6 Gynecomastia
INDICATIONS
Progressive gynecomastia that lasts more than 12 months and is not responsive to medical management
Adolescence-associated gynecomastia that occurs during development of social skills and interactions and continues beyond mid-adolescence (past 12 years of age)
Weight-loss-associated gynecomastia that persists despite massive weight loss
Psychologically symptomatic gynecomastia that has associated psychological and emotional trauma
INTRODUCTION
Gynecomastia is defined as benign enlargement of the breast in the male. Although this can be physiologic and often spontaneously regresses, it can become progressive and become a factor of psychological trauma to the male patient. Although the range of gynecomastia appearance is continuous and involves both the parenchyma and the skin envelope, discrete grades that allow for operative planning have been developed. 1 , 2 The Simon classification takes into consideration the degree of enlargement and the degree of skin excess (Table 6.1).
Grade | Enlargement | Skin excess |
I | Small | Absent |
IIA | Moderate | Absent |
IIB | Moderate | Present |
III | Large | Present |
Rohrich’s more recent 2003 classification quantifies the amount of breast tissue and incorporates ptosis, rather than skin excess, in the grading of gynecomastia. The standard Regnault’s classification of ptosis 3 describes four types of ptosis: first degree or grade I, in which the nipple-areolar complex (NAC) is within 1 cm of the inframammary fold; second degree or grade II, in which the NAC is below the inframammary fold but not at the lowest contour of the breast; third degree or grade III, in which the NAC is at the lowest contour of the breast; and fourth degree, or pseudoptosis, in which the majority of the gland is below the level of the inframammary fold.
We use Rohrich’s classification in surgical planning (Table 6.2). The surgical goals are thus to reduce the amount of breast tissue as well as improve the breast ptosis while utilizing surgical incisions that will leave inconspicuous scars. This chapter describes ultrasound-assisted liposuction (UAL), suction-assisted lipectomy (SAL), and traditional resection and their respective roles in the surgical treatment of gynecomastia.
ULTRASOUND-ASSISTED LIPOSUCTION
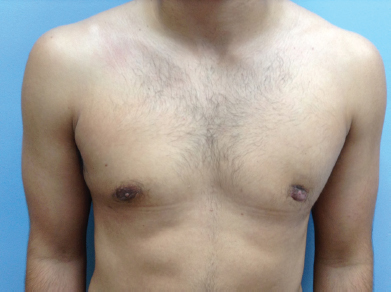
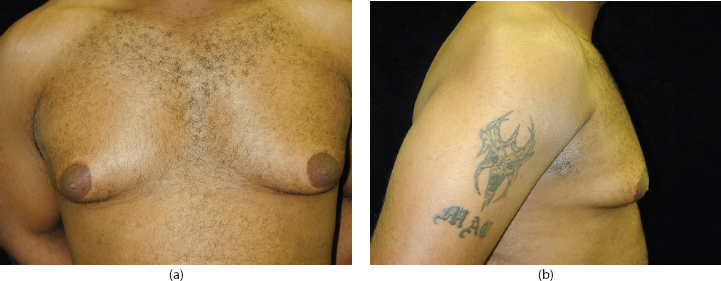
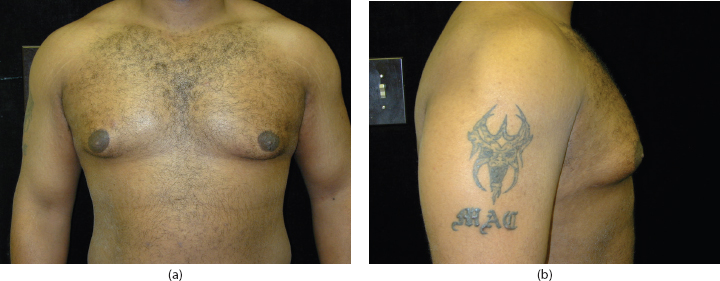
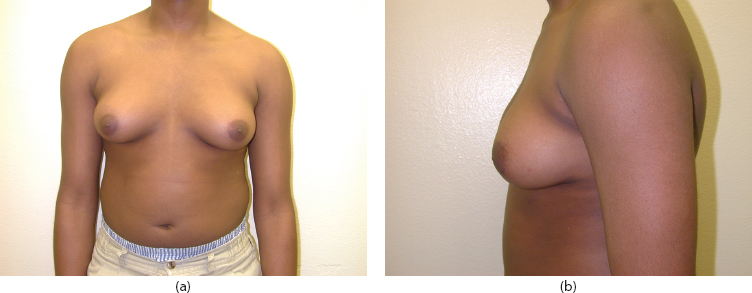
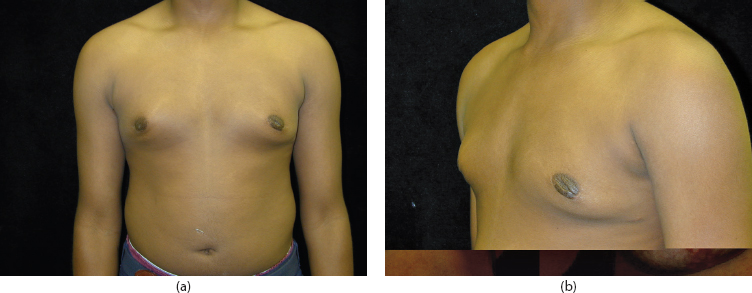
The UAL technique is especially useful for the more fibrous tissue that is usually seen with gynecomastia. It is effective for all grades of gynecomastia; however, if removal of redundant skin is required, a staged excision is delayed for 6 to 9 months to allow for maximal skin retraction and healing to occur. Figures 6.1 to 6.4 illustrate preoperative and postoperative pictures of patients for whom UAL was utilized in grade I and II gynecomastia. Figures 6.5 and 6.6 illustrate the great flexibility and use of UAL along with SAL.

Special equipment
Necessary equipment for UAL includes a scalpel; an infiltration pump and infiltration cannula of choice (we prefer a Mercedes tip cannula for infiltration and a solution of 1 L lactated Ringer solution mixed with 1 ampoule of 1:1000 epinephrine); UAL generator of choice; a standard surgical aspirator; and a closed-suction drain.
Preoperative markings
We perform our preoperative marking (Figure 6.7) with the patient in the standing position, which prevents distortion of the tissues and displacement of the ptotic breast and skin envelope. Our markings allow visualization of critical landmarks during the case and planning for surgical incisions.

Our sequence of marking is as follows:
We first mark bilateral inframammary folds.
Then, the sternal midline is marked.
The chest boundary and planned stab incision sites are next. We design 5-mm incisions in the lateral aspect of the inframammary fold, which provides optimal access to dense breast parenchyma and allows access to obliterate the inframammary fold and to suction the medial chest. 2
The pigmented areolar skin junction with the non-pigmented chest wall skin, from the 3-o’clock to the 9-o’clock positions, is marked. (This periareolar scar, used for skin incision, camouflages the subsequent scar well.)
Contours and protuberant areas are marked, particularly in the axilla, superiorly along the upper chest, and inferiorly below the inframammary fold.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree