Abstract
This chapter shows that successful reconstructive surgery is heavily dependent on a thorough understanding of the components of truncal anatomy. The implications of thorough knowledge for chest wall and breast reconstruction are obvious. Additionally, tissues from the trunk can be used elsewhere as free flaps. The authors describe the anatomy of the trunk, abdomen, pelvis, and posterior trunk. Each section begins with the skeletal foundation and from there progresses into the fascia and muscles and concludes with a discussion of the pertinent vasculature.
4 Anatomy of the Trunk
4.1 Goals and Objectives
Understand the proper vascular, neural, muscular and bony anatomy of the trunk in relation to plastic surgery.
Appreciate that flap surgery is essentially applied anatomy.
Know the anatomy well to maximize flap success and patient safety.
4.2 Introduction
Reconstructive plastic surgery is often dependent on a thorough understanding of the components of truncal anatomy. Implications for chest wall and breast reconstruction are obvious. Additionally, tissues from the trunk can be used elsewhere as free flaps. The authors describe the anatomy of the trunk, abdomen, pelvis, and posterior trunk. Each section begins with the skeletal foundation and progresses into the fascia, muscles, and concludes with a discussion of the pertinent vasculature.
4.3 Chest
The superior border of the chest is made up by both clavicles and the manubrium. The anterior axillary line, defined as a line between the middle and lateral end of the clavicle, defines the lateral border. The costal margin, defined by the edge of ribs 7 through 10, and the distal portion of the sternum define the inferior border.
The hallmark of the superficial anatomy of the chest is the breast tissue. It can extend from the second rib to the sixth rib and from the sternum to the latissimus dorsi. The entire chest wall has a superficial fascia that lies just deep to the skin and subcutaneous tissue. Immediately over the breast tissue, this fascia is divided into superficial and deep, surrounding the breast tissue. In between these two layers, Cooper’s ligaments run perpendicular, providing support to the parenchyma. Just lateral to the midclavicular line, the nipple-areolar complex can be found at the level of the fourth intercostal space. 1
The breast has a very rich blood supply that is derived from the internal thoracic perforators, thoracoacromial artery, lateral thoracic artery, and intercostal vessels. 2 The innervation is mainly by the thoracic intercostal nerves branches from T2 to T6. Although the exact nipple location can vary, the innervation and blood supply remains constant at the level of the fourth intercostal space, being provided mainly by T4 lateral cutaneous branch and the internal thoracic artery perforators. 3
Inspection and examination of the chest reveals a groove on the superior and lateral portion of it, which marks the clavipectoral triangle. It is bordered by the pectoralis major and deltoid muscles as well as the clavicle. It contains the cephalic vein and the clavipectoral fascia, which courses below the pectoralis major. Deep to this triangle, the subclavian vein and subclavian artery can be found. 2
4.3.1 Skeletal Structure
The skeletal structure of the thorax is formed by the sternum, the ribs, and the vertebral column. Additionally, the clavicles connect the chest with both upper extremities.
The sternum is a convex, flat bone that can be found in the center of the chest. It is divided into the manubrium, body, and xiphoid process; the sternal angle marks the point where the body joins the manubrium. On its lateral surface, it articulates with costal cartilage from the first seven ribs. The clavicles also articulate at the level of the manubrium. The manubrium serves as the insertion of the sternocleidomastoid muscles. The body serves as the origin of the sternocostal head of the pectoralis major. 2
There are seven pairs of true ribs and five pairs of false ribs. True ribs connect directly to the sternum while false ribs do so indirectly with costal cartilage from ribs above them. The superior border is the insertion point for the intercostal muscles, while the inferior border has the intercostal neurovascular bundle. The inner surface of the ribs is lined with pleura. The head of the ribs articulate, with two facets, with the vertebral column.
The clavicle is a double curved bone that articulates medially to the manubrium and laterally to the acromion forming the sternoclavicular and acromioclavicular joints. The first two-thirds of the ribs have a concave anterior border, while the posterior border is convex. The deltoid, trapezius, subclavius, pectoralis major, sternocleidomastoid, and sternohyoid muscles attach to the clavicle. 4
The vertebral column will be discussed later in this chapter.
4.3.2 Muscles
The chest has four muscle groups that carry several mobility and breathing functions. They are the pectoralis major, pectoralis minor, serratus anterior, intercostal, and subclavius muscles.
The pectoralis major is the most superficial muscle of the chest. It has a fan-shaped appearance with fibers running from its medial and superior origin to the lateral edge of the bicipital groove of the humerus. The clavicular head originates from the anterior border of the medial portion of the clavicle superiorly and the sternocostal head from the medial and anterior aspect of the sternum as well as from the costal cartilage of ribs 2 through 6. It assists in the flexion and extension of the humerus as well as in its adduction and medial rotation. The main blood supply is derived from the pectoral branch of the thoracoacromial trunk. 5 , 6 , 7 , 8 , 9 On the medial aspect of the muscle, there are additional perforator vessels which are derived from the internal mammary system. On the lateral portion, perforators from the intercostal arteries and lateral thoracic artery also supply the muscle. 3 The dominant pedicle, or main blood supply combined with the secondary segmental blood supply, classifies this muscle as a Type V Mathes and Nahai flap. 5 In plastic surgery, this muscle is commonly used to cover local sternal wounds. Innervation is accomplished by the lateral and medial pectoral nerves that contract the clavicular and the sternocostal head, respectively. 6
The pectoralis minor is a flat and triangular muscle, deep to the pectoralis major. The muscle has three heads that originate from the external border of ribs 3, 4, and 5; the fibers then converge into the internal border of the coracoid process of the scapula. Its main function is to stabilize the scapula against the chest wall. Blood supply is most commonly from the pectoral branch of the thoracoacromial trunk and the lateral thoracic artery. These two dominant pedicles classify this muscle as a type III flap. 5 It is often used to locally cover defects of the shoulder and axilla but, it can also be used for breast implant coverage as well as a functional muscle free flap when combined with microsurgical anastomoses in facial reanimation. 5 It is innervated by the medial pectoral nerve and also receives some innervation from the lateral pectoral nerve that passes directly through it. 10
The serratus anterior is a flat and thin muscle that lies in the lateral wall of the chest. It originates from the first nine ribs and it inserts on the medial border of the scapula. This muscle holds the scapula against the chest wall and assists in the upward rotation and protraction of the scapula. The superior portion of the muscle derives its blood supply from the lateral thoracic artery, while the lower portion from the thoracodorsal artery. 11 This muscle has two dominant pedicles making it a type III muscle flap. This muscle can be used in plastic surgery to assist in breast reconstruction with coverage of an expander and it also finds use as a functional free flap in facial reanimation. 5 It is innervated by the long thoracic nerve. 12
The ribs are connected by a series of muscles that play a role in the expansion and active relaxation of the chest cavity during respirations. They accomplish this function in part by the opposing directions of their muscle fibers. The deepest muscle is the innermost intercostal followed by the internal intercostal. The external intercostal muscle is the most superficial. Their blood supply and innervation are derived from the neurovascular bundle that runs on the inferior aspect of each rib.
The subclavius muscle is a small fusiform muscle that is located immediately below the clavicle and above the subclavian artery. It originates just distal to the costal cartilage of the first rib and inserts in the inferior surface of the middle third of the clavicle. 4 Protecting the brachial plexus and subclavian vessels is part of the function of this muscle. 13 It also assists in shoulder depression. Blood supply derives from the thoracoacromial trunk.
4.3.3 The Angiosome
Prior to the increased interest in microsurgical free flaps, little importance was assigned to the superficial blood supply of overlying skin. The organization of superficial vasculature territories of the skin and soft tissues has been described by the angiosome model. Perforating vessels give rise to defined islands of blood supply which vary in density according to anatomic location. A total of 376 such vessels of 0.5 mm or greater diameter have been identified in the literature. 14 Just as in the dermatome model, where sensory nerve fiber overlap occurs, the angiosomes have similar watershed areas of overlap. For instance, the head, thorax, and proximal limbs have a larger but less dense angiosome pattern as compared to the distal extremities. 14 This network of vessels within the skin assists our clinical guidance in the design of local soft-tissue flaps for wound coverage, such as in the field of plastic surgery.
4.3.4 Vasculature
The chest has several networks of blood vessels that supply the skin and soft tissues (Fig. 4‑1). There are a series of vessels that connect the subclavian and external iliac arteries and supply the anterior chest wall and the anterior abdominal wall throughout their course. We will discuss the blood supply to the anterior chest structures in this section.
There are two major vessels: the subclavian and axillary arteries that are responsible for perfusion of not only the upper extremities but also of the chest wall.
The subclavian artery originates from the brachiocephalic trunk on the right and the aortic arch on the left. It travels laterally between the anterior and middle scalene muscles and becomes the axillary artery after it crosses the lateral border of the first rib. It gives rise to the internal thoracic artery, dorsal scapular artery, and vessels that supply the neck.
The axillary artery originates on the lateral border of the first rib and becomes the brachial artery after passing the teres major. The pectoralis minor helps in further dividing this vessel into three different parts. The first part is medial to the muscle and gives rise to the superior thoracic artery. The second portion of the vessel is immediately inferior to the muscle and the thoracoacromial and lateral thoracic arteries are derived from it. Finally, the third part is lateral to the pectoralis minor and gives rise to the subscapular artery, anterior humeral circumflex artery, and posterior humeral circumflex artery. 15
The branch of the subclavian artery that plays a key role in supplying blood to the anterior chest wall is the internal thoracic artery. It travels within the thoracic cavity from its origin toward its bifurcation into the superior epigastric and musculophrenic arteries. It can be found lateral to the sternum, running deep to the internal intercostal muscles but superficial to the innermost muscles. During its course, it gives perforating vessels through the second and sixth intercostal spaces, supplying the pectoralis major and medial chest wall as well as medial breast parenchyma. 16 The internal mammary vessels, also termed “the internal thoracic vessels,” can additionally be used as recipient anastomotic sites for microsurgical free flaps in breast reconstruction.
The superior thoracic artery arises from the first part of the axillary artery as its only branch and travels along the pectoralis minor border. It supplies the superior portion of the serratus anterior as well as the first and second intercostal spaces.
The thoracoacromial artery is a very short trunk that is deep to the pectoralis minor. It gives rise to four branches: pectoral, acromial, clavicular, and deltoid. The pectoral branch travels in between the pectoralis major and minor with small branches supplying blood to them. Small perforators also supply the skin on the superior and lateral aspect of the chest. The acromial branch goes over the coracoid process and under the deltoid muscles supplying these muscles. The clavicular branch provides blood supply to the subclavius muscle and the deltoid to the pectoralis major and deltoid muscles. 12 , 13
The lateral thoracic artery usually travels at the lower border of the pectoralis minor. It supplies the superior portion of the serratus anterior. It has lateral perforators that supply the breast parenchyma as well as the superior and lateral portion of the skin and subcutaneous tissue of the thorax. 17
The largest branch of the axillary artery is the subscapular artery. It supplies the latissimus dorsi and also provides branches to the inferior portion of the serratus anterior. It begins its course at the lower border of the subscapularis muscle and gives off two branches: the thoracodorsal and circumflex scapular arteries. 16 The branch that supplies the serratus is usually found superficial to the muscle accompanying the long thoracic nerve.
The anterior and posterior circumflex humeral arteries are also branches of the third part of the axillary artery. The anterior circumflex artery runs in front of the neck of the humerus and deep to the coracobrachialis and biceps brachii muscles. It provides blood to the biceps brachii and the deltoid muscle. The posterior humeral circumflex runs posterior to the axillary nerve through the quadrangular space. It also supplies the deltoid muscle as well as provides branches to the teres minor. 18
Finally, the anterior and posterior intercostal arteries also play a role in the perfusion of the chest wall. The anterior portion arises from the internal thoracic artery, while the posterior portion arises from the thoracic aorta or the costocervical trunk (a branch of the subclavian artery). 19 , 20
4.4 Abdomen
The abdominal activity and the abdominal wall make up most of the anterior trunk. It provides flexibility and facilitates mobility. It also provides protection for the abdominal organs.
4.4.1 Fascia
Immediately below the skin, we find Camper’s fascia, followed by Scarpa’s fascia. Camper’s fascia is more prominent below the umbilicus. As it progresses inferiorly, it becomes continuous with the superficial thigh fascia of the thigh. Scarpa’s fascia is connected to the external oblique muscle that is immediately posterior to it. It forms the fundiform ligament, which is found at the dorsum of the penis. 15 At the inferolateral portion of the abdominal wall, it is continuous with the fascia lata of the thigh, just below the inguinal ligament. In males, toward midline, Scarpa’s continues over the penis and scrotum, forming dartos fascia. In females, it continues into the labia majora and forms the fascia of Colles. 4
4.4.2 Skeletal Structure
The middle and inferior portion of the trunk lacks the anterior bony structure that is seen in the chest cavity. The anterior abdominal wall lacks bony structures, giving the trunk mobility and flexibility. The posterior skeletal frame and the most inferior aspect of the trunk (vertebral column and the bony pelvis) will be described later in this chapter.
Although not part of the anterolateral portion of the abdomen, the costal margin of the chest is the superior boundary of the abdomen. Inferiorly the pubic tubercle defines the inferior portion of the abdomen.
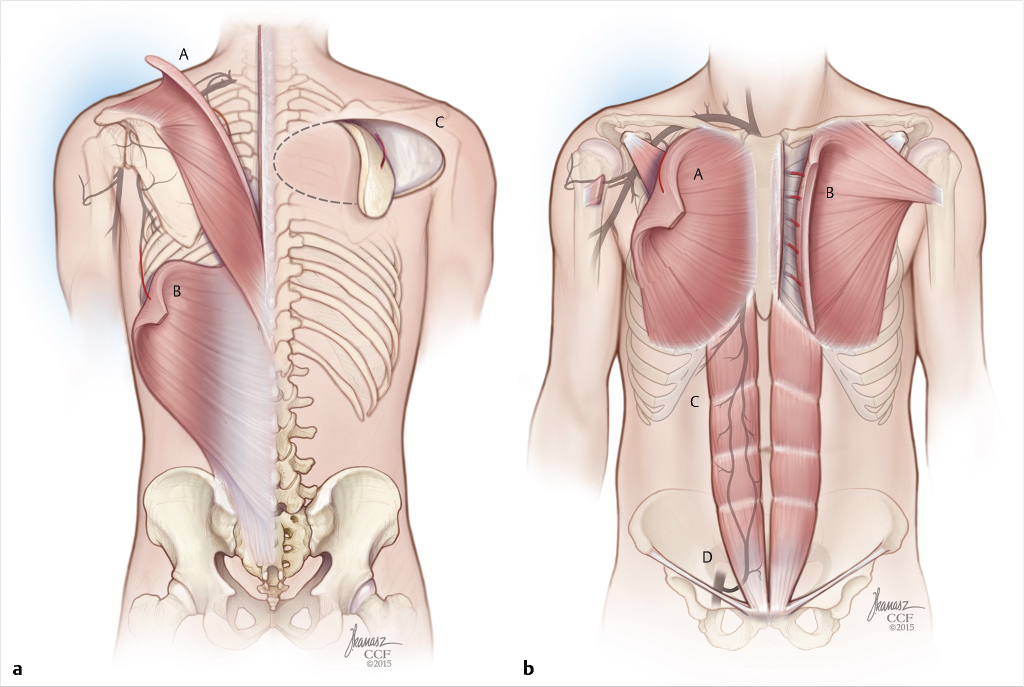
4.4.3 Muscles
The anterolateral abdominal wall is an extensive association of muscles that extends from the costal margin to the inferior portion of the trunk. The rectus abdominis, external oblique, internal oblique, transverse abdominal muscles, and their respective aponeurosis form this structure. Several anatomical structures are formed at the boundaries of these muscle groups.
The structure that is found in the midline of the abdomen is known as linea alba. This predominantly fibrous white line is formed by the convergence of the aponeurosis of the abdominal muscles. It runs from the xiphoid process to the pubic symphysis. It separates the right and left rectus abdominis muscles. In this line, the umbilicus is situated, which is a scar that arises after the obliteration of the umbilical cord.
The rectus muscles are encased by the aponeurosis of other abdominal muscles that is known as rectus sheath. At approximately one-third of the distance between the umbilicus and the pubic symphysis, we can identify a horizontal line known as the arcuate line. Between the costal margin and this line, the internal oblique aponeurosis divides into an anterior section that passes over the rectus muscle and a posterior section that passes under the rectus. The anterior internal oblique aponeurosis is joined by the external oblique tendinous portion to form the anterior rectus sheath. The posterior rectus sheath is formed by the posterior aspect of the internal oblique aponeurosis and the transversalis aponeurosis. Below the arcuate line, the aponeurosis of the external, internal, and transverse abdominal muscles travel anterior to the rectus muscle. The lack of posterior sheath at this level is what creates the arcuate line.
Just lateral to the rectus muscles, we can find the linea semilunaris. This fibrous line can be found extending from the cartilaginous portion of the ninth rib to the pubic tubercle. It is formed by the internal oblique aponeurosis, as it divides to enclose the rectus muscle.
The rectus abdominis is a long flat muscle that is found on both sides of the abdominal wall. It originates at the pubic crest and inserts to the costal cartilages of ribs 5 through 7 and xiphoid process of the sternum. It is crossed by three bands of fibrous tissues called tendinous intersections. This muscle assists in the flexion of the lumbar spine and forceful exhalation. Its blood supply derives from the superior and inferior epigastric arteries. Due to the presence of these two dominant pedicles, the muscle is considered a type III flap by the classification of Mathes and Nahai. It has been extensively utilized as a flap in breast reconstruction as well as for perineal defects. 5 Innervation is accomplished by the last six thoracoabdominal nerves (T7–T12), which travel through the anterior rectus shealth. 21
The pyramidalis muscle is also contained in the rectus sheath, anterior to the rectus abdominis. This small triangular muscle originates at the pubic symphysis and pubic crest and inserts at the linea alba. 4 It serves to tense the linea alba. It is supplied by the same arterial vasculature supplying the rectus muscles.
The external oblique muscle is one of three flat muscles that forms the anterolateral abdominal wall. It originates from the fifth through the twelfth ribs and inserts in the iliac crest, pubic tubercle, and the linea alba. It is the largest and most superficial of the three lateral abdominal wall muscles. The medial aspect of the muscle has a tendinous aponeurosis that in the midline makes part of the anterior rectus sheath. The inferior portion of the aponeurosis inserts into the anterior superior iliac spine and the pubic tubercle, forming a defined edge known as inguinal ligament. The external oblique muscle has a segmental blood supply via the lateral cutaneous branches of the inferior eight posterior intercostal arteries. This segmental vascularization classifies this muscle as a type IV flap. This muscle finds uses in coverage of the chest, posterior trunk, and abdomen, as well as in breast reconstruction. 5
Just deep to the external oblique, we can find the internal oblique muscle. The muscle originates from the iliac crest, thoracolumbar fascia, and the inguinal ligament. It inserts in the 10th, 11th, and 12th ribs, as well as at the linea alba medially. Its aponeurosis is part of the rectus sheath. The inferior aspect of the muscle, corresponding to the muscle fibers that originate from the inguinal ligament, forms an arch over the internal portion of the inguinal ligament and joins the aponeurosis of the transverse abdominal muscle forming the conjoint tendon. This muscle’s circulation is derived from a dominant pedicle, a minor pedicle, and a secondary segmental blood supply which classify it as a type V flap. The dominant pedicle is the ascending branch of the deep circumflex iliac artery. The minor pedicles are the lateral branches of the deep inferior epigastric artery and the secondary segmental supplies are derived from the lower thoracic and lumbar arteries. It is used in the coverage of groin, perineal, and greater trochanter wounds. It has also been used as a free flap to the head and neck, upper extremity, and lower extremity. 5
The deepest of the abdominal wall muscles is the transverse abdominal muscle. It originates from the iliac crest, thoracolumbar fascia, inguinal ligament, and costal cartilage of the 7th through 12th ribs. The muscle inserts into the xiphoid process, linea alba, and pubic crest. Similar to the other two muscles, the aponeurosis forms the rectus sheath as well as the conjoint tendon.
The external oblique, internal oblique, and transverse abdominal muscles assist in the flexion and rotation of the vertebral column. They also help increase intra-abdominal pressure by pulling the chest cavity downward. These muscles derived their blood supply from the lower thoracic intercostal vessels. They are innervated by the thoracoabdominal nerve routes extending from T7 to T12 and L1. 4
4.4.4 Vasculature
The abdominal wall has an extensive network of vessels that supply the different muscles and soft tissues. There are several anastomoses throughout that ensure adequate collateral flow and can be very helpful for the harvesting of grafts.
As a continuation of the thoracic intercostal vessels, the lumbar arteries supply a portion of the anterolateral abdominal wall. They derive from the posterior portion of the abdominal aorta. They travel horizontally toward midline, crossing behind the sympathetic chain and on the right, posterior to the vena cava. They perforate the transverse abdominal muscle and travel in between this muscle and the internal oblique.
The superior epigastric artery supplies the superior portion of the abdominal wall. It arises from the internal thoracic artery at the levels of the sixth and seventh costal cartilage and anastomoses with the inferior epigastric vessel at the umbilicus. Superiorly, it travels anterior to the transverse abdominal muscle and perforates the rectus muscle. 22
The inferior epigastric artery supplies the lower portion of the abdominal wall. It is a branch of the external iliac artery and arises just above the inguinal ligament. It pierces the transversalis fascia passing anterior to the arcuate line dividing into a medial and lateral branch. Several perforates arise from these branches supplying the subcutaneous tissue skin overlying the abdominal wall. 22 It continues to ascend in between the rectus muscle and the posterior rectus sheath until it anastomoses with the superior epigastric artery.
Another branch of the external iliac artery, the deep circumflex iliac artery, arises opposite to the inferior epigastric artery. It travels along the iliacus, posterior to the inguinal ligament, toward the anterior superior iliac spine where it gives an ascending branch. It anastomoses with the lateral femoral circumflex artery at this level. The artery then pierces the transversalis fascia and travels along the inner lip of the iliac crest where it gives rise to periosteal branches. It then perforates the transverse abdominal muscle and travels between this muscle and the internal oblique muscle to anastomose into the iliolumbar and lumbar vessels. 22
The superficial epigastric artery can be found arising from the femoral vessel, below the inguinal ligament. It travels through the femoral sheath and distally it continues anterior to the inguinal ligament. 23 The artery then travels in the subcutaneous tissue in the lower abdomen supplying the overlying skin and adipose tissue. The femoral artery also gives rise to the superficial circumflex iliac artery, which travels over the inguinal ligament in the superficial fascia along iliac crest. It supplies the skin and subcutaneous tissue in the inferior portion of the abdominal wall. 24
4.5 Pelvis
The most inferior aspect of the trunk is known as the pelvis. As opposed to the superior portion of the trunk, where the differences are mostly related to appearance and the presence of breasts, the pelvis has obvious differences between both men and women. The overall architecture of the pelvis is similar, consisting of a bowl-shaped bony structure with muscles and connection to the lower extremities. However, the perineal anatomy and underlying organs differ between sexes. In the next section, the anatomy of the pelvis will be reviewed.
4.5.1 Skeletal Structure
The pelvis is formed by the iliac bones bilaterally. It is formed by three separate elements known as ilium, ischium, and pubis. In adults, these three are fused into one bone as opposed to infants.
The ilium is divided into two parts: the ala and the body. The arcuate line and the margin of the acetabulum separate the two parts of this bone. The ala is the lateral boundary of the pelvis. Its anterior and posterior borders have two projections: anteriorly they are known as the anterior superior iliac spine and the anterior inferior iliac spine, and posteriorly the posterior superior iliac spine and posterior inferior iliac spine. 4 The external portion of the body of the iliac bone participates in the formation of the acetabulum and it has an articular segment as well as a nonarticular one that forms the acetabular fossa.
The ischium forms the inferior and posterior aspect of the hip bone. It also participates in the formation of the acetabulum. Anterior to the ilium and ischium, we can find the pubic bone. The ischium has an ischial body, an ischial spine, a tuberosity and a ramus. The inferior ramus of the pubic bone units with the iscial ramus to form the obturator foreman. 21
The sacrum and coccygeal anatomy were described in the back section. These bones articulate with the iliac bones posteriorly to form the sacroiliac joint. As opposed to most of other body joints, its main function is to stabilize the union between the trunk and the lower extremities and not movement. In women, this joint may actually facilitate movement during delivery.
An anterior joint is also formed by the symphysis pubis. It is formed by the pubic area of both iliac bones. Similar to the sacroiliac joint, the symphysis pubis is not mobile and only participates in the stabilization of the pelvis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree