Abstract
Fractional ablative and nonablative resurfacing are effective and safe options for the treatment of rhytides, photoaging, scars, and mild laxity. Microscopic thermal zones induce epidermal and dermal remodeling, thereby creating the resurfaced effect. Preoperative evaluation of skin type, isotretinoin use, infections, prior wound healing, and melasma, among other features, is important as this may affect whether treatment should be pursued. Laser settings at time of treatment are determined by the following: the energy, the depth, the density of mircoscopic thermal zones, and the number of passes. Intraoperative skin cooling is important to prevent bulk heating of the skin. Skin of color mandates modifications in the treatment parameters, particularly treatment density. Postoperative care must be instructed in detail to patients, and patients must be diligent to maximize treatment benefits.
62 Laser Resurfacing
Key Points
Fractional ablative and nonablative lasers are effective and safe options for the treatment of rhytides, photoaging, scars, and mild skin laxity due to dermal remodeling as an effect of treatment.
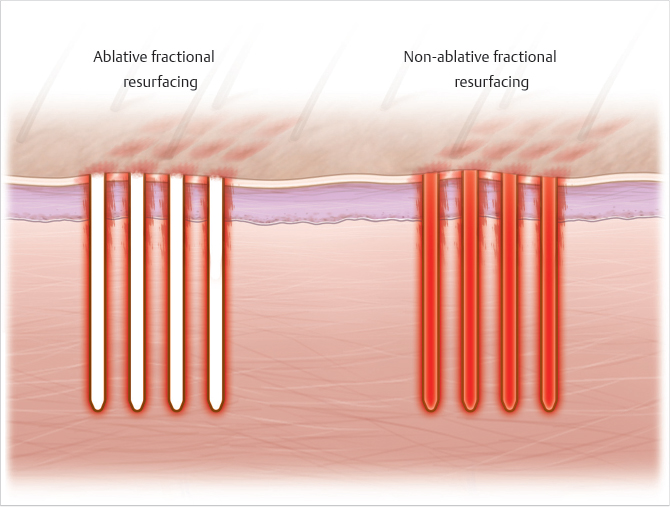
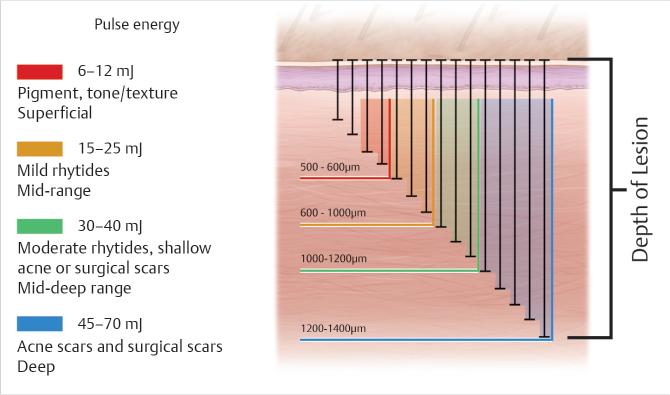
Nonablative wavelengths create dermal coagulative injury at depths of 1 mm or more, sparing the stratum corneum, while ablative wavelengths induce columns of ablation extending from the stratum corneum to the dermis (up to 4 mm). These noncontiguous injury sites are called microscopic thermal zones. Treatment density (coverage) is 5 to 50% with lower density utilized in darker skin types (Fig. 62.1 and Fig. 62.2).
Fractional mode technology affords the ability to treat darker skin types and higher risk anatomic sites albeit with caution.
62.1 Indications
Indications for fractional laser therapy are listed in Table 62.1 .
62.2 Device Selection
The instructions in this chapter are based on experience with the Solta Fraxel DUAL (1,550 nm/1,927 nm, Erbium/Thulium) and Solta Fraxel Re:pair (10,600 nm, CO2). These devices utilize intelligent optical tracking system that distributes the microscopic thermal zones evenly over several passes of the roller accounting for the practitioner’s gliding speed, thus reducing risks of bulk heating. The concepts presented in this chapter may be extended cautiously to other infrared nonablative fractional lasers (1,550 nm/1,540 nm/1,440 nm) and ablative fractional lasers (2,790 nm/2,940 nm).
62.3 Preoperative Steps
The facial resurfacing procedure begins with a thorough preoperative analysis to assess the severity of dermatoheliosis, distribution of rhytides, dyschromia, scarring, and overall goals of treatment and patient expectations.
Patients with concerns about epidermal photoaging, mild rhytides, and scars (atrophic, burn, or traumatic) are good candidates for nonablative fractional resurfacing (NAFR). Younger scars respond better to laser therapy. Patients with deeper rhytides, greater laxity, traumatic scars, burn scars with contractures, and deeper acne scarring are good candidates for ablative fractional resurfacing (AFR). Patients should expect 2 weeks of downtime after AFR.
Assessment of absolute contraindications, including active infections, pregnancy, and koebnerizing phenomena such as psoriasis and vitiligo.
Assessment of relative contraindications, including recent tanning or sun exposure, and use of isotretinoin within the last 6 months.
History of subtle melasma and postinflammatory hyperpigmentation should be assessed as rebound hyperpigmentation may occur after aggressive treatments (high fluence, high coverage). In this case, patients should be counseled on use of fractional nonablative lasers at low fluences and/or low coverage which may necessitate more treatments.
To avoid pigmentary complications, recommend pretreatment with hydroquinone, retinoic acid, or topical tranexamic acid (such as SkinMedica © Lytera 2.0 or SkinCeuticals © Discoloration Defense) for 2 to 4 weeks prior and photoprotection.
History of herpes simplex virus (HSV) should be assessed and antiviral prophylaxis should be initiated 1 day prior to treatment and continued for a total of 3 days (nonablative) and 7 days (ablative).
In our experience, oral antibiotics (Doxycycline 100 mg twice daily started the day before treatment, total 7 days duration) are provided for all patients undergoing AFR.
In contrast, patients with history of acne undergoing NAFR can be treated with low dose antibiotics (doxycycline 50 mg twice daily started on day of procedure, total 5 days duration) to reduce the risk of acne flare after the procedure.
Recommend use of Alastin© Regenerating Skin Nectar as pretreatment 2 to 3 weeks prior to procedure to activate dermal remodeling cellular pathways, which will be employed during the postoperative period.
Topical retinoids should be discontinued 5 days prior to laser treatment.
Topical anesthesia for 60 minutes prior to procedure is recommended for NAFR (23% lidocaine/7% tetracaine for skin types 1–3 and thicker skin; 20% benzocaine/6% lidocaine/6% tetracaine for skin types 4–6, Asian patients, and acne prone skin; EMLA [lidocaine/prilocaine] may also be considered for Asian and sensitive skin types), whereas conscious sedation is recommended for AFR to permit patient comfort.
Cleanse treatment sites with chlorhexidine liquid to ensure complete removal of topical anesthesia prior to treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








