales; the patient feels hot and cold, shivers, and has fever. In chronic EES, the skin thickens, and scaling continues and becomes lamellar.
Two stages, acute and chronic, merge one into the other. In the acute and subacute phases, there is rapid onset of generalized vivid red erythema and fine branny scales; the patient feels hot and cold, shivers, and has fever. In chronic EES, the skin thickens, and scaling continues and becomes lamellar. There may be loss of scalp and body hair, and the nails become thickened and separated from the nail bed (onycholysis).
There may be loss of scalp and body hair, and the nails become thickened and separated from the nail bed (onycholysis). There may be hyperpigmentation or patchy loss of pigment in patients whose normal skin color is brown or black.
There may be hyperpigmentation or patchy loss of pigment in patients whose normal skin color is brown or black. The most frequent preexisting skin disorders are (in order of frequency) psoriasis, atopic dermatitis, adverse cutaneous drug reaction, lymphoma, allergic contact dermatitis, and pityriasis rubra pilaris.
The most frequent preexisting skin disorders are (in order of frequency) psoriasis, atopic dermatitis, adverse cutaneous drug reaction, lymphoma, allergic contact dermatitis, and pityriasis rubra pilaris.








