Genetic Diseases 
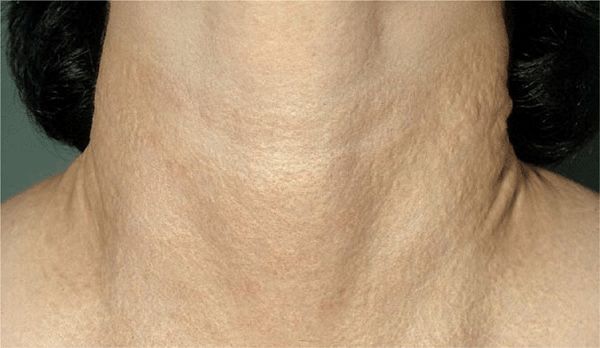
Figure 16-1. Pseudoxanthoma elasticum Multiple, confluent, chamois-colored or yellow papules (pseudoxanthomatous) create a large, circumferential, pebbled plaque on the neck of a 32-year-old woman. Changes in the connective tissue in this condition lead to excessive folds on the lateral neck.
Epidemiology
Incidence. In mental institutions, 1:100 to 1:300; in general population, 1:20,000 to 1:100,000.
Age of Onset. Infancy.
Sex. Equal incidence.
Race. All races.
Heredity. Autosomal dominant. TS is caused by mutations in a tumor-suppressor gene, either TSCS1 or TSCS2. TSCS1 maps to chromosome 9q34. TSCS2 maps to 16p13.3.
Pathogenesis
Genetic alterations of ectodermal and mesodermal cells with hyperplasia, with a disturbance in embryonic cellular differentiation.
Clinical Manifestation
White macules are present at birth or appear in infancy (>80% occur by 1 year of age, 100% appear by 2 years); >20% of angiofibromata are present at 1 year of age, 50% occur by 3 years. Seizures (infantile spasms) occur in 86%; the earlier the onset of seizures, the worse the mental retardation. Mental retardation (49%).
Skin Lesions. 96% incidence.
Hypomelanotic Macules. “Off-white”; one or many, usually more than three. Polygonal or “thumbprint,” 0.5–2 cm; lance ovate or “ash-leaf” spots (Fig. 16-2), 3–4 cm (up to 12 cm); tiny white “confetti” macules, 1–2 mm (Fig. 16-3). White macules occur on trunk (>), lower extremities (>), upper extremities (7%), head and neck (5%). White macules shine up with Wood light (Fig. 16-2B)

Figure 16-2. Tuberous sclerosis: ash-leaflet hypopigmented macules (A) Three well-demarcated, elongated (ash-leaflet shaped), hypomelanotic macules on the lower leg of a child with tan skin. (B) Ash-leaflet hypomelanotic macules in pale skin are better visualized under Wood light where they light up.

Figure 16-3. Tuberous sclerosis: “confetti” macules Multiple, discrete, small, confetti-like, hypopigmented macules of variable size on the leg. These lesions are pathognomonic.
Angiofibromas. 0.1–0.5 cm, dome-shaped and smooth, exhibiting red or skin color (Fig. 16-4). Occur in the center of the face. They are firm and disseminated but may coalesce; termed adenoma sebaceum but represent angiofibromas (present in 70%).

Figure 16-4. Tuberous sclerosis: angiofibromas Confluent, small, angiomatous (erythematous, glistening) papules on the cheek and nose. These lesions were not present during the first few years of life; appeared only after the age of 4 years.
Plaques. Represent connective tissue nevi (“shagreen” patch), present in 40%; skin colored; occur on the back and buttocks (Fig. 16-5B).
Figure 16-5. Tuberous sclerosis: (A) Periungual fibroma (Koenen tumor). (B) Shagreen patch, slightly elevated, skin colored. This represents a connective tissue nevus.
Periungual Papules or Nodules. Ungual fibromas (Koenen tumors) present in 22%, arise late in childhood, and have the same pathology (angiofibroma) as the facial papules (Fig. 16-5A).
Associated Systems
CNS (tumors producing seizures), eye (gray or yellow retinal plaques, 50%), heart (benign rhabdomyomas), hamartomas of mixed cell type (kidney, liver, thyroid, testes, and GI system).
Laboratory Examinations
Dermatopathology. White Macules. Decreased number of melanocytes, decreased melano-some size, decreased melanin in melanocytes and keratinocytes.
Angiofibromata. Proliferation of fibroblasts, increased collagen, angioneogenesis, capillary dilatation, absence of elastic tissue.
Brain Pathology. “Tubers” are gliomas.
Imaging. Skull X-Ray. Multiple calcific densities.
CT Scan. Ventricular deformity and tumor deposits along the striothalamic borders.
MRI. Subependymal nodules.
Electroencephalography. Abnormal.
Renal Ultrasound. Reveals renal hamartoma.
Diagnosis
More than five ash leaf macules (Fig. 16-2) in an infant are highly suggestive. Confetti spots (Fig. 16-2) are virtually pathognomonic. Evaluate the patient with a study of the family members and by obtaining various types of imaging as well as electroencephalography. Mental retardation and seizures may be absent.
Differential Diagnosis
White Spots. Focal vitiligo, nevus anemicus, tinea versicolor, nevus depigmentosus, postinflammatory hypomelanosis.
Angiofibromas. Tricholemmoma, syringoma, skin-colored papules on the face, dermal nevi.
Note: angiofibromata of the face (Fig. 16-4) have been mistaken for and treated as acne vulgaris or rosacea.
Periungual Fibromas. Verruca vulgaris.
Course and Prognosis
A serious autosomal disorder that causes major problems in behavior, because of mental retardation, and in therapy, to control the serious seizure problem present in many patients.
In severe cases, 30% die before the fifth year of life, and 50–75% die before reaching adult age. Malignant gliomas are not uncommon. Genetic counseling is imperative.
Management
Prevention. Counseling.
Treatment. Laser surgery for angiofibromas.
Support organization: http://www.support-group.com
 ICD-10: Q82.810
ICD-10: Q82.810 
 Pseudoxanthoma elasticum (PXE) is a serious hereditary disorder of connective tissue that involves the elastic tissue in the skin, blood vessels, and eyes. Autosomal recessive (most common) and autosomal dominant. Incidence: 1:40,000 to 1:100,000.
Pseudoxanthoma elasticum (PXE) is a serious hereditary disorder of connective tissue that involves the elastic tissue in the skin, blood vessels, and eyes. Autosomal recessive (most common) and autosomal dominant. Incidence: 1:40,000 to 1:100,000. Etiology and Pathogenesis: Pathogenic mutation in the ABCC6 gene, which encodes MRP6, a member of the ATPase-dependent transmembrane transporter family of proteins. MRP6 can serve as an efflux pump transporting small-molecular-weight glutathione conjugates, which may facilitate calcification of elastic fibers.
Etiology and Pathogenesis: Pathogenic mutation in the ABCC6 gene, which encodes MRP6, a member of the ATPase-dependent transmembrane transporter family of proteins. MRP6 can serve as an efflux pump transporting small-molecular-weight glutathione conjugates, which may facilitate calcification of elastic fibers. The principal skin manifestations are a distinctive peau d’ orange surface pattern resulting from closely grouped clusters of yellow (chamois-colored) papules in a reticular pattern on the neck, axillae, and other body folds (
The principal skin manifestations are a distinctive peau d’ orange surface pattern resulting from closely grouped clusters of yellow (chamois-colored) papules in a reticular pattern on the neck, axillae, and other body folds ( The effects on the vascular system include GI hemorrhage, hypertension occurring in young persons and resulting from involvement of renal arteries, and claudication.
The effects on the vascular system include GI hemorrhage, hypertension occurring in young persons and resulting from involvement of renal arteries, and claudication. Ocular manifestations (“angioid” streaks and retinal hemorrhages) can lead to blindness.
Ocular manifestations (“angioid” streaks and retinal hemorrhages) can lead to blindness. Dermatopathology: Biopsy of a scar can detect characteristic changes of PXE before typical skin changes are apparent. Swelling and irregular clumping and basophilic staining of elastic fibers, elastic fibers appear curled and “chopped up,” with calcium deposition.
Dermatopathology: Biopsy of a scar can detect characteristic changes of PXE before typical skin changes are apparent. Swelling and irregular clumping and basophilic staining of elastic fibers, elastic fibers appear curled and “chopped up,” with calcium deposition. Imaging: X-ray—extensive calcification of the peripheral arteries of the lower extremities. Arteriography of symptomatic vessels.
Imaging: X-ray—extensive calcification of the peripheral arteries of the lower extremities. Arteriography of symptomatic vessels. The course is inexorably progressive. Gastric artery hemorrhage → hematemesis. Peripheral vascular disease → cerebrovascular accidents, atherosclerosis obliterans, or bowel angina. Pregnancies are complicated by miscarriage, cardiovascular complications. Blindness. Life span is often shortened due to myocardial infarction or massive GI hemorrhage.
The course is inexorably progressive. Gastric artery hemorrhage → hematemesis. Peripheral vascular disease → cerebrovascular accidents, atherosclerosis obliterans, or bowel angina. Pregnancies are complicated by miscarriage, cardiovascular complications. Blindness. Life span is often shortened due to myocardial infarction or massive GI hemorrhage. Management: Genetic counseling. Evaluate family members for PXE. Regular reevaluation by primary care physician and ophthalmologist is mandatory.
Management: Genetic counseling. Evaluate family members for PXE. Regular reevaluation by primary care physician and ophthalmologist is mandatory. Support organization: PXE International,
Support organization: PXE International,  ICD-10: Q85.1
ICD-10: Q85.1 
 Tuberous sclerosis is an autosomal-dominant disease arising from a genetically programmed hyperplasia of ectodermal and mesodermal cells and manifested by a variety of lesions in the skin, CNS (hamartomas), heart, kidney, and other organs.
Tuberous sclerosis is an autosomal-dominant disease arising from a genetically programmed hyperplasia of ectodermal and mesodermal cells and manifested by a variety of lesions in the skin, CNS (hamartomas), heart, kidney, and other organs. The principal early manifestations are the triad of seizures, mental retardation, and congenital white spots.
The principal early manifestations are the triad of seizures, mental retardation, and congenital white spots. Facial angiofibromata are pathognomonic but do not appear until the third or fourth year.
Facial angiofibromata are pathognomonic but do not appear until the third or fourth year.








