Abstract
Fractures of the distal forearm are among the most common injuries treated by orthopaedic surgeons and hand surgeons. This chapter begins with distal radius fractures, first reviewing the epidemiology, classification, and evaluation. The operative indications and subsequent techniques are then discussed, focusing on important points of each treatment. Although open reduction and internal fixation is the most common operative treatment, there are many other modalities to be considered as well. Also included is a section on operative considerations of certain fracture patterns such as volar ulnar corner injuries and how they differ in management. Finally, the complications associated with distal radius fractures are reviewed.
Fractures of the distal ulna are discussed next. Although often seen in combination with distal radius fractures, ulnar fractures can occur in isolation. Again evaluation, classification, and management are reviewed, including a discussion of the controversy involving when to fix ulnar styloid fractures associated with a distal radius injury.
Lastly, Galleazzi fractures, or fractures of the distal radius with disruption of the distal radioulnar joint (DRUJ), are reviewed. The biomechanics of the DRUJ as well as appropriate imaging to help detect injury are discussed. In adults, Galleazzi fractures are invariably treated with surgery.
8 Fractures and Dislocations of the Distal Radius and Ulna
I. Distal Radius Fractures
A. Epidemiology
Distal radius fractures are one of the most common fractures encountered by hand/ upper extremity surgeons.
In 2000, there were 1.7 million osteoporotic fractures of the forearm, followed by 1.6 million hip fractures. 1
Occur in a 4:1 female to male ratio. 1
They carry a significant cost of treatment burden. In 2007, Medicare paid $170 million for distal radius fractures. 2
As with many other fractures, they occur in a bimodal age distribution with higher energy injuries occurring in younger patients and lower energy osteoporotic fractures occurring in the elderly.
Distal radius fractures are important to recognize as they are predictors of subsequent osteoporotic fractures. 3
The relative risk of a hip fracture is 1.54 in women and 2.27 in men with osteoporotic distal radius fractures. 4
B. Evaluation
As with all fractures, a thorough history and neurovascular/skin examination is paramount.
Median nerve dysfunction is the most common nerve injury as a consequence of its proximity to the distal radius. 5
The median nerve lies closer to the radius as it travels more distally and is estimated to be 3 mm or so from the bone at the level of the wrist. 6
Incidence of acute carpal tunnel syndrome requiring decompression is estimated to be 3 to 9%. 5 , 7
All patients should be asked about any history of carpal tunnel syndrome and any new/acute symptoms accompanying the injury.
Imaging evaluation includes initial posteroanterior, lateral, and supplemental oblique X-rays.
Postreduction X-rays may include a modified lateral projection with the beam angled 10 degrees proximally to evaluate the reduction of the articular surface. 8
Medoff published average radiographic parameters of the distal radius from a sample size of 40, including radial inclination (23.6 degrees), radial height (11.6 degrees), and volar tilt (11.2 degrees). 8 The normal radiographic parameters of the distal radius are shown in ► Fig. 8.1 (normal wrist X-ray with overlying parameters).
Forearm X-rays should also be included to evaluate the elbow as well.
It is important to inspect the distal radioulnar joint (DRUJ) to assess for concomitant injury.
Lafontaine described criteria associated with unstable distal radius fractures which are therefore at risk of secondary displacement after reduction (► Table 8.1). 9

Degree of dorsal displacement |
Associated ulnar styloid fracture |
Age >60 years |
Dorsal comminution |
Intra-articular involvement |
C. Classification
Historically there have been many published classification systems of distal radius fractures as listed in ► Table 8.2. 10 Details of each of these systems are beyond the scope of this chapter.
For research purposes, the AO/Universal classification is most widely used today.
Clinically, a descriptive classification of the fracture is often sufficient.
Gartland and Werley | Lidstrom | Older and Colleagues |
Thomas | Malone | Jenkins |
McMurtry and Jupiter | Universal/AO | Mayo Clinic |
Fernandez |
D. Treatment
1. Nonoperative Treatment
Nondisplaced fractures are likely inherently stable and can be treated with removable bracing for protection.
Closed reduction and splinting is indicated as the initial management for all displaced distal radius fractures presenting to the emergency room.
Although controversial, evidence suggests that lower demand and/or elderly patients with mild residual deformity after closed reduction may still do well with nonoperative management in a cast.
The American Academy of Orthopaedic Surgeons (AAOS) guidelines are unable to recommend for or against operative treatment in patients older than 55. 11
Chung et al found elderly patients tend to do well with either open reduction internal fixation (ORIF) or casting; however, ORIF was estimated to be seven times more expensive. 12
Casting techniques: The Cotton-Loder position of wrist flexion and ulnar deviation should be avoided as this has been shown to increase carpal tunnel pressure.
Gelberman et al showed increasing carpal tunnel pressure to 47 mmHg at 40 degrees of wrist flexion. 13
The AAOS guidelines recommend weekly radiographic follow-up for 3 weeks after injury to evaluate for fracture displacement. 11
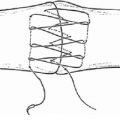
2. Closed Reduction and Percutaneous Pinning
In young patients with extra-articular fractures, pinning alone is an option.
Trumble et al demonstrated good results with pinning in fractures with comminution of only one cortex in young patients. Supplementary external fixation was required if comminution extended to two or more cortices. 14
In older patients with extra-articular and/or minimally displaced intra-articular fractures, pinning is also an option; however, it requires supplemental external or internal fixation. 14
External fixation or internal bridging plate depends on the ligamentaxis to hold reduction. 15
3. External Fixation
Agee helped to popularize the idea of using an external fixator to achieve fracture reduction via multiplanar ligamentotaxis. 15
External fixation is often useful in situations with significant soft tissue compromise, polytrauma, highly comminuted articular fractures, etc.
4. Bridge Plating
Hanel et al popularized bridge plating to act as an internal fixator (vs. external) for distal radius fractures. 16
Indications include high energy fractures with extension into the radial metaphysis and polytrauma patients requiring early use of the upper extremities.
Although the original technique involved using a 3.5-mm plate on the floor of the 4th dorsal compartment to the 3rd metacarpal, 17 Hanel et al published a modification using either a Synthes 2.4 mm distal radius bridge plate or mandibular reconstruction plate through the 2nd dorsal compartment to the 2nd metacarpal (► Fig. 8.2). 16
The bridge plate functions as an internal fixator, reducing the fracture through ligamentotaxis.
Advantages include reducing the need for nursing care of pin site tracts on external fixators, relatively short operative time, and a stable wrist to allow early use of the upper extremity.
Immediate weight bearing through the forearm and elbow is permissible with a platform walker followed by transition to hand grip crutches at 1 month or so.
The plate is removed after fracture consolidation, an average of 112 days in Hanel’s series. 16

5. Open Reduction and Internal Fixation: Volar Plating
In the 1990s, Orbay introduced locked volar plating as an alternative to the more common dorsal plating at the time. 18 This was quickly adopted given the high rate of extensor tendon irritation/ruptures seen with dorsal plating.
Volar plating has demonstrated improved functional results in the early postoperative period with few complications compared to other treatment methods. 19
Indications including unstable distal radius fractures, open fractures, and fractures failing nonoperative management.
The AAOS guidelines recommend operative fixation of fractures with postreduction radial shortening >3 mm, dorsal tilt >10 degrees, or intra-articular displacement/ step-off >2 mm. However, the guidelines do not recommend for or against any specific type of operative treatment. 11
Approach to the distal radius (Video 8.1)
The fracture is most commonly accessed via the modified Henry approach to the distal radius, utilizing the interval between the median nerve/carpal tunnel contents and the radial artery—through the floor of the flexor carpi radialis sheath
This incision may be extended to further open the carpal tunnel should decompression be required.
The radial artery and the superficial branch of the medial nerve are at risk.
Although effort should be made to repair the horizontal limb of the pronator quadratus exposure in order to cover the plate, there were no differences in range of motion (ROM), grip strength, and postoperative complications in a series by Ahsan et al 20 which evaluated repair versus no repair of the pronator quadratus (PQ).
Reduction techniques
In the operating room, the reduction maneuver of Agee can be utilized to recreate radial height, volar tilt, and intra-articular step-off via ligamentotaxis. 21
Reduction maneuver involves traction, volar translation, and pronation.
Should the reduction be unstable, it can be pinned with K-wires aimed proximally through the radial styloid.
Additionally, weighted traction can be applied with finger traps off the edge of the table to provisionally hold the reduction while the plate is applied.
The plate itself can be used as a reduction tool to restore volar tilt as well. The plate is first attached distally such that the proximal portion sits off the radial diaphysis. Then bringing this proximal plate down to bone will tilt the articular surface volarly—“Lift-off” technique.
Outcomes
6. Fragment-Specific Fixation
Fragment-specific fixation has shown to be a viable alternative to other forms of fixation in certain instances. 23
The benefits of this approach include versatile fixation that can be tailored to specific fracture patterns and strong fixation that allows for early postoperative ROM. 23 , 24
Fragment-specific fixation has been shown to provide stronger fixation of volar ulnar corner fragments biomechanically. 25
Drawbacks include an initial learning curve that may increase operative times and hardware irritation. 23 In addition, missed fragments may result in an unstable fixation, highlighting the need for careful preoperative planning.
Principles
There are five primary fracture elements that need to be addressed, namely, radial column, ulnar corner, volar rim, dorsal wall, and impacted articular fracture fragments. 26
Commonly available pin and plate configurations include 26 , 27 volar pin plates, ulnar pin plates, radial pin/column plates, dorsal/volar buttress clip pins, and dorsal/volar radial hook plates.
Plates are placed in an orthogonal position to increase strength. 24 , 26
The focus is on anatomic articular reduction. 24
Metaphyseal defects are filled with bone graft in order to prevent loss of radial length. 24
Small fragments may not need specific fixation if large fragments are fixed around them to hold in place.
Wrist ROM should be started early to prevent postoperative stiffness. 24 , 26
Approaches:
Although the extended flexor carpi radialis (FCR) approach allows access to the entire volar surface of the distal radius, more limited approaches may be used as well depending on the fracture pattern.
Limited-incision volar approach: Utilizes interval between radial artery and brachioradialis to gain access to the volar radial aspect of the distal radius.
Volar ulnar approach: Utilizes the interval between the flexor carpi ulnaris (FCU) and the flexor digitorum profundus (FDP) tendons to gain access to the volar ulnar corner of the distal radius.
Dorsal approach:
A standard 3rd compartment splitting approach may be utilized to view the entire dorsal surface of the radius if needed. Alternatively more limited approaches can be used.
Interval between the 3rd and 4th extensor compartments can be used to access the dorsal wall.
Interval between the 4th and 5th compartments can gain access to the dorsal ulnar corner as needed.
Medoff suggests a stepwise operative approach that involves: 26
Restoring radial column length.
Fixing the volar rim.
Reducing and fixing any dorsal or free articular components to the previously fixed volar rim, using bone graft as needed for defects.
Fixing with a radial column plate to maintain length.
Contraindications 24
Fracture fragment extension into the radial diaphysis is an absolute contraindication.
Relative contraindications include very poor quality bone and large metaphyseal defects.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree