Disorders of Psychiatric Etiology 
Classification of Disorders of Psychiatric Etiology
• Dysmorphic syndrome
• Delusions of parasitosis
• Compulsive habits
• Neurotic excoriations
• Trichotillomania
• Factitious syndromes
• Cutaneous signs of injecting drug use

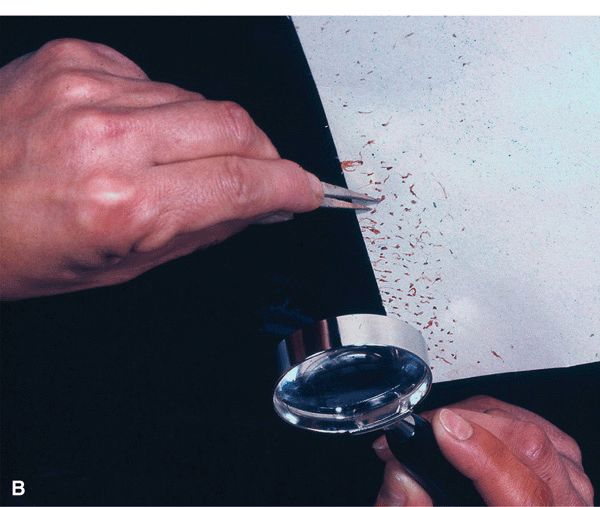
Figure 24-1. Delusions of parasitosis (A) Usually patients collect small pieces of debris from their skin by scratching with their nails or an instrument and submit them to the doctor for examination for parasites. In this case, pointed tweezers were used and the results are ulcers, crusted lesions, and scars. (B) Occasionally, this can progress to an aggressive behavior such as depicted in this case where the patient posed to demonstrate how she collects the “parasites” from her skin on a piece of paper. In the majority of cases, patients are not dissuaded from their monosymptomatic delusion.
 ICD-10: F45.2
ICD-10: F45.2 
 Patients with dysmorphic syndrome regard their image as distorted in the eyes of the public; this becomes almost an obsession.
Patients with dysmorphic syndrome regard their image as distorted in the eyes of the public; this becomes almost an obsession. The patient with BDS does not consult a psychiatrist but a dermatologist or plastic surgeon. The typical patient with BDS is a single, female, young adult who is an anxious and unhappy person.
The patient with BDS does not consult a psychiatrist but a dermatologist or plastic surgeon. The typical patient with BDS is a single, female, young adult who is an anxious and unhappy person. Common dermatologic complaints are facial (wrinkles, acne, scars, hypertrichosis, dry lips), scalp (incipient baldness, increased hair growth), genital (normal sebaceous glands on the penis, red scrotum, red vulva, vaginal odor), hyperhidrosis, and bromhidrosis.
Common dermatologic complaints are facial (wrinkles, acne, scars, hypertrichosis, dry lips), scalp (incipient baldness, increased hair growth), genital (normal sebaceous glands on the penis, red scrotum, red vulva, vaginal odor), hyperhidrosis, and bromhidrosis. Management is a problem. One strategy is for the dermatologist to agree with the patient that there is a problem and thus establish rapport; in a few visits, the complaint can be explored and further discussed.
Management is a problem. One strategy is for the dermatologist to agree with the patient that there is a problem and thus establish rapport; in a few visits, the complaint can be explored and further discussed. If the patient and physician do not agree that the complaint is a vastly exaggerated skin or hair change, then the patient should be referred to a psychiatrist; this latter plan is usually not accepted, in which case the problem may persist indefinitely.
If the patient and physician do not agree that the complaint is a vastly exaggerated skin or hair change, then the patient should be referred to a psychiatrist; this latter plan is usually not accepted, in which case the problem may persist indefinitely. ICD-10: F22.0
ICD-10: F22.0 
 This rare disorder, which occurs in adults and is present for months or years, is associated with pain or paresthesia and is characterized by the presence of numerous skin lesions, mostly excoriations, which the patient truly believes are the result of a parasitic infestation (
This rare disorder, which occurs in adults and is present for months or years, is associated with pain or paresthesia and is characterized by the presence of numerous skin lesions, mostly excoriations, which the patient truly believes are the result of a parasitic infestation ( The onset of the initial pruritus or paresthesia may be related to xerosis or, in fact, to a previously treated infestation.
The onset of the initial pruritus or paresthesia may be related to xerosis or, in fact, to a previously treated infestation. Patients pick with their fingernails or dig into their skin with needles or tweezers to remove the “parasites” (
Patients pick with their fingernails or dig into their skin with needles or tweezers to remove the “parasites” ( It is important to rule out other causes of pruritus. This problem is serious; patients truly suffer and are opposed to seeking psychiatric help. Patients may sell their houses to move away from the offending parasite.
It is important to rule out other causes of pruritus. This problem is serious; patients truly suffer and are opposed to seeking psychiatric help. Patients may sell their houses to move away from the offending parasite. The patient should see a psychiatrist for at least one visit and for recommendations of drug therapy: pimozide plus an antidepressant. Treatment is difficult and usually unsuccessful.
The patient should see a psychiatrist for at least one visit and for recommendations of drug therapy: pimozide plus an antidepressant. Treatment is difficult and usually unsuccessful. ICD-10: L98.1
ICD-10: L98.1 
 Neurotic excoriations are not an uncommon problem, occurring more in females than in males and in the third to fifth decades.
Neurotic excoriations are not an uncommon problem, occurring more in females than in males and in the third to fifth decades. They may relate the onset to a specific event or to chronic stress; patients deny picking and scratching.
They may relate the onset to a specific event or to chronic stress; patients deny picking and scratching. The clinical lesions are an admixture of several types of lesions, principally excoriations, all produced by habitual picking of the skin with the fingernails; most common on the face (
The clinical lesions are an admixture of several types of lesions, principally excoriations, all produced by habitual picking of the skin with the fingernails; most common on the face ( The lesions are located only on sites that the hands can reach, thus often sparing the center of the back.
The lesions are located only on sites that the hands can reach, thus often sparing the center of the back. The diagnosis can be deceptive, and what prima facie appears to be neurotic excoriations could be a serious cause of pruritus.
The diagnosis can be deceptive, and what prima facie appears to be neurotic excoriations could be a serious cause of pruritus. Psychiatric guidance may be necessary if the problem is not solved, as it can be very disfiguring on the face and disruptive to the patient and the family. The course is prolonged, unless life adjustments are made.
Psychiatric guidance may be necessary if the problem is not solved, as it can be very disfiguring on the face and disruptive to the patient and the family. The course is prolonged, unless life adjustments are made. Pimozide has been helpful but must be used with caution and with the advice and guidance of a psychopharmacologist. Also, antidepressant drugs may be used.
Pimozide has been helpful but must be used with caution and with the advice and guidance of a psychopharmacologist. Also, antidepressant drugs may be used. Trichotillomania is a compulsive desire or habit to pluck hair. Can be on the scalp or any other hairy region (e.g., beard). Confluence of areas with very short sparse hairs, small bald areas, and normal area of scalp (
Trichotillomania is a compulsive desire or habit to pluck hair. Can be on the scalp or any other hairy region (e.g., beard). Confluence of areas with very short sparse hairs, small bald areas, and normal area of scalp (








