5 Breast reduction: Inferior pedicle, wise pattern
INDICATIONS
Symptomatic macromastia, including neck pain, shoulder pain, back pain, bra strap grooving, intertrigo or skin breakdown from bra use
INTRODUCTION
Macromastia is a pathologic condition consisting of hypertrophy of the breast (see Figure 5.1). It generates both physical and psychological distress, presenting a significant threat to a woman’s health-related quality of life. In addition to psychological considerations regarding poor perception of body image and sense of self-esteem, macromastia has been consistently correlated with a number of musculoskeletal complications, including neck pain, back pain, headache, peripheral neuralgias, and shoulder pain, among others. According to data released in 2008 by the American Society for Aesthetic Plastic Surgery (ASAPS), reduction mammaplasty has been among the most rapidly growing plastic surgical procedures in the United States. More than 153,087 reductions were performed in 2007, which was increased from the 1997 value of 47,874 reductions. 1 – 4

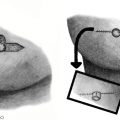
Traditionally, reduction mammaplasty has manifested a well-established surgical approach to the relief of physical pain and discomfort associated with breast hypertrophy. While several techniques with unique advantages and disadvantages have been proposed in the approach to breast reduction, debate over which technique produces optimal patient outcomes continues to persist. In 1998, Hidalgo et al. 5 , 6 conducted a survey at the meeting of the American Society of Plastic and Reconstructive Surgeons. This revealed the traditional inferior pedicle, inverted T-scar method was the most popular reduction technique among plastic surgeons (Figure 5.2). This conclusion was more recently confirmed in 2008 when a national survey of 2665 members of the ASPS revealed that 69% of surgeons preferred the inferior pedicle technique over other popular methods for breast reduction. 7 – 9

The inverted T-scar skin design, which includes a variety of glandular pedicle types, is an attractive alternative among reduction mammaplasty protocols due to its predictability, versatility, and level of control that it offers over both the extent of reduction and the breast-shaping process. Despite these advantages, common criticisms of the inverted T-scar approach include breast shape abnormalities (pseudoptosis), areolar malposition, hypertrophic scarring, and poor long-term projection. However, several outcome studies have demonstrated high patient satisfaction and well-being following reduction mammaplasty, particularly with the inferior pedicle technique (86–97%). This tutorial presents a method of breast reduction that is reliably reproducible and consistent. Table 5.1 indicates the special equipment needed for this method.
Tape measure Radiographic or wire template Normal saline, 1-L bag with 25 mL 1% lidocaine with epinephrine 1:100,000 (tumescent) Methylene blue and tuberculin syringe (1 mL) IV Ancef, 1 g prior to incision, or Clindamycin, 900 mg if penicillin allergic Blake drains 19F, 1 per side 2-0 Prolene, 2-0 Vicryl, 2-0 nylon, 3-0 Monocryl, 4-0 Monocryl sutures |
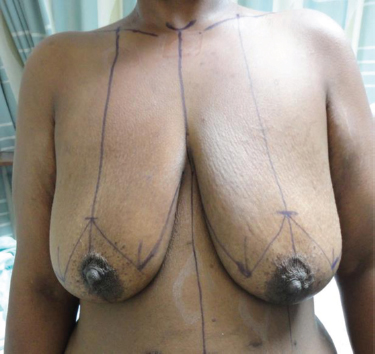
PREOPERATIVE MARKINGS
With the patient standing, perform the marking in a preoperative hold with a chaperone present.
Mark midline from the sternal notch to the umbilicus (Figure 5.3).
Mark the bilateral inframammary folds (IMFs).
Mark the breast meridians by wrapping a tape measure around the posterior neck and placing it in line with each nipple. Alternatively, you can mark 7 cm lateral to the sternal notch along the clavicular line and then reference down to the nipple.
Transpose the IMFs by placing a finger under the breast and then palpating anteriorly to feel the point to mark along the breast meridian. This marks the new nipple position (at the level of the IMFs).
Measure 2 cm superior from this position to place the most superior aspect of the nipple position on the template.
Draw marks over the template.
Continue the marks laterally. Warn the patient that all axillary and lateral chest excess will not be removed with the index procedure, and that this area will become more noticeable after breast reduction.
Mark and discuss any asymmetries with the patient. Warn the patient of the inability to completely correct these asymmetries.
Double-check the marks, including measuring from the midline to relevant points using a tape measure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree