Chapter 17 2ST/2Gr, 4ST, and 3ST/2Gr Techniques
Deciding Which Hamstring Configuration to Use
Introduction
Use of the four-strand hamstring (4HS) graft using the semitendinosus (ST) with or without the gracilis (Gr) has increased dramatically in the past 5 years. This graft has long been considered to have lower morbidity than bone–patellar tendon–bone (BPTB) grafts. After reports showed its clinical stability results to meet or exceed those of the BPTB,1–7 its use began to significantly increase. 2ST/2Gr is the most commonly used hamstring graft, followed by 4ST. However, a total of six different multistrand hamstring graft configurations have been reported and are in current use. This chapter will describe the advantages of each configuration according to the five parameters involved in decision making. Graft preparation techniques will also be described.
The Parameters for Choosing A Hamstring Graft Configuration
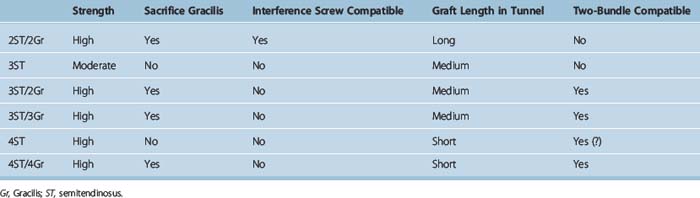
Five parameters (Table 17-1 and see later discussion) will drive decision making regarding which HS graft, or soft tissue graft in general, will be used. The first three parameters are available graft length in the tunnel, the type of fixation that can be used, and whether the gracilis must be sacrificed. These are generally themost important considerations to most orthopaedic surgeons. The last two parameters, relative graft strengths and whether it is double-bundle compatible, are important to some.
1 Is the Graft Long Enough to Allow Adequate Tunnel Healing?
In our experience, ST harvests range in length from 24 to 34 cm, with most being between 26 and 30 cm in usable length. Intraarticular anterior cruciate ligament (ACL) length is 3 to 3.5 cm.8 Roughly 1 cm of shortening occurs as a result of whipstitch implantation. Thus, for example, a 27-cm graft will be 26 cm after suturing. When quadrupled, this length is 6.5 cm. Subtracting 3 cm for the intraarticular portion leaves 3.5 cm of graft for both tunnels, or about 1.75 cm or 17.5 mm for each tunnel. If the ST is only doubled and not quadrupled, the resultant 12 cm or longer graft can provide 4 cm or more of graft length in each tunnel. Some surgeons9 will use 4ST if the ST is 30 cm or longer and 2ST/2Gr if the ST harvest is less than 30 cm.
The Argument for Greater Length Being Necessary
Many surgeons are not comfortable with graft lengths of less than 2 cm in each tunnel. The principal argument in favor of this is the study by Greis et al10 that shows greater pull-out strength as graft length increases.
The Argument for Less Length Being Sufficient
However, there is a significant body of data indicating that 15 mm or even less graft in a tunnel is acceptable. A recent study by Zantop et al in goats using Endobutton fixation showed no difference in load to failure between 15 mm and 25 mm of graft in the tunnel.11 A study by Yamazaki et al in dogs using whipstitch cortical screw post fixation showed no difference between 5 mm and 15 mm.12 Equally persuasive in favor of shorter lengths being acceptable is the clinical experience of a number of experienced surgeons such as Rosenberg and Cooley2 and Paulos13 who have had excellent results using 15-mm grafts. We have also used 15 mm as a minimum without a graft failure.
2 Is the Graft Long Enough to Allow Direct Tibial Fixation or Only Indirect?
Direct fixation includes all interference screw and interference screw–based techniques such as Intrafix and techniques that rely on direct friction with the graft, such as the WasherLoc. Indirect fixation uses a fabric interface with the graft such as the whipstitch post technique or Fastlok. As seen in Table 17-1, use of the Gr as well as the ST is necessary to be certain of a long-enough graft to ensure the use of direct fixation techniques.
3 Is the Gracilis Sacrificed?
The Gracilis Is not Really a Hamstring
One argument against the 2ST/2Gr graft is that it disables not one but two hamstring muscles because the Gr is also harvested in addition to the ST. However, the Gr is not really a hamstring. Gray’s Anatomy14 lists only three hamstring muscles: the biceps femoris, semimembranosus, and ST. All are innervated by the sciatic nerve; all flex the knee. The Gr is not listed as a hamstring. Rather, the Gr is listed with the adductors longus, brevis, and magnus as “medial femoral muscles.” All of these muscles, including the Gr, are innervated by the obturator nerve. The gracilis’ action is listed as “adducts the thigh.” Thus, the loss of the Gr is not the loss of a second hamstring. Rather, it is the loss of an accessory adductor, much as the loss of the ST is the loss of an accessory hamstring.
What Is Lost by Harvesting the Gracilis in Addition to the Semitendinosus?
Chapter 67 reviews strength after hamstring harvest. Hamstring strength can be restored in virtually 100% of patients in our experience. Specific testing has noted a small decrease in peak flexion torque at high flexion angles and decreased tibial internal rotation strength in flexion; however, no clinical deficit has ever been reported in function as a result of the addition of Gr harvest relative to ST alone. On theoretical grounds, some have avoided Gr harvest in sprinters and soccer players.15 However, performance deficits or subjective complaints have not been reported in this group. Anecdotally, we have performed bilateral 2ST/2Gr in a professional soccer player with excellent subsequent performance.
4 How Strong Is the Graft?
Using the data from the classic study of Noyes et al16 in which the ST was 70% of the strength of the native ACL and the Gr was 49% of the strength, extrapolated hamstring graft strengths can be estimated. The 4ST would be 280%, the 2ST/2Gr would be 238%, the 3ST would be 210%, and the 2ST would be 140%. The 4ST and 2ST/2Gr have produced very high stability rates in clinical series.2–7 The 2ST has been associated with low rates, although this may well be largely due to the outmoded fixation that was used when those studies were done.17–19 Regardless of whether this is true, few surgeons today are comfortable with only a 2ST graft. The 3ST graft has produced high stability in some20 but not all21 series. This mixed clinical performance and the lower strength of the graft coupled with the increased complexity of using an odd-stranded graft in the femur has resulted in this graft being seldom used.
5 Is the Graft Double-Bundle Compatible?
Yasuda et al22 have reported a six-strand, double-bundle technique with 3ST/3Gr, as described in Chapter 22. Christel uses a 2ST anteromedial (AM) bundle and either a 2Gr or 3Gr (if the Gr is small) posterolateral (PL) bundle, as described in Chapter 23. Zhao et al have reported a 4ST AM and 4Gr PL bundle eight-strand technique.23
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree